Transepiphyseal Resection and Intercalary Reconstruction
D. Luis Muscolo
Miguel A. Ayerza
Luis A. Aponte-Tinao
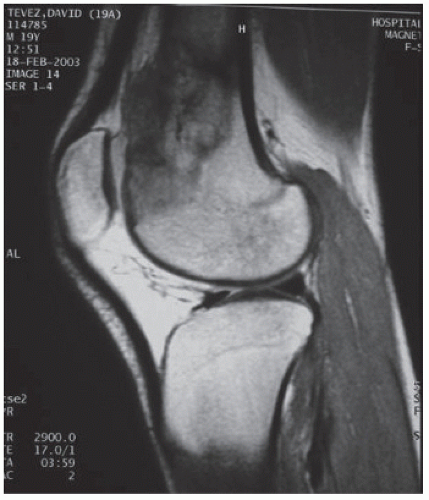
Patients are selected for this procedure according to the following criteria: (a) intrachemotherapy tumor progression, (b) tumor growth toward the epiphysis, and (c) amount of epiphysis to be preserved in order to allow fixation of the osteotomy junction. Prechemotherapy and postchemotherapy MRI studies are compared to evaluate tumor response. Tumors with no clinical or MRI evidence of progression during chemotherapy are considered potential candidates for transepiphyseal resections (Figs. 21.1 and 21.2).
INDICATIONS
Tumors growing in the metaphyseal area with no or partial compromise of the epiphysis
A residual epiphysis of >1 cm should be obtained in order to allow fixation of the osteotomy junction and safe oncologic margins.
Tumors with no evidence of progression clinically or on magnetic resonance imaging (MRI) studies during chemotherapy
This technique is designed in order to resect the tumor, preserving the patient’s own articular cartilage, cruciate, and collateral ligaments and without altering the normal joint anatomy.
CONTRAINDICATIONS
Patients in whom preoperative imaging studies demonstrate evidence of epiphyseal compromise of the tumor
Intrachemotherapy tumor progression
PREOPERATIVE PREPARATION
Patients are usually treated with chemotherapy and, after the induction period, definitive surgery of the primary lesion is performed. Magnetic resonance images are done with a 1.5-T Magnetom Vision unit (Siemens, Erlangen, Germany) at the time of the diagnosis and after chemotherapy in order to evaluate tumor response. The whole limb is evaluated using a body coil. In order to determine epiphyseal tumor spread and its relation to the articular cartilage, images are obtained using an additional knee coil. These images are reviewed on paired longitudinal T1-weighted and short tau inversion recovery images. The extent of the epiphyseal involvement is calculated with coronal, sagittal, and axial images defining the end of the tumor as the point in which marrow signal intensity changed from normal to abnormal (1,2,3,4,5,6,7). All scans are performed by the same radiologist.
TECHNIQUE
All operations are performed in a clean-air enclosure with vertical airflow and usually with spinal anesthesia. The patient is placed on the operating table in the supine position. A sandbag is placed under the ipsilateral buttock. A long midline incision is made beginning in the midthigh and a medial parapatellar arthrotomy is performed that enables a wide exposure of the distal femur and the knee joint. The biopsy tract is left in continuity with the specimen (Fig. 21.3). The distal femur is approached via the interval between the rectus femoris and vastus medialis. If there is an extraosseous component, a cuff of normal muscle must be excised. Proximal femoral osteotomy is performed at the appropriate location as determined by the preoperative imaging studies. All remaining soft tissues at the level of transaction are cleared. The osteotomy is performed after the posterior and medial structures have been protected and retracted and perpendicular to the long axis of the femur. Following the osteotomy, the distal femur is pulled forward to expose the soft tissue attachments of the popliteal space. The popliteal artery is mobilized, and the geniculate vessels are ligated and transected. The gastrocnemius is released and the posterior capsule is opened. The cruciates and collateral ligaments are identified and remain intact attached to the epiphysis that is saved. The next step is to mark the intraepiphyseal cut (Fig. 21.4). The osteotomy is planned 1 to 2 cm from the lower edge of the tumor growth, defined as the point at which marrow signal intensity changed from abnormal to normal. At the time of surgery, measurements obtained with preoperative MRI are correlated with anatomical landmarks: the epicondyles, the intercondylar notch roof, and the articular cartilage limits in the femur. Following the osteotomy the distal femur is passed off the operative field (Fig. 21.5). After resection of the tumor, insertion of an allograft segment tailored to fit the bone defect is performed. After the donor bone is thawed in a warm solution, it is cut to the proper length (Fig. 21.6). The intraepiphyseal osteotomy is temporarily secured with threaded Kirschner wires that are inserted through the distal part of both condyles and into the allograft. Then the osteotomy is stabilized by internal fixation with cancellous screws compressing the metaphyseal bone (Figs. 21.7 and 21.8). Before the proximal osteotomy is stabilized, the posterior capsule is repaired suturing autologous capsular tissues with capsular tissues provided by the allograft. The diaphyseal osteotomy
is stabilized by internal fixation with an anterior short plate, and to minimize the risk of fracture an additional lateral condylar buttress plate is placed to cover the entire length of the allograft (Figs. 21.9



is stabilized by internal fixation with an anterior short plate, and to minimize the risk of fracture an additional lateral condylar buttress plate is placed to cover the entire length of the allograft (Figs. 21.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree