Tibiotalocalcaneal and Ankle Arthrodesis Using Ring External Fixation
Justin Orr
Mark E. Easley
INTRODUCTION
Current recommendations for primary and revision tibiotalar (ankle) joint arthrodesis favor internal compression techniques using screw and/or plate internal fixation, with satisfactory outcomes being reported for most patients. Similarly, when there is concomitant subtalar joint arthritis, current recommendations for primary and revision tibiotalocalcaneal (TTC) arthrodesis favor screw and/or plate internal fixation or retrograde TTC intramedullary nail internal fixation. Recently, comparable union rates and results of primary and revision tibiotalar arthrodeses have been reported using ring external fixation techniques (1, 2, 3, 4, 5 and 6). In select patients, ankle and TTC arthrodesis with internal fixation may be limited or even contraindicated given insufficient bone stock to adequately support implants, an abundance of avascular bone, a history of deep infection or osteomyelitis, in cases of prior failed total ankle replacement with significant osseous defects, or in cases when previous ankle or TTC arthrodesis has failed (4,6, 7 and 8). Ring external fixation may facilitate clinically acceptable limb salvage in these complex cases. The following review primarily discusses the indications/contraindications, surgical technique, and postoperative management for ankle arthrodesis using ring external fixation; however, these principles apply equally to TTC arthrodesis using ring external fixation. A description of the modifications in surgical technique necessary for TTC arthrodesis using ring external fixation in cases where subtalar joint arthritis is present is described as well.
Many advances have been made in recent years for management of advanced ankle arthritis recalcitrant to nonoperative treatment. Although ankle arthroscopy, distraction arthroplasty, fresh allograft shell reconstruction, supramalleolar osteotomy, and total ankle replacement have shown promise in select cases of advanced ankle arthritis, ankle arthrodesis remains the standard for surgical management. Results of ankle arthrodesis using internal fixation for stability and compression are consistently favorable, and internal fixation for ankle arthrodesis is the technique of choice in most cases. However, surgeons occasionally encounter cases of ankle arthritis with or without concomitant subtalar joint arthritis that should be managed with arthrodesis but does not lend itself well to internal fixation. External fixation represents an attractive alternative in such situations (9). A recent cadaveric biomechanical study demonstrated equal bending stiffness and a twofold increase in torsional stiffness using a ring external fixator for TTC arthrodesis compared to retrograde intramedullary nailing, providing biomechanical support for ring external fixation (10).
Although external fixation for problems of the foot and ankle is not universally taught in orthopedic training programs, it has been used routinely for numerous disorders of the foot and ankle in select medical centers worldwide. Gradually, the number of surgeons applying the techniques developed in these institutions for the surgical management of foot and ankle disorders is increasing, either by necessity or by recognition of the advantages of these methods in select foot and ankle problems. While results of ankle and TTC arthrodesis using external fixation are not as widely published as those using internal fixation, the results of ankle and TTC arthrodesis using external fixation, even in revision surgery, are favorable.
INDICATIONS AND CONTRAINDICATIONS
The most common indication for ankle arthrodesis is severe, destructive arthritis that fails nonoperative management, most commonly posttraumatic in origin. Less frequently, ankle arthritis is caused by primary or inflammatory arthropathies. Currently, severe ankle arthritis can be managed with total ankle replacement or fresh allograft reconstruction, but ankle arthrodesis remains the gold standard. Regardless of the method of fixation, ankle arthrodesis is contraindicated in patients with peripheral vascular disease until adequate circulation for healing can be reestablished.
Absolute indications for arthrodesis include ankle arthritis associated with neuropathy, extensive avascular necrosis of the talus and/or distal tibia, severe coronal or sagittal plane deformity, and nonreconstructable ankle ligament insufficiency. That is to say, in such cases, total ankle replacement is generally contraindicated. Joint-sparing procedures may be favored when ankle arthritis is associated with ipsilateral hindfoot arthritis or a contralateral ankle or TTC arthrodesis.
Typically, ankle arthrodesis can be effectively performed with internal fixation. External fixation may confer advantages over internal fixation in several situations. Specifically, external fixation for ankle arthrodesis may be considered with the following:
History of septic arthrosis or osteomyelitis
A compromised soft tissue envelope about the ankle
Inadequate bone stock at the arthrodesis site to support internal fixation limited to the tibia and talus
A leg length discrepancy that is inadequately treated with a shoe modification, requiring potential distraction osteogenesis for limb lengthening
Failed prior ankle arthrodesis using internal fixation
Neuropathic joint arthropathy
Anticipated patient noncompliance with postoperative weight-bearing restrictions.
A recent series by Easley et al. reported an 85% fusion rate with use of ring external fixation for revision and rerevision ankle arthrodesis and noted that ring external fixation is a valuable alternative to internal fixation in complex cases where internal fixation is limited or contraindicated. The authors of that study selected history of infection at the nonunion site or patient noncompliance with weight-bearing restrictions as absolute indications for ring external fixation in cases of revision ankle fusion. While contraindications to ankle arthrodesis are few, relative contraindications to external fixation for ankle arthrodesis are patients with indwelling total joint arthroplasties, as potential pin tract infections may lead to periprosthetic infection, and sensory neuropathy of the contralateral leg, as the external fixator may cause wounds to the contralateral lower extremity unbeknownst to the patient.
PREOPERATIVE PLANNING
Patient history, clinical evaluation, and routine ankle radiographs establish the diagnosis of symptomatic ankle arthritis. On examination, particular attention should be paid to associated malalignment deformities and/or presence of ankle equinus contracture, as adjunctive deformity corrective procedures, or Achilles tendon lengthening may be necessary. Weight-bearing radiographs of the ankle usually confirm the diagnosis. The soft tissue envelope about the ankle and the vascular status must be evaluated. Poor soft tissues about the ankle, often secondary to trauma and/or prior surgery, typically necessitate a less invasive exposure for joint preparation. Compromised perfusion of the extremity should prompt vascular consultation to optimize the chance for union and proper soft tissue healing.
Routine weight-bearing AP, mortise, and lateral ankle radiographs generally suffice, but if there is any suspicion on clinical evaluation for limb malalignment or foot pathology, then mechanical axis, hip and knee, and foot radiographs should also be evaluated. Computed tomography (CT) and magnetic resonance imaging (MRI) are not routinely required. In select cases, CT may help identify hindfoot arthritis/deformity if plain radiographs of the foot and ankle fail to adequately reveal these clinical findings. MRI should be considered if osteonecrosis of either the tibial plafond or
talus is suggested by the radiographs; this may dictate how much bone resection is required at the arthrodesis site to access vascular surfaces for fusion.
talus is suggested by the radiographs; this may dictate how much bone resection is required at the arthrodesis site to access vascular surfaces for fusion.
Simply placing a tibiotalar arthrodesis in neutral plantarflexion/dorsiflexion (0°), subtle hindfoot valgus (0° to 5°), and avoidance of internal rotation will generally result in a functional, plantigrade foot. However, disregard for whole limb and foot alignment may lead to a poor functional outcome, despite successful ankle fusion. Limb malalignment may need to be addressed before or simultaneous with ankle arthrodesis. A powerful advantage of arthrodesis with ring external fixation in the setting of proximal or distal malalignment or limb length discrepancy is that simultaneous combined procedures can be performed, such as proximal tibial corticotomy with lengthening/realignment and ankle arthrodesis or concomitant ankle and foot procedures.
When arthrodesis is planned in the face of infection, preoperative evaluation includes complete blood cell count with differential and blood cultures. Consideration may be given to an MRI or a combination technetium bone scan/indium-labeled white blood cells scan to confirm or evaluate the extent of infection, keeping in mind that peripheral vascular disease and antibiotics will interfere with the effectiveness of these studies. To obtain useful intraoperative cultures, antibiotics should be stopped at least 72 hours prior to surgery. Planning should include the potential for a staged procedure. Irrigation and debridement, hardware removal, and possible antibiotic bead placement should be planned as the first stage. If the ankle is determined to be unstable at that time, the external fixator frame may be placed for support. In a second stage, the antibiotic beads can be removed, the ankle again débrided, and compression may be applied through the ankle if there is no evidence of persistent infection. Alternatively, the plan can be for a single-stage procedure if the surgeon is satisfied that all of the infected tissue has been removed.
Preoperative expectations are critical to a successful result, and certain realities should be addressed in preoperative counseling, to include the risks of wound healing complications, pin tract infections, failure of fusion and requirement for additional procedures, neurovascular risks, and infection. Regarding pin tract infection, it is critical that the patient understands that pin tract infections are an inherent risk during ring external fixation and do not represent an unexpected complication nor necessitate automatic hardware removal; however, use of one or more cycles of oral antibiotics during the period of external fixator frame wear is often typical.
Daily living with an applied ring external fixator frame can be an intimidating and frustrating experience for some patients. Therefore, it is paramount that every potential patient understands thoroughly what the external fixator frame will look like and has a full appreciation for and understanding of the potential burdens and benefits of the external fixator frame prior to application. The authors find it helpful to maintain one or two previously removed, sanitized frames in the office or clinic to provide as exhibits for the patient who is considering ankle or TTC arthrodesis with ring external fixation. As well, it is often helpful to provide direct lines of communication with other consenting patients who also have an attached external fixator or previously did.
SURGICAL TECHNIQUES
Technique 1: Ankle Arthrodesis Using Ring External Fixation
A proximal regional anesthetic typically suffices for both ankle and TTC arthrodeses using external fixation. Tourniquet (thigh) use is generally limited to the approaches for joint preparation. External fixation alone cannot produce fusion; proper joint preparation is essential. Therefore, if there is any concern for the perfusion of any of the joint surfaces, then the tourniquet must be released before wound closure to confirm bleeding at the arthrodesis site. Tourniquet use is not required during application of the external fixator.
Positioning
The patient is positioned supine, often with a support under the hip of the operative leg. The goal is to orient the lower leg perpendicular to the operating table and floor to facilitate proper placement of the external fixator. A sterile proximal calf support (bump) (Fig. 39.1) should be created to suspend the lower leg during external fixator placement. The lower leg is prepared and draped in usual sterile fashion, and the leg is exsanguinated using a tension bandage unless persistent infection is suspected.
Surgical Approach and Joint Preparation
The ankle joint is approached using the individual surgeon’s preferred exposure, taking into account prior incisions and the status of the existing soft tissue envelope. We prefer to perform ankle arthrodesis through a direct anterior approach when possible, using the interval between the tibialis anterior (TA) and extensor hallucis longus (EHL) tendons, with preservation of the medial and lateral malleoli. We prefer to preserve the malleoli in most cases, as there is potentially more
surface area available for fusion and less bone loss. In selected cases, resection of one or both malleoli can improve bone contact and/or alignment.
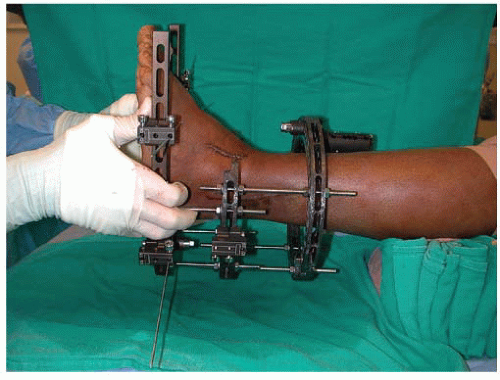
FIGURE 39.1 A support under the calf facilitates positioning of the external fixator. The surgeon must ensure that when the support is removed, the proximal ring does not impinge on the calf.
A longitudinal midline incision is made over the anterior ankle, starting approximately 10 cm proximal to the ankle joint and 1 cm lateral to the tibial crest, just along the lateral border of the palpable TA tendon (Fig. 39.2). The incision is extended distally to the talonavicular joint.
Deep, full-thickness retraction is used as soon as possible to limit the risk of skin compromise. We prefer early use of self-retaining retractors (i.e., Gelpi retractors), and at no point, should direct tension be placed on the skin margins. Protect the traversing branch of the superficial peroneal nerve, which is often identifiable as it crosses directly over or immediately proximal to the ankle joint.
The extensor retinaculum is identified and divided directly over the EHL tendon. In our experience, it is imperative to attempt to maintain the integrity of the TA tendon sheath during the approach, in order to minimize risk of anterior wound complications associated with tendon “bowstringing.” The EHL and TA tendons are retracted laterally and medially, respectively, with deep self-retaining retractors. The dissection is continued deep, and the deep anterior neurovascular bundle is identified and safely retracted laterally with the EHL tendon. Incise the anterior joint capsule and periosteum over the distal tibia and dorsal talar neck longitudinally, sharply dissect the
periosteum off the bone, and retract the capsule and periosteum medially and laterally, exposing the ankle joint fully (Fig. 39.3). Visually inspect the ankle joint, removing any loose bodies and anterior tibial or talar osteophytes as necessary.
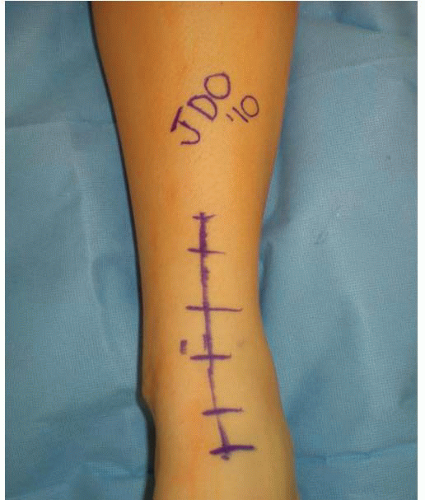
FIGURE 39.2 Incision for anterior approach to the ankle, utilizing the interval between the TA and EHL tendons.
Once the ankle joint is fully exposed, attention is now turned to meticulous joint preparation. Again, just as with ankle arthrodesis using internal fixation, external fixation does not obviate the need for thorough joint preparation. We routinely use joint distraction with either lamina spreaders or an invasive joint distractor placed over anterior smooth pins in the distal tibia and talar head-neck junction. (Remaining articular cartilage is removed with a sharp elevator, osteotome, or chisel.) We prefer to maintain the architecture of the subchondral bone of the tibial plafond and talar dome, which facilitates easy adjustment of coronal and sagittal plane alignment without compromising limb length or bony apposition. On the contrary, flat cuts sacrifice limb length and make alignment adjustments more challenging. In the setting of malalignment, some deformity correction may need to be made through the joint with limited sacrifice of the subchondral osseous anatomy. The subchondral bone is penetrated with a drill bit and/or narrow chisel (Fig. 39.4). This promotes fusion by increasing surface area, delivering autogenous bone graft to the arthrodesis site, and encouraging bridging trabeculae for fusion. The malleoli are preserved when possible, and the medial and lateral gutters are prepared as described above to further increase the arthrodesis surface area. Autogenous or allograft bone grafting is at the discretion of the individual surgeon, but excessive use of bone graft might prevent bony apposition and should be avoided when possible. In cases of prior infection, we selectively supplement limited bone graft with appropriate antibiotic powder.
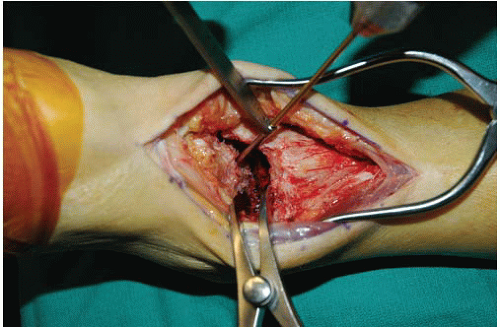
FIGURE 39.4 Lamina spreader placed laterally to facilitate subchondral bone drilling of medial talar dome.
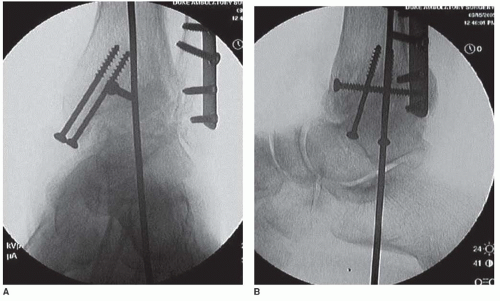
FIGURE 39.5 A: Intraoperative fluoroscopy, anterior posterior view, confirms proper alignment. In this case, provisional pin fixation was used. B: Lateral view.
Once the joint is prepared, attention is then turned to ankle joint reduction and provisional alignment prior to application of the external fixator. We find that provisional fixation with one or two smooth, large-diameter Steinmann pins is often necessary to maintain ideal position prior to application of the ring external fixator (Fig. 39.5). This pin is placed similar to the guide pin used for retrograde intramedullary TTC nail procedures. Provisional fixation should maintain adequate reduction of the prepared talus within the prepared ankle mortise. Optimal function and potential for fusion is established with maximum contact between the arthrodesis surfaces, avoiding anterior translation of the talus within the ankle mortise. Valgus is generally established in the hindfoot; varus malalignment at the ankle joint must be avoided. Furthermore, calcaneus or equinus positioning must be corrected to a neutral sagittal plane alignment. Finally, the second metatarsal should be in line with the tibial crest to ensure proper rotational positioning, avoiding internal rotation.
The wound is then gently irrigated and meticulously closed in a layered fashion, making sure to reapproximate the extensor retinaculum and subcutaneous skin. The skin is closed in a tensionfree manner, using nonbraided suture. We recommend closing the wound before applying the external fixator because access to the wound becomes challenging with the ring external fixator applied. If the individual surgeon chooses to close the wound after application of the ring external fixator, one or two anterior fixator struts or threaded rods can be retracted or removed to allow adequate access to the wound(s). A deep drain may be used to minimize the risk of hematoma and subsequent wound complications, but it must be positioned so as not to interfere with pin placement. Judicious use of incisional negative pressure wound dressings is at the discretion of the individual surgeon and may have a role in cases of prior infection or tenuous soft tissue envelope.
Safe Insertion of Transosseous Wires and Half Pins
With any use of external fixation, adherence to safe, proper transosseous wire and half pin placement is quintessential to avoid untoward injury to soft tissues and neurovascular structures at risk. For ankle and TTC arthrodesis, a thorough understanding of cross-sectional anatomy of distal lower extremity is paramount to safe use of transosseous fixation (11). In general, we recommend the use of 1.8-mm thin wires and 5- or 6-mm hydroxyapatite-coated half pins for ankle and TTC external fixator arthrodesis. Threaded half pins should be meticulously placed to ensure that threads
engage the tibia in a bicortical manner. Drilling and placement of half pins should always include use of blunt dissection to bone and use of tissue-protecting guides or sleeves placed against the bone. Saline solution should always be utilized during drilling to prevent thermal bone necrosis.
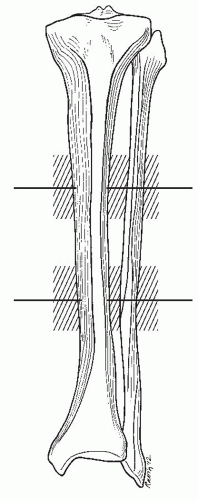
FIGURE 39.6 Shaded areas show safe zones, or preferred anatomic levels, for placement proximal-most and distal-most rings for proximal (tibial) ring block.
For the purposes of ankle and TTC arthrodesis, we generally recommend a two-ring proximal tibial block. The top, or proximal-most, ring in the tibial block is generally placed just distal to the midshaft of the tibia. The bottom, or distal-most, ring in the tibial block is generally placed in the distal third of the tibia, proximal to the metaphyseal flare (Fig. 39.6). The tensioned reference wire for the proximal-most ring is placed in a medial-oblique manner or directly perpendicular to the long axis of the tibia, and two half pins are placed directly perpendicular to the medial face of the tibia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









