Thumb Opponensplasty
Ashraf M. Youssef
Colleen Davis
Kevin J. Malone
“A great asset to man is the opposable thumb. The hand (is) so useful to all and the livelihood of the manual worker owes much of its efficiency to this pincer action of the thumb.”
—Sterling Bunnell, 1938
INTRODUCTION
Thumb opposition is a complex multiplanar movement performed by median nerve innervated muscles. It is often confused with thumb apposition, which is simply placing the thumb in contact with the fingers. True opposition, however, involves placing the thumb forward to the fingers out of the plane of the palm and with the pulp of the thumb facing the pulp of the fingers (Fig. 20-1). This is achieved by a combination of three distinct movements of the thumb ray: metacarpal palmar abduction, metacarpal pronation, and metacarpophalangeal (MCP) joint flexion. This movement is coordinated through contraction of the abductor pollicis brevis (APB), flexor pollicis brevis (FPB), and opponens pollicis (OP) with APB being the most important of the three.
Thumb opponensplasty involves restoration of thumb opposition via transfer of a functional, expendable, extrinsic, or intrinsic muscle-tendon unit to the thumb ray to compensate for the functional loss of the thenar muscles.
ANATOMY
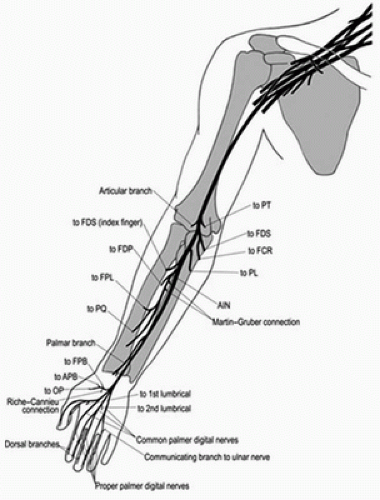
A thorough understanding of median nerve anatomy is necessary to properly diagnose and treat median nerve palsies (Fig. 20-2). Below is the classically described innervation pattern of the median nerve; however, significant overlap with the ulnar nerve does exist, particularly with the musculature of the hand. Multiple anatomic studies describe pure median, pure ulnar, and dual median/ulnar innervations of each of the thenar muscles. This is supported by the fact that FPB remains functional in 73% of complete median and 58% of complete ulnar nerve injuries.
The median nerve is composed of fibers from the medial and lateral cords of the brachial plexus.
The median nerve enters the forearm through the two heads of pronator teres and travels to the wrist between flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP).
The anterior interosseous nerve (AIN) branches from the median nerve at the level of pronator teres and innervates flexor pollicis longus (FPL), FDP to the index and long fingers, and pronator quadratus (PQ).
Proximal to the AIN branch, the median nerve innervates pronator teres, flexor carpi radialis, palmaris longus, and FDS.
Distal to the AIN branch, the median nerve passes through the carpal tunnel and innervates APB, OP, and FPB via the recurrent motor branch. Additionally, the first and second lumbricals are also innervated by the median nerve.
It is essential that one be familiar with variations in the origin and course of the recurrent motor branch of the median nerve to avoid iatrogenic injury during procedures around the wrist. Common variations with their approximate incidences include the following:
Greater than 50%—originates distal to the carpal tunnel or within the carpal tunnel exiting distally beneath the transverse carpal ligament (TCL)
25%—pierces through the TCL
10%—exits the carpal tunnel ulnarly distal to the TCL and then travels radially to the thenar compartment volar to the TCL
Another variation that one must be familiar with is a potential communicating motor branch between the median and ulnar nerves.
Martin-Gruber anastomosis: approximately 10% to 44% of individuals. Motor fibers from proximal median nerve or AIN travel to ulnar nerve in the forearm.
Riche-Cannieu anastomosis: present in approximately 77% of individuals. Motor fibers from the deep motor branch of ulnar nerve in the hand travel to the median nerve.
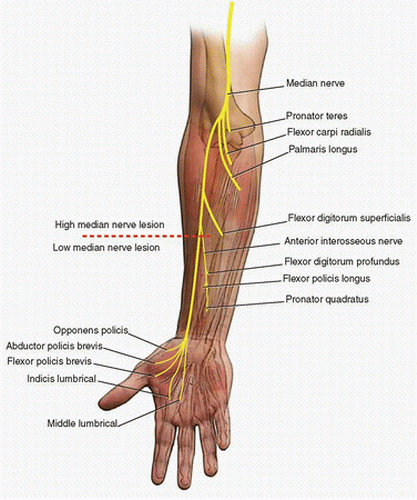
Low median nerve palsy is defined as a lesion of the median nerve proper distal to AIN branch. Conversely, high median nerve palsy involves a lesion of the median nerve proximal to the
branching of the AIN therefore manifesting with loss of both median nerve and AIN innervated muscle function (Fig. 20-3).
branching of the AIN therefore manifesting with loss of both median nerve and AIN innervated muscle function (Fig. 20-3).
Low median nerve palsy leads to loss of thumb opposition. Paralysis of the first and second lumbricals is also present but usually clinically insignificant if the ulnar nerve is intact as their function can be compensated by the ulnar nerve innervated interossei muscles.
High median nerve palsies includes the above deficits in addition to loss of some or all of the following:
Forearm pronation—as PQ is innervated by the AIN.
Thumb and index finger flexion—as FDP to the index finger and FPL are innervated by the AIN.
Long-finger flexion—loss of long-finger flexion is more variable than is loss of index finger flexion as FDP to the long finger often has dual innervation from the AIN and ulnar nerve. It may receive sole innervation from the ulnar nerve in up to 50% of individuals.
INDICATIONS
Opponensplasty is indicated for loss of thumb opposition in the setting of a stable and supple thumb ray. Although exceedingly rare today due to vaccination, polio has historically been the most common indication for thumb opponensplasty. Common indications today include loss of thumb opposition due to:
Chronic median nerve entrapment neuropathies resulting in thenar atrophy
Median nerve injury
Muscular dystrophies
Loss of the thenar musculature due to infection or trauma
CONTRAINDICATIONS
Opponensplasty will be unsuccessful if performed in the setting of a first web space contracture. The contracture must first be addressed with therapy, splinting, and/or surgery.
Noncorrectable instability or contracture in any joints of the thumb ray precludes opponensplasty.
While there are few absolute contraindications to opponensplasty, one must adhere to the general principles for tendon transfers.
Full passive range of motion must be present or established prior to transfer.
Tendon transfers should not be performed in the setting of an open wound.
The donor muscle must be of sufficient strength and its primary function expendable.
The donor tendon must be of sufficient length and travel in-line with the force vector of its new desired function after transfer.
Choosing a donor muscle with synergistic function to the one(s) being replaced will facilitate postoperative rehabilitation.
PREOPERATIVE PREPARATION
The hand and fingers must be assessed for adequate range of motion. Contractures and joint stiffness are common in long-standing median nerve palsies. These can be prevented preoperatively with appropriate splinting and therapy. Once contractures have developed, they must be corrected prior to opponensplasty with aggressive therapy, splinting, and/or surgical release.
Dorsal skin contractures of the first web space that fail to respond to splinting can be addressed with Z-plasty or a dorsal rotational flap with skin grafting.
All soft-tissue wounds should be stable. Ideally, the tendon transfer should pass through uninjured supple tissues to minimize potential of tendon adhesions.
Contracture of the carpometacarpal (CMC) joint capsule can lead to isolated loss of thumb pronation. This can often be treated with thumb CMC capsulotomy.
Severe contractures and those that fail to respond to the above treatments may be treated with metacarpal osteotomy and/or trapeziectomy.
The interphalangeal (IP) joint of the thumb must be stable and capable of extension to neutral to provide a stable post for pinch grip. Repair or tenodesis of the EPL tendon or fusion of the IP joint should be performed if necessary.
Strength and functional excursion of the flexors and extensors of the wrist and fingers must be examined in order to determine the musculotendinous units available for transfer.
The function of the donor motor unit must be expendable.
The donor motor unit must be of sufficient strength preoperatively. The transferred unit will lose one grade of strength on the Oxford scale after transfer (Table 20-1).
The length of the donor motor unit is also of key importance. An ideal donor tendon should comfortably reach the thumb MCP joint without lengthening, grafting, or overtensioning. It is challenging to set appropriate tension through a lengthened system or graft, and overtensioning may adversely affect the power by altering the length-tension relationship of the muscle.
Finally, proper patient selection and education are paramount to success. A technically well-performed transfer will lead to poor outcomes in a patient who is noncompliant with the postoperative therapy. Furthermore, excellent objective outcomes do not preclude poor subjective outcomes in a patient with unrealistic expectations.
TABLE 20-1 Oxford Scale for Grading Muscle Strength | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The surgeon must have a detailed discussion with the patient on what is reasonable to expect in terms of potential functional recovery.
The discussion must stress the need for participation in a lengthy, structured postoperative rehabilitation plan such as the one outlined in the therapy section of this chapter. A patient who is unable or unwilling to actively participate in pre- and postoperative therapy should be discouraged from undergoing opponensplasty.
TECHNIQUE
There is no agreed-upon “best” technique for opponensplasty for low median nerve palsy. Four common techniques are listed in Table 20-2 and described below. The FDS to the ring finger appears to be the most commonly used technique; however, transfer of the extensor indicis proprius (EIP) tendon is becoming more popular because it does not weaken the patients grip and leaves little to no functional deficit. One study by Anderson suggests that FDS is better suited for stiffer hands while EIP performed better in more supple hands. The Huber technique has the unique benefit of cosmesis as the bulk of the transferred unit somewhat restores the appearance of a thenar compartment. For this reason, it is often used in pediatric cases. The Camitz technique restores the least amount of function but is a relatively simple procedure that can be performed in severe cases of carpal tunnel syndrome at the time of carpal tunnel release through an extended incision.
Opponensplasty for high median nerve palsy is treated in the same manner as a low palsy; however, the additional deficits must also be addressed, specifically loss of thumb IP, index, and long finger flexion as well as forearm pronation. The FDS transfer is not available as a donor motor unit in high median nerve palsy.
Thumb IP flexion can be restored via transfer of the brachioradialis tendon to the FPL tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree