Surgical Repair: Reconstruction of Acute and Chronic Thumb Metacarpophalangeal Ulnar Collateral Ligament Deficiency
Thao P. Nguyen
Ngozi Mogekwu Akabudike
INTRODUCTION
The ulnar collateral ligament (UCL) is the primary stabilizer of the thumb metacarpophalangeal (MP) joint under radial or valgus stress. Injuries to the UCL are common after falls, sporting injuries, or motor vehicle accidents causing forced abduction or rotation and hyperextension at the thumb MP joint. Campbell, in 1955, coined the term “gamekeeper’s thumb” to describe chronic attritional injury to the UCL seen in Scottish gamekeepers who killed their game by grasping the head of the animals, often rabbits, between their thumb and index finger to break the animals’ necks (1). Acute injury to the UCL is termed “skier’s thumb” because of the high incidence seen after skiing accidents (2). This occurs when the pole maintains the thumb in an abducted position causing radial deviation. Incompetence of the thumb UCL frequently leads to painful, chronic instability and poor function.
ANATOMY
The thumb MP joint is a diarthrodial joint capable of abduction, adduction, flexion, and extension. Unlike the other fingers in the hand, the thumb MP joint must remain stable in both flexion and extension to resist the radial and ulnar stresses incurred during pinch and grasp. The thumb MP joint has considerable variation in the flexion-extension arc and degree of valgus laxity (3,4). Stability of the thumb is critical for overall hand function and is often achieved at the expense of
motion. Thumb MP joint stability is provided by the bony anatomy as well as dynamic and static restraints. Compared with the finger metacarpals, the thumb metacarpal head is less spherical and its cartilage is more limited on the dorsal aspect leading to further stability (5). The static restraints are the proper and accessory collateral ligaments, the palmar plate, and the dorsal capsule. The proper collateral ligament extends from the midaxis of the metacarpal head to the palmar aspect of the proximal phalanx (Fig. 8-1). Along with the dorsal capsule, this ligament is taut in flexion. The proper collateral ligament serves as the primary restraint to valgus stress with the MP joint flexed and prevents palmar subluxation of the proximal phalanx. The accessory collateral ligament is palmar to and contiguous with the proper collateral ligament at the metacarpal head and inserts onto the volar plate (Fig. 8-2). In extension, both the accessory collateral ligament and the volar plate are taut becoming the principal restraints to valgus stress in this position.
motion. Thumb MP joint stability is provided by the bony anatomy as well as dynamic and static restraints. Compared with the finger metacarpals, the thumb metacarpal head is less spherical and its cartilage is more limited on the dorsal aspect leading to further stability (5). The static restraints are the proper and accessory collateral ligaments, the palmar plate, and the dorsal capsule. The proper collateral ligament extends from the midaxis of the metacarpal head to the palmar aspect of the proximal phalanx (Fig. 8-1). Along with the dorsal capsule, this ligament is taut in flexion. The proper collateral ligament serves as the primary restraint to valgus stress with the MP joint flexed and prevents palmar subluxation of the proximal phalanx. The accessory collateral ligament is palmar to and contiguous with the proper collateral ligament at the metacarpal head and inserts onto the volar plate (Fig. 8-2). In extension, both the accessory collateral ligament and the volar plate are taut becoming the principal restraints to valgus stress in this position.
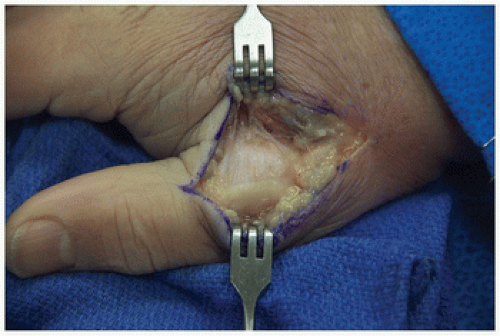
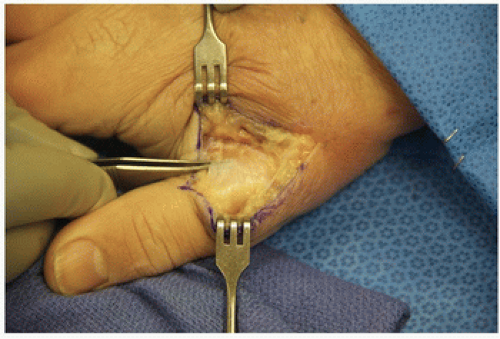
The dynamic stabilizers include the extrinsic (extensor and flexor pollicis longus, extensor pollicis brevis) and intrinsic (abductor and flexor pollicis brevis, adductor pollicis) tendons and muscles. The adductor mechanism plays an important role as a dynamic stabilizer. Via its aponeurosis, it
inserts onto the extensor expansion superficial to the MP joint capsule and UCL (Figs. 8-3 and 8-4). The adductor also has a deep insertion to the palmar aspect of the proximal phalanx via the ulnar sesamoid bone. Several structures can be injured after an acute valgus stress to the thumb MP joint. There may be a rupture of the dorsal capsule, volar plate, adductor mechanism, and extensor pollicis brevis. The thumb will be stable to valgus stress testing when these structures alone are involved. In contrast, when the proper collateral ligament is torn, instability will be present when the thumb is stressed in flexion. When the accessory collateral ligament is also torn, the tear is complete and the MP joint will be unstable in extension and flexion.
inserts onto the extensor expansion superficial to the MP joint capsule and UCL (Figs. 8-3 and 8-4). The adductor also has a deep insertion to the palmar aspect of the proximal phalanx via the ulnar sesamoid bone. Several structures can be injured after an acute valgus stress to the thumb MP joint. There may be a rupture of the dorsal capsule, volar plate, adductor mechanism, and extensor pollicis brevis. The thumb will be stable to valgus stress testing when these structures alone are involved. In contrast, when the proper collateral ligament is torn, instability will be present when the thumb is stressed in flexion. When the accessory collateral ligament is also torn, the tear is complete and the MP joint will be unstable in extension and flexion.
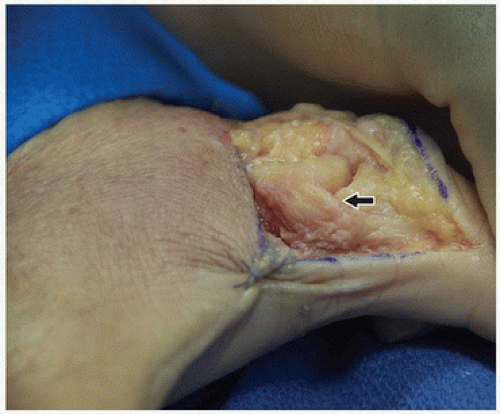
Thumb UCL ruptures can occur at the midsubstance, proximally or distally. Distal avulsion off the base of the proximal phalanx is most common and can lead to a Stener lesion. This lesion occurs when the UCL is avulsed distally from the base of the proximal phalanx and displaces proximal and superficial to the adductor aponeurosis (6). The adductor aponeurosis becomes interposed between the torn UCL and its insertion at the base of the proximal phalanx, preventing it from healing in the correct anatomic location. Many feel this is the essential pathoanatomy determining the need for operative intervention.
PREOPERATIVE PLANNING
Patients will present with persistent pain, swelling, and frequently ecchymosis of the thumb. They complain about weakness with pinching or gripping activities and may demonstrate frank instability. Physical examination reveals localized swelling and often radial deviation and palmar subluxation of the proximal phalanx. A lump along the ulnar aspect of the thumb at the level of the metacarpal head may be palpated, which is highly suggestive of a Stener lesion. However, lack of a palpable mass does not rule out a Stener lesion (7). After palpation of the joint and before stability testing, anteroposterior and lateral radiographs are obtained to determine whether an avulsion fracture is present, typically from the ulnar base of the proximal phalanx. Associated fractures of the thumb metacarpal may also occur. After careful assessment of the radiographs, evaluation of joint stability with valgus stress testing is the most critical part of the examination. The goal is to determine whether the injury is incomplete (grade 1 or 2) or complete (grade 3). Testing stability in full extension and 30 degrees of flexion places the accessory and proper ligaments under tension, respectively. Carefully align the MP joint before stress testing because the thumb may already have assumed an angular posture secondary to ligamentous injury, thus influencing the measurement/severity of instability.
Grade 1 injury is a sprain without joint instability.
Grade 2 injury is an incomplete tear with joint instability but with a firm endpoint on stress testing. A firm endpoint and less than 30 degrees of valgus laxity rules out a complete UCL tear.
Grade 3 injury is a complete tear with an unstable joint and no endpoint on stress testing. In complete ruptures, a Stener lesion is more than 80% likely (7).
Instability is defined as opening of the joint more than 30 to 35 degrees without a firm endpoint (or 15 degrees more than the contralateral thumb) at both full extension and 30 degrees of flexion.7 Assessing the stability in flexion tests the proper collateral ligament, and stressing the joint in extension tests the accessory collateral ligament and volar plate.
Valgus stress testing should not be avoided for fear of displacing a nondisplaced ligament rupture or avulsion fracture. The location of the bony fragment does not indicate the ligament location, nor does it indicate joint stability. Furthermore, if the ligament was not displaced at the time of an uncontrolled injury, controlled stress testing should not cause the ligament to displace.
Other imaging studies, such as arthrogram, ultrasonography, and magnetic resonance imaging, can provide further sensitivity and specificity in the diagnosis of UCL tears; however, these are rarely required for accurate diagnosis.
INDICATIONS/CONTRAINDICATIONS
Grade 1 and 2 UCL injuries are managed conservatively in a splint or thumb spica cast with the interphalangeal (IP) joint free for immediate range of motion (ROM).
Immobilization of the MP joint is maintained for 3 to 6 weeks (8).
Active and passive ROM can be started either immediately or after immobilization if radial deviation is avoided.
Strengthening, gripping, and pinching activities are initiated at 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree