Tibiofibular Syndesmosis Reduction and Fixation
Arup K. Bhadra
David A. Porter
INTRODUCTION
Syndesmosis injury or high ankle sprain has been identified by many physicians as the most difficult injury to treat in the athlete (1,2). It is well known as a greater source of impairment in high-level as well as recreational athletes than the more typical lateral (low) ankle sprain (3, 4, 5 and 6). It accounts for 1% to 18% of all ankle sprains (3,7,8). There is a wide spectrum of syndesmosis injuries ranging from a minor sprain of the anterior, inferior tibiofibular ligament (AITFL) to frank diastasis of the entire tibiofibular joint complex. Many cases of frank diastases occur with a fracture of the fibula (Maisonneuve or Weber C); however, a sprain of the syndesmosis without a fracture to the fibula with diastases is also possible (Grade II or III syndesmosis dislocation).
The syndesmosis is made up of three ligaments including the interosseous membrane. The ligaments include (a) the AITFL—the first and the most common (9) to fail with an external rotation force; (b) the posterior inferior tibiofibular ligament (PITFL) consisting of a superficial and deep portion, which is also known as the transverse tibiofibular ligament; and (c) the interosseous ligament (also known as the interosseous membrane). The interosseous ligament is the strongest portion of the syndesmosis and is the main ligamentous support between the tibia and fibula (10).
External rotation force is the most significant force in a syndesmosis injury (8,11,12). Patients/athletes present with severe ankle pain directly over the syndesmosis and commonly the medial ankle. The pain and swelling is severe both medially and laterally with complete disruption, but can be conspicuously absent in the stable “high ankle sprain.” When the mechanism of injury is suspected to occur with an abduction and external rotation force, a rupture of the deltoid ligament or a fracture of medial malleolus will produce tenderness over the medial ankle. Moreover, the fibula must be palpated from distal to proximal to rule out the possibility of a Maisonneuve fracture or proximal tibiofibular joint disruption.
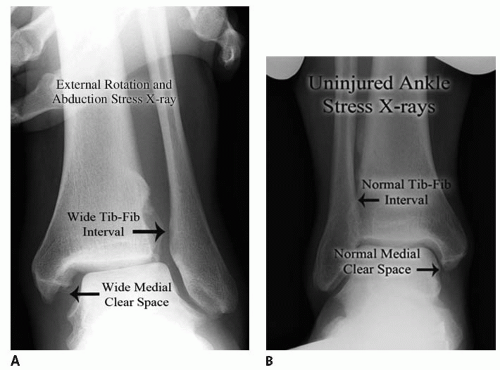
The “squeeze test” described by Hopkinson et al. (8) is a method of detecting “stable” syndesmosis injuries. We find the external rotation test to be more reliable for assessing syndesmosis injuries. The test is performed by stabilizing the leg with the knee flexed at 60° to 90° while hanging off the exam table and externally rotating the dorsiflexed foot. Pain is produced at the syndesmosis in the distal leg and ankle when it is injured. The next step in the evaluation of syndesmosis injury (13, 14 and 15) is to obtain routine radiographs. A careful evaluation of the distal tibiofibular relationship with regard to the medial clear space, the tibiofibular clear space, and the tibiofibular overlap is crucial (16, 17 and 18). A radiograph of the uninjured ankle can be utilized to help clarify the normal anatomic relationship of distal tibia and fibula (Fig. 31.1). We use weight-bearing radiographs as our initial evaluation to give physiologic stress to the ankle ligament. Occult diastasis can often be detected using this method, but on occasion, stress radiographs are needed to elicit this occult disruption.
Criteria for the Diagnosis of Diastases
Medial clear space widening (normal 2 to 3 mm) or greater than 1 to 2 mm than opposite uninjured side (Fig. 31.2)
Increased tibiofibular clear space (normal is less than 6 mm AP and mortise views)
Less tibiofibular overlap (normal is greater than or equal to 6 mm AP view)
As mentioned, stress radiographs with application of external rotation and abduction force can be required to expose an occult diastasis (see Fig. 31.1). Bone scan, CT, and MRI (Fig. 31.3) are other radiographic modalities used in the diagnosis of syndesmosis injury. MRI allows an accurate picture of ligamentous anatomy and the distal tibiofibular joint. Oae et al. (19) reported a sensitivity of 100%, a specificity of 93%, and an accuracy of 97% in diagnosing a syndesmosis injury with MRI.
Acute traumatic syndesmosis injury can be classified into three grades:
Grade I—stable sprain without diastasis—“high ankle sprain”
Grade II—latent diastasis or diastasis that is only apparent after stress radiographs
Grade III—frank diastasis (seen on routine, nonstress radiographs)
The initial treatment of acute syndesmosis injuries should begin with rest, ice, compression, and elevation (RICE). The affected leg should be immobilized and the patient should remain non-weight bearing while the appropriate diagnostic tests are ordered (16,20,21). Sprains without diastases can be treated nonsurgically. Patients may bear weight as tolerated in a walking boot or brace. Crutches are used if weight bearing is painful. Physical therapy can start once pain subsides and weight bearing becomes easier. Patients with latent diastases do not require surgery if anatomical reduction of distal tibiofibular joint is confirmed by CT or MRI. The patient is immobilized in a non-weightbearing cast or walking boot. A repeat weight-bearing radiograph at 2 to 3 weeks postinjury should be obtained to confirm continued anatomical reduction. Gradual weight bearing can be allowed at 4 weeks, with full weight bearing by 8 weeks postinjury.
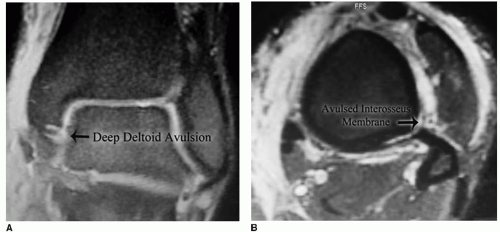 FIGURE 31.3 Same football player as in Figure 31.1. A: Coronal STIR image shows syndesmosis disruption and subtle evidence of avulsed deep deltoid but no evidence of bone bruising in the ankle. B: Axial STIR image shows possible partial avulsion of interosseous membrane off the posterolateral tibia with thickened membrane and periosteal edema. |
INDICATIONS AND CONTRAINDICATIONS
In most situations, such as elite, competitive, or even recreational athletes, those with latent diastases may do better with surgical treatment. In fact, this author prefers a more aggressive surgical approach for this latent instability (21). On the other hand, frank diastases always require surgical stabilization as soon as the soft tissue envelope is healthy, unless there are overriding medical contraindications (16). Any lateral displacement of the talus or fibula requires internal fixation.
PREOPERATIVE PLANNING
Careful and thorough assessment of the patient including mechanism of injury, level of activities of the athlete, and review of high-quality radiographic investigations are important to make correct diagnosis as well as predict outcome. A preoperative plan or surgical tactic may provide mental preparation and avoid unnecessary mistakes. Patients should be appropriately counseled about the risks and benefits and also be warned about ankle stiffness and persistent activity-related pain despite good ankle function (5).
SURGICAL TECHNIQUE
Patient Positioning and Preparation
Patients are generally positioned supine, and a general and/or ankle block anesthetic is administered. A towel roll is placed under the ipsilateral buttock to keep the lower leg in a position of neutral rotation.
Prophylactic intravenous antibiotics are administered prior to skin incision. A first-generation cephalosporin is used unless there is allergic contraindication, in which case an alternative antibiotic is chosen.
Stability of the syndesmosis is tested with external rotation and abduction stress under fluoroscopy and the image is saved on the C-arm screen for comparative guidance later on.
A general anesthetic is typically required for this procedure because of the proximal extent of the interosseous injury. A field block to the distal lateral leg and medial ankle can be undertaken to decrease the discomfort from the tourniquet. This surgeon places an ankle block at the beginning of the procedure to decrease intraoperative and postoperative pain.
A sterile tourniquet is placed on the calf after padding with sterile Webril to decrease any risk of an upper leg deep venous thrombosis.
The foot and ankle are prepped in routine sterile fashion with Betadine scrub, paint, and alcohol up to the knee, or more recently ChloraPrep. The toes are excluded from the operative field with the use of an Ioban.
At the appropriate time, the foot, ankle, and leg are exsanguinated and the tourniquet is inflated. We use 275 mm Hg for our tourniquet pressure and have found this to be more than adequate for the calf tourniquet.
Medial Exposure
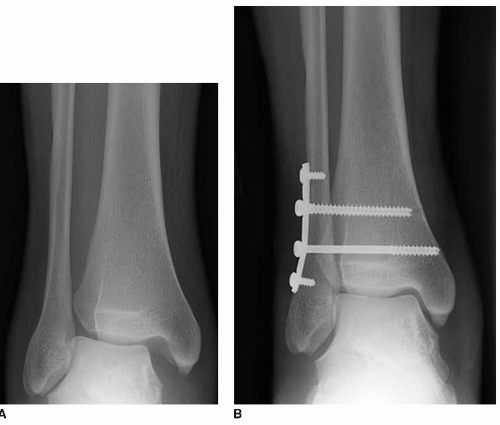
When the preoperative radiograph suggests medial clear space widening (see Fig. 31.2A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree