Four-Part Proximal Humeral Fractures: ORIF
Erwin Aschauer
Herbert Resch
E. Aschauer: General Hospital Salzburg, Department for Trauma and Sport Traumatology, Salzburg, Austria.
H. Resch: General Hospital Salzburg, Department for Trauma and Sport Traumatology, Salzburg, Austria.
PATHOLOGY
Risk Factors
Fractures of the proximal humerus are very frequent injuries. About 4% of all fractures occur in this region,14 and women are affected twice as frequently as men.31 In comparison with proximal femoral fractures, the frequency is about 70% to 100%.14,31 “Most of these fractures result from a fall on the outstretched arm in older people.” These patients have osteoporotic bones, which are very fragile. Poor bone quality often leads to complex fractures, so it is not surprising that the severity of the injuries increases with age.7 Court-Brown et al. reported in an epidemiological study that no less than 70% of the patients having three- or four-part fractures are older than 60 years, and more than 50% are older than 70 years.
Because free range of motion is so important for shoulder function during the different activities of everyday life, proper treatment of these difficult fractures requires careful consideration of the principles of soft-tissue treatment, as well as the principles of fracture treatment.
In severely displaced proximal humerus fractures, parts of the periosteum are disrupted, and, in some cases, there is no more connection between the fragments at all. Together with the periosteum, the blood vessels are destroyed, creating a risk of avascular necrosis of fragments, especially of the humeral head.24 In the past, this was the reason to do a prosthesis in acutely displaced humeral head fractures; nowadays, we have acquired better knowledge of the blood supply of the humeral head and have new techniques at our disposal2,12,13,20,22,27, 28 and 29 to preserve periosteum and blood vessels during the operation.5,9,25,27,33 Moreover, we believe that a secondarily implanted prosthesis, because of humeral head necrosis after primary osteosynthesis, has no worse outcome than that of prosthesis placed for an acute fracture.
Mechanisms of Injury
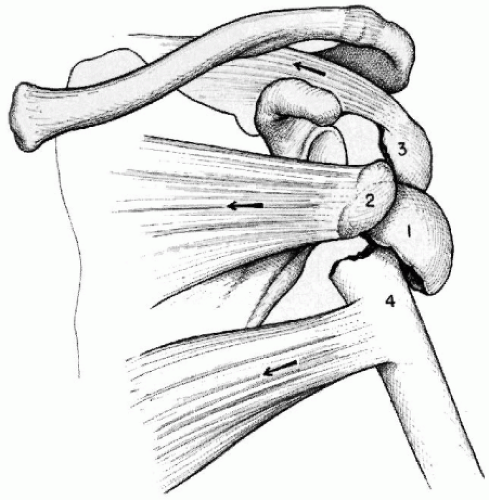
Proximal humerus fractures usually result from falling on the outstretched arm or a direct blow to the shoulder. The fracture pattern is determined by the interaction of the external forces applied to the arm and the internal forces of the intrinsic shoulder muscles. The upper arm is connected to the body by the thoracohumeral muscle (pectoralis major, latissimus dorsi) and the scapulohumeral muscles (deltoid, supraspinatus, infraspinatus, subscapularis, teres major,
teres minor, biceps, and triceps). All of these muscles have an influence on the mechanism of injury and fracture type and can cause secondary displacement as well. The resulting force vector on the cuff to the intact humeral head would be directed downward and medially. The pectoralis major muscles, teres major and latissimus dorsi, pull the humeral shaft medially into internal rotation. The deltoid, biceps, and triceps muscles raise the arm against gravity (Fig. 14-1). Normally, the effects of the muscles on the different fragments after the fracture can be first seen some days after the injury. The reason is loss of muscle tension during early posttraumatic period. Knowledge of these facts is important to choose the right kind of treatment, conservative or operative, and, when operative, which implant.
teres minor, biceps, and triceps). All of these muscles have an influence on the mechanism of injury and fracture type and can cause secondary displacement as well. The resulting force vector on the cuff to the intact humeral head would be directed downward and medially. The pectoralis major muscles, teres major and latissimus dorsi, pull the humeral shaft medially into internal rotation. The deltoid, biceps, and triceps muscles raise the arm against gravity (Fig. 14-1). Normally, the effects of the muscles on the different fragments after the fracture can be first seen some days after the injury. The reason is loss of muscle tension during early posttraumatic period. Knowledge of these facts is important to choose the right kind of treatment, conservative or operative, and, when operative, which implant.
Furthermore, position and fragment distances can indicate whether there are any periosteal connections. The muscles are usually fully tensioned at the moment of the fall, causing a fracture. Due to the muscle pull, the greater and lesser tuberosity will be displaced in three- and four-part fractures. Later, no more change of this position is possible, only the angulation of the shaft fragment will look different on the first x-ray. The tuberosities remain the same as they were at the moment of the accident.
Based on the principle of mechanisms of fractures you can distinguish between two kinds of fractures: avulsion fractures and impacted fractures (valgus fractures). Avulsion fractures are caused by the interaction of fall energy and the effects of the rotator cuff muscles on the humeral head. The main fracture line can be found along the surgical neck, where there is a weak transitional zone between cortical and cancellous bone. If there are no more fracture lines, a two-part fracture will result. Additional displace fracture planes features of tuberosities lead to three-part fractures. The rotator cuff does not lose its effect immediately after the fracture, which leads to typical displacements. In case of subcapital two-fragment fractures, a varus position will take place (Fig. 14-2A). Subcapital fracture and fracture of the lesser tuberosity lead to a mixed varus and externally rotated position of the humeral head (Fig. 14-2B). Fracture of the greater tuberosity, in addition to a subcapital fracture, leads to varus and internal rotation (Fig. 14-2C). The strength of the rotator cuff very often tears the periosteum, so these fractures are unstable and have a tendency to medially displace the shaft fragment. Because of the destroyed periosteum, the greater tuberosity goes up into the subacromial space; the lesser tuberosity mostly will be displaced medially. In four-part fractures, both tuberosities are broken over and the rotator cuff has no effect on the head anymore.
In impacted fractures, the axial force of the glenoid to the articular part of the humeral head pushes the head fragment down onto the metaphysis. The tuberosities break out and are pushed aside laterally and to the front. If the impaction of the head fragment is not too severe, the lesser tuberosity can remain on the head, resulting in a three-part valgus fracture. In most cases, however, both tuberosities are fractured (four-part valgus fracture), and there are two main fracture lines: one along the surgical neck and a second along the anatomic neck. The tuberosities remain in periosteal connection with the shaft fragment.
Avulsion Fractures
Surgical Neck Fractures
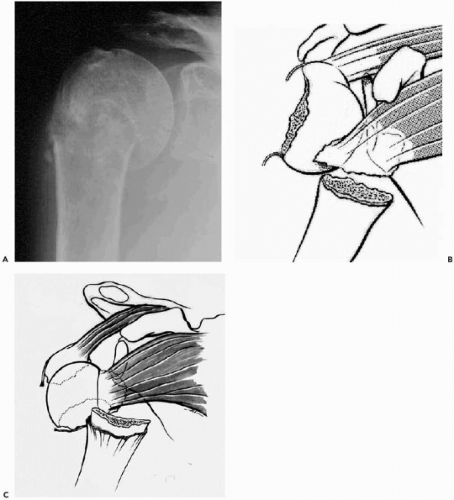
Often varus displacement of the head fragment takes place only days after injury. Depending on the condition of the periosteum on the medial side, the head fragment is displaced medially in different degrees (sometimes after a few days). In many cases, the head is in an excentric position, that is, situated dorsally to the axis of the humeral shaft. On an anteroposterior (AP) x-ray, this excentric malposition leads to an overlapping of anatomic structures and looks like impaction. An additional axial or trans-scapular view can avoid this misinterpretation (Fig. 14-3, A and B). It is typical to see this phenomenon only a few days after the injury, when the tension of the muscles comes back again.
Surgical Neck Fracture and Fracture of the Greater Tuberosity
Because of the fracture of the greater tuberosity, the supraspinatus and infraspinatus muscle no longer effect
the humeral head. The only remaining muscle moving the humeral head is the subscapularis, which rotates the head internally without any resistance. The extent of the rotation depends on the condition of the periosteum between the head and the shaft. When all periosteal connections are disrupted, the head is rotated internally to the maximal extent and looks like a ball—perfectly circular—on the AP x-ray. Corresponding to the lack of any connections, the humeral shaft is displaced medially to the head, caused by the pull of the pectoralis major. The greater tuberosity also has no more connection to the shaft and is displaced upward and dorsally by the pull of supraspinatus and infraspinatus.
the humeral head. The only remaining muscle moving the humeral head is the subscapularis, which rotates the head internally without any resistance. The extent of the rotation depends on the condition of the periosteum between the head and the shaft. When all periosteal connections are disrupted, the head is rotated internally to the maximal extent and looks like a ball—perfectly circular—on the AP x-ray. Corresponding to the lack of any connections, the humeral shaft is displaced medially to the head, caused by the pull of the pectoralis major. The greater tuberosity also has no more connection to the shaft and is displaced upward and dorsally by the pull of supraspinatus and infraspinatus.
Surgical Neck Fracture and Fracture of the Lesser Tuberosity
After fracture of the lesser tuberosity, the subscapulary muscle has no more effect on the humeral head. The supraspinatus and infraspinatus pull the head in varus and external rotation. A completely destroyed periosteum leads to grotesque rotations of the head, and the pectoralis major displaces the shaft medially.
Impacted Valgus Fractures
Four-Part Fracture
The impact of the glenoid pushes the humeral head down toward the metaphysis, breaks the tuberosities out, and pushes them aside. The tuberosities remain at the right height, and their periosteal connections are not torn. The rotator cuff has no effect on the humeral head at all. The only connection between the head and shaft may be on the medial side in the form of remaining periosteum (so-called hinge periosteum). This periosteum is very important; it makes reduction easier and maintains the blood supply of the head. This periosteum is always intact if no lateral displacement occurs between the articular head fragment and the shaft. Biomechanical studies on cadavers have shown that the periosteum can bear 6 mm of lateral displacement and 9 mm of medial displacement26,29 (Fig. 14-4, A and B). Normally, the impaction is not exactly axial; instead, a simultaneous tilt of the head fragment to the dorsal takes place, so rotation is possible. This all creates a distorted picture on the x-rays, so it is not easy to find the correct diagnosis. The dorsal tilt, however, ensures that the dorsomedial periosteum remains, even with lateral displacement.
Concomitant Injuries
The mechanism leading to a fracture of the proximal humerus, in most cases, is a fall on the outstretched arm from standing—or even less—height, particularly with older people. The injury only needs to be moderate in degree because osteoporosis is usually present. In this group of patients, proximal humeral fractures commonly occur as single injuries without any associated fractures.
With younger people, the severity of injury is usually more serious. The resulting fractures are often more complicated, more displaced, and sometimes dislocated. In addition, there is more soft-tissue damage, such as contusions, disruptions of tendons and muscles, or even lesions of nerves and blood vessels. Many fractures of the proximal humerus occur in patients with multiple traumas. In those cases, the upper arm injury is not the main problem, and attention is focused on more life-threatening problems. It is not unusual, howevr, to later detect the fracture by chance on a chest x-ray.
Electric shocks or convulsive episodes can cause shoulder
dislocations and fracture dislocations. The dislocations can be both anterior and posterior and are easily overlooked. Another ethiology for fractures of the proximal humerus is metastatic disease. In weakened bones, fractures can occur without trauma while performing trivial daily activities.
dislocations and fracture dislocations. The dislocations can be both anterior and posterior and are easily overlooked. Another ethiology for fractures of the proximal humerus is metastatic disease. In weakened bones, fractures can occur without trauma while performing trivial daily activities.
Dislocation Versus Impacted Valgus
In contrast to impacted valgus fractures, severely displaced humeral head fractures (“true” four-part fractures) have a worse prognosis because there are only very few or no softtissue links at all (i.e., destroyed hinge periosteum).
The extreme variant of this fracture type is the four-part fracture dislocation. The head fragment is displaced far away from the shaft fragment and reduction—open as well as percutaneous—is very difficult to obtain. The risk of avascular necrosis of the head fragment is high, so prosthetic replacement is the treatment of choice in most cases. With younger people, however, an attempt—whether closed or open—should be made to reduce the fracture to obtain the original anatomy of the humeral head. If a necrosis does develop, a good functional outcome can be expected with secondary prosthetic replacement because the tuberosities are healed in good position.
In some elderly patients, when the condition of the patient does not allow the implantation of a prosthesis, percutaneous treatment can be performed under regional anesthesia.
Head Splits
Impression and head-splitting fractures lead to a prosthesis implant in a high percentage of cases. Treatment of the impression of the articular surface of the humeral head depends on the size of the defect. Small defects up to 20% of the head’s surface can be managed with reduction and immobilization of the arm. One can manage larger defects, especially those located in the anterior head (Hill-Sachs defects), by transferring the lesser tuberosity into the defect.
Head splits are usually associated with fractures of the tuberosities or the surgical neck. If the patient has a good bone stock, open reduction and internal fixation can be attempted, but it is a difficult procedure with a high rate of secondary redisplacement. With younger people, however, it is worth trying.
SPECIAL TESTS
Accurate Radiographs
Accurately performed x-rays are essential for visualizing the fracture type, making the correct diagnosis, and planning treatment. The Neer trauma series includes a true AP, an axillary, and an additional lateral trans-scapular view.24 To perform a true AP view in the scapular plane, the contralateral shoulder has to be rotated out approximately 40 degrees so that the glenoid surface comes into the sagittal plane (a true AP view). The lateral trans-scapular view, also called tangential or Y-view is performed in many hospitals as second view but does not enable correct fracture assessment, particularly regarding lesser tuberosity displacement.35
It can be done in either a sitting, standing, or prone position without removing the arm from the sling.
It can be done in either a sitting, standing, or prone position without removing the arm from the sling.
A good axillary view is essential. No other view can show the situation on the lesser tuberosity in a comparably exact manner. Furthermore, it allows the interpretation of the axis and the relation between the head and shaft as well as between the head and glenoid. The x-ray is performed on the sitting patient with the arm abducted. Being careful in abducting and resting the patient’s arm, it is possible to do this in almost all cases. An alternative technique is the Velpeau axillary view. It is not necessary to remove the arm from an already applicated sling, and the arm can remain close to the chest. The patient is seated and tilted backward in a 45-degree angle over the table. The x-ray plate lies below on the table, and the tube comes from above in a vertical direction. Howerver, incorrect or oblique views will misrepresent the fracture and create confusion.
Conclusions from Radiographs to Periosteum Condition
If there is no displacement in the horizontal plane on either the AP or axillary view, then the periosteum on the medial side is intact. In subcapital fractures with misrepresented impaction (AP view) but true anterior angulation (axillary view), the periosteum on the medial and in the front is disrupted. In these cases, there is a high risk of secondary displacement of the shaft because of the pull of major pectoralis muscle medially. If there is such a displacement on the primary x-ray, you can expect an increase in the following days.
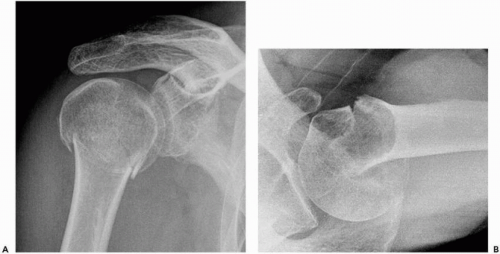
Lateral displacement of the greater tuberosity without change of height (typical of impacted fractures) leaves the periosteal connection between shaft and greater tuberosity intact. Depending on the degree of lateral displacement, the periosteum is stripped some distance from the shaft (“long rein”), and the tuberosity follows the posterior pull of the infraspinatus. After the reduction of the head fragment, the greater tuberosity will come close to the shaft again (AP view) but will remain in a posterior position. If there is proximal (superior) displacement of the greater tuberosity, periosteal connections between shaft and tuberosity are destroyed, and the tuberosity follows the pull of the rotator cuff under the acromion (typical in avulsion fractures) (Fig. 14-5).
Medial displacement of the lesser tuberosity is possible in cases of the disruption of the periosteum between shaft and tuberosity (avulsion fractures). In impacted fractures the periosteum remains intact, and the apparent medial displacement of the lesser tuberosity on the axillary view is caused by impaction of the head fragment underneath the tuberosity.
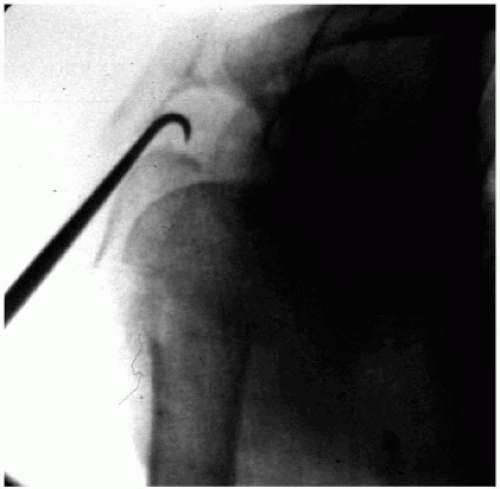
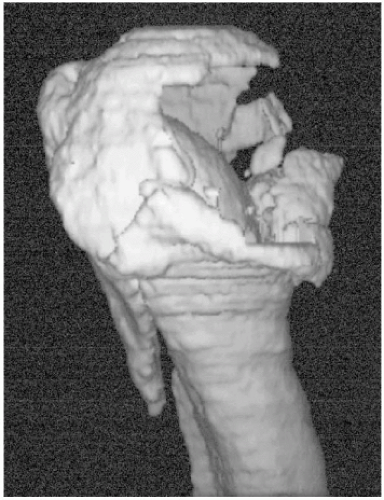
CT scans
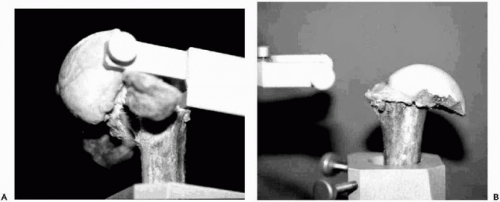
If good radiographs are available, an additional CT scan
does not usually provide any further useful information.37 Sometimes a CT scan is helpful in preoperative planning, especially for percutaneous treatment. The nature of the fracture is best demonstrated with three-dimensionally CT reconstruction.29 It is useful to understand the fracture type, the relation between fragments, and the conclusions concerning soft-tissue connections. Also, evaluating the amount of articular involvement with a head-splitting or impression fracture is possible (Fig. 14-6).
does not usually provide any further useful information.37 Sometimes a CT scan is helpful in preoperative planning, especially for percutaneous treatment. The nature of the fracture is best demonstrated with three-dimensionally CT reconstruction.29 It is useful to understand the fracture type, the relation between fragments, and the conclusions concerning soft-tissue connections. Also, evaluating the amount of articular involvement with a head-splitting or impression fracture is possible (Fig. 14-6).
MRI
Magnetic resonance imaging is inferior to CT scan in visualizing bony structures. It may be helpful in diagnosing concomitant injuries of muscles, tendons, or intra-articular structures. An attempt to visualize the blood supply of the head by using gadolinium has not been successful so far.
Other Studies
Conventional tomography was used to verify nonunions in the past, but CT is now the initial procedure of choice. With the help of an image intensifier it is possible to perform a dynamic examination to check the stability of fractures and implanted material.
NONOPERATIVE TREATMENT
Indications
About 85% of all fractures of the proximal humerus are not displaced or are minimally displaced, so good results after conservative treatment can be expected.9 Displacement, instability, or concomitant dislocation requires an operative treatment to achieve good shoulder function. The shoulder, with its large capsule, allows a wide range of motion,30 so it can compensate for some displacement between the head and shaft fragment. Up to 30-degree angulation in the lateral plane and horizontal displacement, and up to half of the width of the shaft, may be tolerated. However, displacement tuberosity, in relation to the head fragment, that is more than 3 mm should be treated operatively. Often you can see the tuberosities in place, but the head fragment depressed. Impression fractures of the head and head-splitting fractures may yield poor results after conservative treatment.
Closed reduction of displaced four-part fractures is not a realistic option because the muscles of the rotator cuff that pull away the fragments will render such attempts impossible.
In some cases, conservative treatment may be preferred because the patient is not able to tolerate an operation or the patient does not agree to the operation.
Results in Literature
In literature, many different methods of treatment of proximal humerus fractures are reported, and much controversy exists. Fortunately, most fractures are not displaced or are minimally displaced, so, in general, a satisfying result can be expected. Four-part fractures are mostly displaced, and most authors agree that conservative treatment of these cases leads to poor or bad results.21,24,39,40 However, controversy exists regarding the best kind of operative treatment of displaced four-part fractures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree