Total Elbow Replacement for Acute Fracture and Distal Humeral Nonunion: Triceps Attachment Maintained
Bernard F. Morrey
Joaquin Sanchez-Sotelo
Mark Morrey
INTRODUCTION
Management of acute fracture and nonunions of the distal humeral by joint replacement has been an effective treatment option for several decades (1). The ability to salvage otherwise unsalvageable pathologic conditions has been quite gratifying. As with any joint replacement, however, depending on the activity level of the patient over time, these implants will demonstrate mechanical failure, particularly loosening and wear of the articulation. The patients with distal humeral nonunion are particularly vulnerable to this due to the frequency with which there is a deformity associated with the nonunion. This causes excessive stress on the fixation and articulation. Because the nonunion is the most challenging procedure, due to deformity and scarring, this pathology is illustrated in this chapter.
 FIGURE 37-1 Comminuted fracture in osteoporotic bone in the older patient is an ideal indication for joint replacement as the initial and usually final treatment. |
INDICATIONS
Older patients (>65 years?):
Acute fracture unable to be reliably fixed due to the degree of communition or extent of osteoporosis (Fig. 37-1)
Nonunion in patients in whom osteosynthesis is not an option due to inadequacy of the articular surface or articular osseous support or severe osteoporosis or deformity (Fig. 37-2)
Failure of osteosynthesis
PREOPERATIVE PLANNING
The key consideration of preoperative planning for the acute fracture is to observe the level of the fracture. Fractures proximal to the olecranon fossa will usually best be managed with a long flanged implant. Type 1 compound fractures may be dealt with at the time of injury.
For type 2 and 3 injuries, the wound should be managed first, and replaced when it is deemed safe from the soft tissue perspective. For the nonunion, note the degree of deformity and location of previous skin incisions. The most important point in the history is whether or not there was any evidence of infection from the previous surgery. Mayo’s experience reveals that on the average, patients undergoing joint replacement for distal humeral nonunions have had two previous surgical procedures. Thus, the possibility of infection is a real one and always must be considered as a possible cause of the nonunion. Hence, assessment of inflammatory markers and joint aspiration are performed prior to surgery. Severe deformity, as with knee replacement, may require longer stems to avoid loosening. It is, therefore, important to have an array of prosthetic options available for these patients.
The status of the ulnar nerve is also important to document. If translocated and without symptoms, the nerve simply needs to be identified at the time of surgery. If the patient is symptomatic, then decompression of the nerve is carried out. This can take almost as long as the joint replacement in some instances and magnification is often employed.
SURGICAL TECHNIQUE
Patient Positioning
As with all joint replacements, the patient is placed on the table in a supine position, and the arm is brought across the chest. The compound wound is incorporated into the incision or previous skin incisions are honored if at all possible. For those with a nonunion, if there is gross deformity, we employ the landmarks of the subcutaneous border of the ulna distally and the midportion of the humerus proximally in order to ensure that the final incision is straight once the deformity is corrected.
Exposure
After making the skin incision, the dissection carries proximally through the fascia through the subcutaneous tissue, exposing the triceps fascia.
The ulnar nerve is identified and protected if it is asymptomatic. This is best done more proximally at the medial aspect of the triceps prior to its anterior reorientation. If the ulnar nerve is symptomatic, then it is dissected free and protected for the remainder of the procedure.
Note: This step can take a significant period of time if there has been previous surgery, and typically, magnification is required.
Exposure of the Distal Humerus
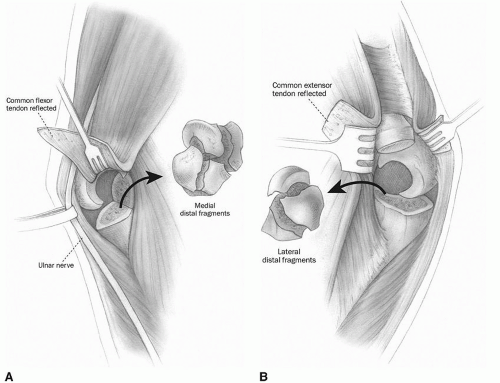
The triceps is elevated from the posterior aspect of the humerus. This is usually not extremely difficult particularly if the ulnar nerve has been isolated. Kocher’s interval is entered distally and the dissection proceeds proximally to release the extensor muscle mass from the lateral epicondyle. The flexors are dissected from the medial epicondyle. The anterior and posterior capsules are completely excised. For acute fractures, this is relatively easy; for nonunion, scarring can make this exposure more difficult. The fracture fragments or nonunion is isolated and the loose fragments excised (Fig. 37-3). The distal humerus is then exposed by reflecting the triceps and mobilizing the ulna either medially or laterally (Fig. 37-4).
Note: In most nonunions, significant contracture and angular deformity are common features that result in soft tissue imbalance, and thus, aggressive release of the bone and soft tissue is essential.
The remainder of the procedure will be that of managing the nonunion. Treatment for the acute fracture is identical except there is no need to manage deformity.
Distal Humeral Preparation
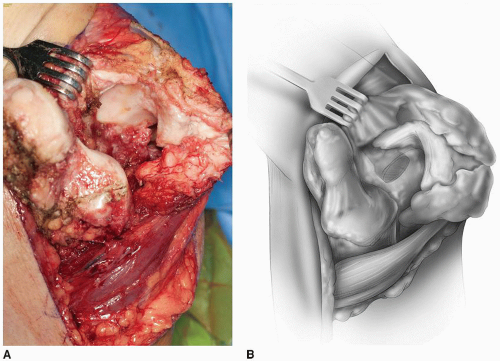
The nature of the pathology is identified. The distal humerus is resected to the level necessary to overcome any excessive flexion contracture (Fig. 37-5).
Note: By leaving the triceps attachment on the ulna and positioning the ulnar articulation over the resected humerus, a good estimate of the adequacy of the release and resection can be made (Fig. 37-6).
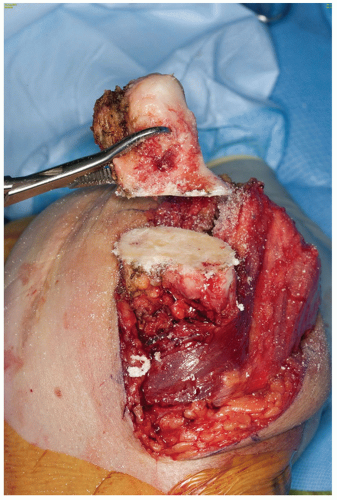 FIGURE 37-5 The contracted soft tissue and deformity requires resection of the proximal 4 cm of distal humerus. Note the enlarged dimension of the humeral shaft at the site of resection. |
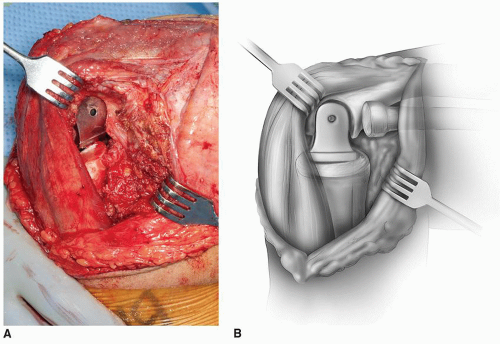
The humerus is then subluxed, either to the medial or to the lateral side of the triceps, and is prepared. Care should be taken to enter the canal with a burr through the sclerosis of the nonunion so as not to violate the cortex. Serial rasping is performed until the proper fit has been determined (Fig. 37-7). A trial implant is then inserted, and the elbow is reduced with the intact ulna in order to provide some insight as to whether or not tension has been restored to determine whether or not more resection is necessary (Fig. 37-8).
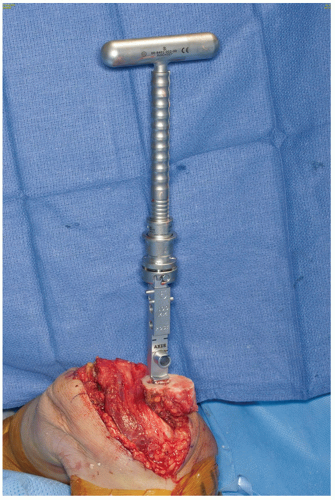 FIGURE 37-7 The forearm has been displaced medially. The humerus emerges from the lateral margin of the triceps. It is readily prepared for the introduction of any elbow implant system. |
Ulnar Preparation
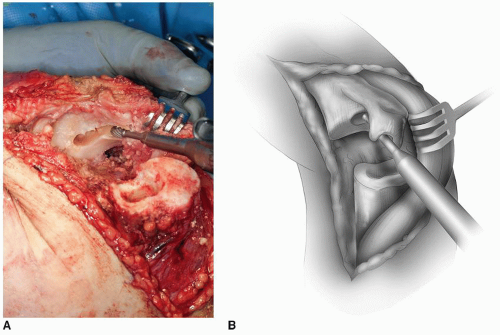
By rotating the ulna and releasing a portion of the medial attachment of the triceps, the base of the coronoid can be identified and is entered with a high-speed burr (Fig. 37-9). We then notch the olecranon such that the flexible reamers can be directed down the canal. The ulna is then prepared with serial reaming and rasping. The final rasp is inserted to the proper depth that is facilitated by removing the tip of the olecranon (Fig. 37-10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree