Tibial Periarticular Fracture Reduction and Fixation
John P. Ketz
Roy W. Sanders
INTRODUCTION
Fractures of the weight-bearing articular surface of the tibia are complex injuries that present challenges to the treating surgeon (1). Tibial “pilon” or “plafond” fractures encompass a wide spectrum of injuries. Each is unique but can be separated into low-energy and high-energy injury patterns. These injuries require distinct treatment protocols. High-energy injuries include complex patterns that are associated with significant articular cartilage and soft tissue damage. Initially, immediate open reduction and internal fixation (ORIF) of these injuries were performed, but this was associated with a high rate of wound complications and poor results due to soft tissue compromise (2). External fixation was then used with and without limited ORIF as definitive fixation (3, 4, 5 and 6). This method did not allow for anatomic restoration of the articular surface and only introduced other complications, which led to the concept of a staged treatment protocol. This has been the mainstay of treatment, because it uses external fixation in a temporary manner to allow soft tissues improvement and surgical planning (7, 8, 9 and 10). Then, formal open reduction can be performed to anatomically reduce the articular surface. This technique has improved results and decreased complications. Newer techniques still employ the staged method of treatment but have added fragment-specific fixation with multiple soft tissue-friendly approaches (11).
INDICATIONS AND CONTRAINDICATIONS
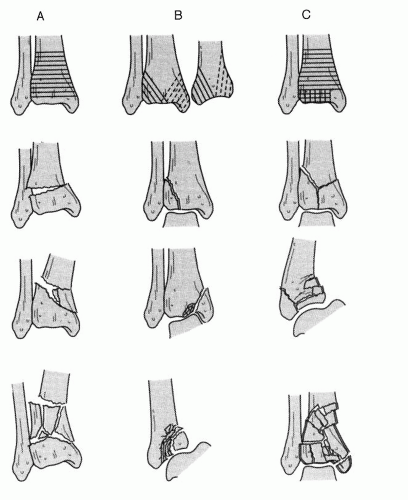
The treatment for tibial pilon fractures is almost exclusively operative. Nonoperative treatment is typically reserved for only truly nondisplaced fractures or for those patients that are poor surgical candidates with significant contraindications to intervention. Consideration may be given to operative treatment for these nondisplaced fractures in the poly-trauma setting as it will minimize the risk of displacement and allow for early range of motion (ROM). Operative indications include articular displacement, unacceptable axial alignment, and open fractures. The goal of the surgery is to restore the mechanical alignment to the distal tibia as well as anatomical reduction to the joint surface. Poor articular reductions and residual tibiotalar incongruity produce poor clinical results secondary to posttraumatic arthrosis and pain. There are a number of different techniques available for treatment of these injuries ranging from external fixation to open fixation, or a combination of both. The surgical management of pilon fractures depends on fracture pattern, soft tissue quality, and surgeon preference. The Orthopaedic Trauma Association (OTA) classification system for pilon fractures is depicted in Figure 40.1.
PREOPERATIVE PLANNING
Patients should be initially stabilized with splinting techniques and appropriate wound care for open injuries. Formal radiographs should be obtained of the ankle as well as the tibia and fibula. If there is suspicion for an intraarticular fracture without significant displacement on the plain radiographs,
a computed tomography (CT) can be used initially. The importance of CT scans is paramount as it provides a three-dimensional depiction of the injury. If the fracture is a low-energy pattern and the surrounding soft tissues appear adequate, consideration may be given to immediate ORIF or stabilization using percutaneous techniques.
a computed tomography (CT) can be used initially. The importance of CT scans is paramount as it provides a three-dimensional depiction of the injury. If the fracture is a low-energy pattern and the surrounding soft tissues appear adequate, consideration may be given to immediate ORIF or stabilization using percutaneous techniques.
Most pilon fractures, however, have a high-energy pattern and significant soft tissue compromise. Open injuries should be treated urgently with adequate debridement and temporary closure, if possible. In this scenario, external fixation should be used initially, with fixation of the fibula, if indicated. We strongly recommend that only the surgeon, who will definitively perform fixation, be the one who stabilizes the fibula. This will ensure that any further planned incisions will not be compromised by a previous fibular incision. In fractures with a displaced posterior malleolar fragment, consideration should be given to initial stabilization of this fragment through a posterolateral incision, in combination with external fixation. Fibular fixation may be performed through this incision at the same time.
SURGICAL TECHNIQUES
Technique 1: Stage 1 Temporary Fixation
Fibula Fracture Stabilization
The patient is initially stabilized in the emergency room and brought to the operating room for temporary fixation. If the surgeon will be the one performing definitive fixation, the fibula, if fractured, should be addressed at this time.
If the tibial fracture does not have a posterior malleolar component, or the fracture is not displaced, the patient is placed into the supine position on the operating room table. A tourniquet is applied to the thigh, an Esmarch bandage is used to exsanguinate the leg, and the tourniquet is inflated to 325 mm Hg.
A posterolateral, or a lateral incision, is used to reduce the fibula. Dissection is carried down sharply to expose the peroneal fascia. By staying posterior on the fibula, minimal dissection is performed anteriorly, and the risk of superficial peroneal nerve injury is minimized.
A small cuff of the peroneal fascia is left on the posterior aspect of the fibula to expose the fracture.
Special attention must be paid to restoring the length and rotation of the fibula during fixation as this can impede an anatomical reduction of the tibia.
Plates are typically used for fibular fixation with 1/3 tubular plates for distal fractures and 3.5-mm reconstruction plates or small fragment plates for more proximal fractures. Alternatively, intramedullary pins or screws may be used for distal, noncomminuted fractures that have a more transverse pattern.
The screws can be placed through limited or percutaneous incisions using fluoroscopy. If using the latter technique, the surgeon must guarantee that the distal fibula is not rotated or angulated.
Pearl: Often the fibula fracture is highly comminuted and restoring length and rotation can be challenging. In this scenario, it may be beneficial to apply a medial-based external fixator and gain temporary reduction of the tibia. This technique can restore axial alignment and provide support to the fracture to allow for “fine tuning” of the fibula.
External Fixation
External fixation can be performed through small incisions and allow for temporary stabilization and soft tissue care until formal fixation can occur.
A variety of options for pin placement can be performed. Typically, two (2) 5.0-mm half pins are placed in the tibia through anterior incisions. This should be performed with fluoroscopy to place the pins proximal to the site of any future implants that may be used.
A calcaneal half pin is then placed in a medial to lateral fashion. A transcalcaneal pin should only be used if fibular fixation is not performed to stabilize the lateral column.
Talar pins also have a role for unstable injuries that cannot be held reduced with tibial and calcaneal pins. These pins add an additional fixation point to prevent tibiotalar translation in the sagittal (AP) plane. Talar pins are not routinely used as they are very close to, or in direct contact with, the fracture and may limit future incisions.
Additional forefoot (first metatarsal, cuboid) pins should be considered to prevent the development of an equinus contracture if the soft tissues do not allow for definitive fixation for an extended period of time.
Posterior Malleolar Fracture Stabilization and Application of Frame
If there is a displaced posterior malleolar fragment, it is beneficial to reduce and stabilize this fragment at the time of external fixation and stabilization of the fibula fracture, if present (Fig. 40.2).
In this situation, the patient is placed prone on the operating room table and a tourniquet is applied to the thigh (Fig. 40.3A). The leg is then elevated and exsanguinated.
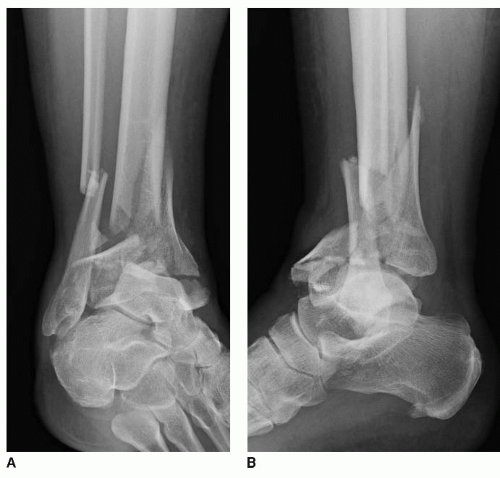
FIGURE 40.2 Radiographs of a 38-year-old female with a high-energy pilon fracture (OTA 43C3) with a large displaced posterior malleolar fragment. A: AP view. B: Lateral view.
A posterolateral incision is placed between the posteromedial aspect of the fibula and the posterolateral aspect of the Achilles tendon (Fig. 40.3B). The incision should be marked on fluoroscopy and is dictated by the proximal extent of the spike of the posterior malleolar fragment.
Dissection is carried down laterally to the peroneal fascia and care should be taken to protect the sural neurovascular structures. The fascia is incised longitudinally. The peroneal tendons are retracted medially to expose the fracture.
The posterior aspect of the fibula is exposed and can then be directly reduced with fracture clamps and plated (Fig. 40.4).
Pearl: For comminuted fractures where restoring length is an issue, a transcalcaneal pin can be placed and used for traction purposes. Also, a reduction clamp can be placed on the distal fragment and pulled inferiorly once the length and rotation are correct, at which point the distal fibular fragment can be K-wired with two 2.0-mm smooth pins into the lateral aspect of the talus.
Dissection is then carried out medially through the incision and the interval between the flexor hallucis longus (FHL) and peroneal tendons is developed (Fig. 40.5A).
The peroneals are retracted laterally and the FHL is retraced medially with the Achilles tendon. The posterior aspect of the tibia is then well visualized. Minimal soft tissue stripping should be performed as excessive dissection in this area can destabilize the syndesmosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree