Chapter 81 Tibial Plateau Fractures
Fractures of the tibial plateau represent only 1% to 2% of all fractures but account for approximately 8% of fractures occurring in older adults.18 As our understanding of the importance of soft tissue injury has evolved concurrently with the evolution of internal fixation devices and techniques, management of these difficult injuries has slowly shifted from primarily a nonoperative course to one of restoration of the articular surface with internal or external fixation and early motion, when possible. Additionally, classification systems and clinical outcome data have dramatically improved our ability to understand and manage these fractures.
Relevant Anatomy
The medial and lateral menisci are both semilunar, triangular-shaped fibrocartilage that rest between the femoral condyles and tibial plateaus. They serve an important function in load sharing by protecting the articular cartilage from up to 60% of the load encountered by the knee.20 The lateral meniscus is larger than the medial meniscus and covers a larger percentage of the lateral plateau. The intermeniscal ligament anteriorly connects the anterior horns of the two menisci, and the menisci are attached peripherally by the coronary ligaments to the peripheral rim of their respective tibial plateaus. The anterior attachment of the lateral meniscus is slightly posterior to that of the medial meniscus. It is important to recognize the normal anatomy of these structures because they are often damaged and require repair in the management of tibial plateau fractures.
Mechanism of Injury
The predominant pattern producing tibial plateau fractures is a varus or valgus stress, with concomitant axial loading. This combination may be seen with low-energy injuries, such as falls from a standing height, or with high-energy injuries, such as motor vehicle accidents. Isolated valgus or varus loading tends to cause an isolated lateral or medial injury, respectively. The more an axial load predominates, the more likely a patient is to sustain a bicondylar injury. The lateral plateau is involved in 55% to 70% of cases, with medial plateau or bicondylar involvement occurring in 10% to 30% of cases.18 Simple central depression–type injuries are often the result of low-energy injuries in older patients with osteoporotic bone and, conversely, bicondylar fractures with axial loading and shearing injuries tend to be seen in high-energy injuries in younger patients.
Classification
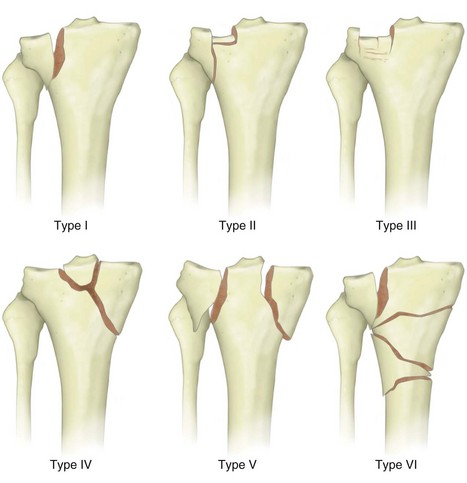
Comprehensive anatomic classifications such as the AO (Arbeitsgemeinschaft fur Osteosynthesefragen) classification or the Orthopaedic Trauma Association classification may be useful for research purposes (Fig. 81-1). However, they are somewhat cumbersome and may be difficult for surgeons to use for clinical communication. The most commonly used classification system in clinical practice is the Schatzker classification system (Fig. 81-2).19
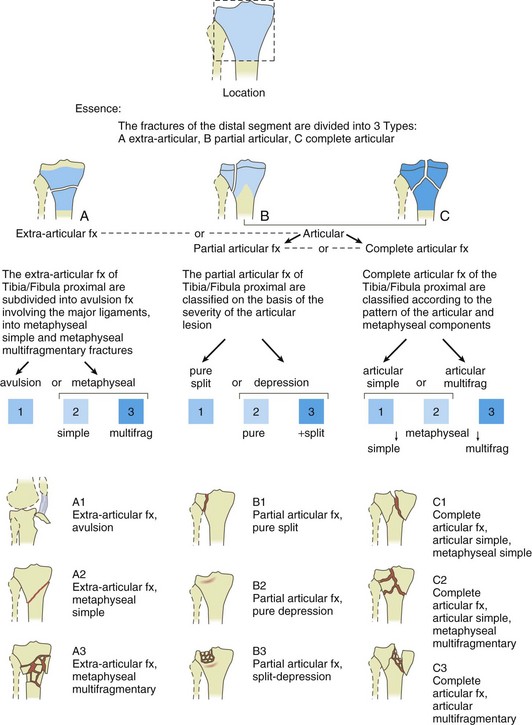
Figure 81-1 AO-ASIF classification of tibial plateau fractures.
(From Müller ME, Nazarian S, Koch P, Schatzker J: The comprehensive classification of fractures of long bones, Bern, Switzerland, 1995, ME Müller Foundation.)
Experienced surgeons know that it is the status of the soft tissues and classification of the soft tissue envelope injury that are as important, if not more important, than the underlying osseous injury. The Tscherne classification of soft tissue damage in closed fractures is an excellent means whereby surgeons can evaluate associated soft tissue injuries.16 A grade 0 injury results from indirect trauma and is associated with negligible soft tissue damage. A grade I injury typically results from low or moderate energy and is identified by superficial abrasions or overlying contusions. In grade II injuries, significant muscle contusion and possible deep contaminated abrasions may be seen. Grade II injuries may be the result of a bumper strike and are often associated with marked fracture comminution. The highest grade in the classification system is grade III soft tissue injury, which is frequently associated with extensive crushing of soft tissues and subcutaneous degloving. There may be concomitant arterial injury. Patients with compartment syndrome automatically fall into the grade III category.
Clinical Evaluation
Physical Examination
One cannot overemphasize the importance of a complete neurologic and vascular examination. Knee dislocations leading to vascular or neurologic injury in association with tibial plateau fractures have been reported to reduce spontaneously and may be missed without careful examination. If pulses are not equal on palpation, arteriography may be performed.15 Use of the ankle-brachial index (ABI) to compare blood pressure in the arm and ankle can help evaluate the vascular status of the limb further. Neurologic injury, most commonly in the form of peroneal nerve palsy, is not uncommon.19 Careful motor and sensory evaluation of the lower part of the leg must be undertaken arduously.
Imaging Studies
The use of MRI for the evaluation of acute knee injuries continues to improve and evolve. The sensitivity and specificity of MRI for meniscal and cruciate ligament injury are greater than 90% when correlated with arthroscopic or intraoperative findings.5 MRI should not be used indiscriminately in place of a careful clinical evaluation, routine plain films, and CT scanning. Its benefit in tibial plateau fractures lies largely in the exclusion of significant meniscal tears or ligamentous injuries in patients who would otherwise be treated nonoperatively or in a percutaneous fashion such that these injuries would then perhaps be missed. Studies in which MRI was performed on tibial plateau fractures have shown associated soft tissue injuries in greater than 45% of patients.11 The role of MRI in the preoperative evaluation of these injuries remains undefined.
Angiography
Angiography is indicated when the vascularity of the lower part of the leg is in question. Asymmetrical distal pulses or an ABI below 0.9 should prompt angiographic examination.15 It is important to recognize that if a leg is obviously ischemic, angiography may be helpful in localizing the injured area but it must not delay vascular exploration and subsequent revascularization to the point that viability of the limb will potentially be compromised. “On the table” angiography by the vascular team in the operating room while spanning external fixation is being performed may help expedite the overall care of the patient in such circumstances. Prolonged ischemia may cause a reperfusion compartment syndrome after perfusion is restored. Therefore, prophylactic fasciotomies may be indicated.
Treatment
Initial Management
In all tibial plateau fractures, the status of the soft tissues is of paramount importance in determining the timing of internal fixation. Patients with higher energy injuries and significant soft tissue damage should typically undergo temporizing knee-spanning external fixation until the soft tissues have recovered to a state in which a surgical incision can safely be made. Surgical incisions made through acutely traumatized tissue portend a high rate of wound dehiscence, wound infection, and subsequent soft tissue complications. It is not uncommon in higher energy injuries for it to take several weeks for the soft tissue envelope to become amenable to surgical intervention. At times, it may be estimated by an experienced physician that the soft tissue envelope will not become amenable to surgical incision for more than 3 to 4 weeks. In such situations, methods other than formal internal fixation will probably need to be used. Delayed definitive internal fixation with the use of temporizing spanning external fixation (Fig. 81-3) has markedly decreased the rate of complications in this difficult patient population. Lower energy injuries, such as those seen after a simple fall that results in a depression fracture in an osteoporotic patient, may often be fixed relatively acutely because the associated soft tissue injury is minor. Obviously, the surgeon’s judgment is paramount when evaluating the character of the osseous and soft tissue injuries.
Nonoperative Management
Although no clear-cut guidelines have been established across all patient ages and activity levels regarding what is acceptable to treat nonoperatively, some general rules can be applied. An articular step-off of less than 3 mm or condylar widening of less than 5 mm tends to have an acceptably low rate of adverse long-term effects if treated nonoperatively. Function deteriorates, however, with varus tilt, whereas mild valgus tilt up to 5 degrees is generally well tolerated.8 Nonoperative management would be poorly advised if a tibial plateau fracture were associated with varus or valgus instability in a fully extended knee joint. Age alone is not an absolute contraindication to surgical management because older patients do well functionally with proper treatment.10 However, surgeons must clearly use their judgment about the expectations, functional demands, medical comorbid conditions, and surgical risks of the specific patient being treated when making a decision regarding the most appropriate intervention. The goal of nonoperative treatment is still to allow early range of motion to include full extension and 120 degrees of flexion. It is known that permanent knee stiffness will probably develop if fractures treated nonoperatively are immobilized for longer than 6 weeks.6
Nonoperative management can include a period of traction and/or casting, followed by early range of motion in a cast brace or functional brace. Cast brace treatment of minimally displaced unicondylar fractures tends to yield good results, but outcomes are far less predictable with bicondylar fractures.2 In general, nonoperative treatment is typically reserved for stable, well-aligned, minimally displaced fractures or fractures in patients with prohibitive medical comorbidity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree