Thoracoscopic Release and Fusion for Scoliosis
Daniel J. Sucato
Matthew D. Abbott
DEFINITION
Thoracoscopy provides the ability to gain access to the thoracic spine via small incisions (portals).
Anterior release includes removal of the annulus fibrosus, anterior longitudinal ligament, nucleus pulposus, and, if necessary, the rib head.
Scoliosis is a lateral curvature of the spine with axial plane rotation.
Fusion is the healing of two vertebral bodies together, usually fused by bone graft or bone graft substitute.
ANATOMY
The thoracic spine spans from the first thoracic vertebra (T1) to the 12th thoracic vertebra (T12).
The rib head attachment to the vertebral body is more anterior in the proximal thoracic spine than the distal thoracic spine.
The annulus fibrosus is the circumferential fibrous tissue that surrounds the nucleus pulposus, which is in the center of the disc.
The anterior longitudinal ligament, which runs on the anterior aspect of the vertebral body, is a strong fibrous tissue that is contiguous throughout the spine. The segmental arteries and veins originate from the aorta and vena cava, respectively, and traverse the vertebral body. The parietal pleura of the chest surrounds the thoracic spine, covering the segmental vessels and the disc and vertebral bodies. The anterior, middle, and posterior axillary lines run (in reference to the axilla) in the anterior, middle, and posterior aspects of the axilla. Scoliotic deformity in the thoracic spine is lateral curvature with axial plane rotation as well as hypokyphosis (idiopathic scoliosis).
The arch of the aorta and the arch of the azygos vein typically are located at the T4-T5 levels.
PATHOGENESIS
Scoliosis can be grouped into many categories based on pathogenesis.
The most common type of scoliosis seen is idiopathic, in which the etiology and pathogenesis are unknown.
Theories of pathogenesis include hormonal influences, growth disturbance, genetic factors, muscle imbalance, and proprioception and balance abnormalities.
Other types of scoliosis include the following:
Congenital: abnormal vertebra due to failure of formation or segmentation
Neuromuscular: for example, cerebral palsy, Duchenne muscular dystrophy, spinal muscular atrophy
Neurogenic: for example, neurofibromatosis, spinal cord injury
NATURAL HISTORY
An idiopathic scoliosis curve may progress in two ways:
With continued spine growth
When curve magnitude is greater than 50 degrees at skeletal maturity
Curve progression can be rapid during spine growth or slow following skeletal maturity (approximately 1 degree per year).
Curve magnitudes above 80 to 90 degrees in the thoracic spine may result in symptomatic pulmonary issues.
Large curves in adulthood can result in pain.
PATIENT HISTORY AND PHYSICAL FINDINGS
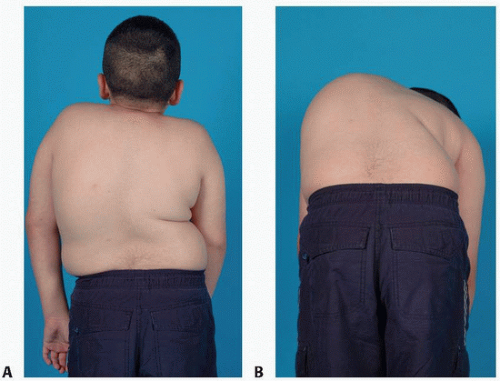
The examination for spine deformity should include standing visualization of the spine to look for shoulder height differences, waist asymmetry, overall trunk balance, or coronal head imbalance (FIG 1).
Further information is obtained as to the character of the pain (eg, sharp, dull, aching), when the pain occurs (eg, during activity, while attempting to sleep, pain waking from sleep), and the location of the pain (eg, upper, middle, lower back) as well as whether it radiates into the lower extremities.
Other history should include any information on other neurologic symptoms such as bowel or bladder incontinence.
Sensory symptoms should be elicited, especially with hyperesthesias along the chest wall or upper or lower extremities.
Cutaneous manifestations of dysraphism should be analyzed.
The neurologic examination should include motor strength and a sensory examination of the upper and lower extremities.
The abdominal reflexes are the most important neurologic assessment. They are assessed by stroking the skin adjacent to the umbilicus on the left and right and upper and lower quadrants and should be symmetrically absent or present. When asymmetric, magnetic resonance imaging (MRI) is necessary to evaluate for neural axis abnormalities.
The lower extremities should be carefully examined for asymmetry with respect to size and strength of the legs as well as foot deformities (eg, cavovarus foot deformities) as an indication for the presence of neural axis abnormalities.
Deep tendon reflexes and the Babinski reflex should be investigated.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiography should include a standing posteroanterior (PA) and lateral radiograph of the spine to include the cervical spine to the pelvis and hips.
The PA radiograph (FIG 2A) should be evaluated for the following:
Coronal plane deformities using the Cobb method
The C7-center sacral vertebral line (CSVL) placement
A trunk shift using Floman method (the distance between the CSVL and the mid-distance between the lateral rib margins)
Evaluation for any congenital abnormalities (eg, hemivertebra, congenital bar)
The Risser stage (0 through 5)
The status of the triradiate cartilage (open or closed)
The lateral radiographs (FIG 2B) should be analyzed to determine the following:
Thoracic kyphosis and lumbar lordosis
Presence of associated spondylolisthesis or spondylolysis
Sagittal balance (distance between C7 plumb line and the posterior edge of the first sacral vertebral body)
The Stagnara view is an oblique view to the patient, but an orthogonal view to the coronal curve that is used in severe spinal deformities to better visualize the spine.
Indications for MRI include neurologic abnormalities, significant back pain associated with scoliosis, atypical curve patterns such as a left thoracic curve, very young age, congenital scoliosis, neurofibromatosis, Marfan disease.
Computed tomography (CT) scanning may be useful to fully define the osseous anatomy, especially for extremely large curves and congenital curves.
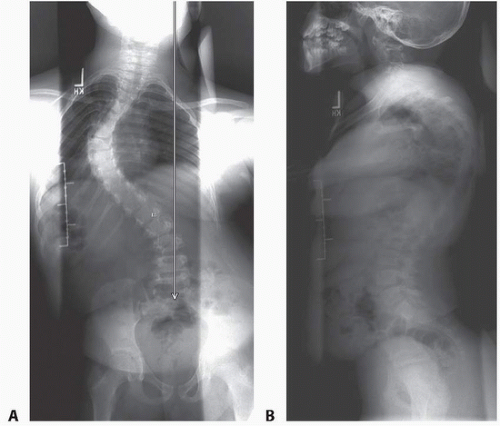 FIG 2 • A,B. Preoperative anteroposterior (AP) and lateral radiographs demonstrate a 93-degree left thoracic scoliosis with a large trunk shift and open triradiate cartilage in the patient shown in FIG 1. |
DIFFERENTIAL DIAGNOSIS
Idiopathic scoliosis
Congenital scoliosis
Neurofibromatosis
Scoliosis associated with Marfan disease
NONOPERATIVE MANAGEMENT
Nonoperative management has little or no role for severe deformity.
Patients who are very young with moderate deformity may be treated with a brace to buy time to allow the patient to grow.
Bracing can be effective to prevent curve progression for smaller idiopathic curves (ie, 25 to 40 degrees).
SURGICAL MANAGEMENT
Anterior thoracoscopic release for spinal deformity has many technical considerations, which are discussed later in this chapter.
Indications for an anterior release/fusion
Severe spinal deformity: scoliosis greater than 80 to 90 degrees with significant rotational deformity or kyphosis greater than 100 degrees with flexibility index less than 50%
Skeletal immaturity, to avoid the crankshaft phenomenon. Usually performed for children younger than 10 years of age with open triradiate cartilage and Risser grade 0. Thoracoscopy has been shown to be safe in children less than 20 kg weight.
Deficient posterior elements, so that a posterior fusion may be difficult. Such deficiencies occur secondary to previous surgery with laminectomies for tumors or the treatment of neural axis abnormalities.
Preoperative Planning
Each patient should be carefully analyzed with respect to those curves that will undergo an anterior release.
The radiograph should be viewed to determine preoperatively which levels should be released. Release always includes the apical levels and usually includes all of the levels within the Cobb measurement.
For severe curves, traction in the operating room may be helpful in assisting curve correction.
Positioning and Approach
Lateral Position
Advantages
More familiar and traditional approach
Conversion to open procedure is easy.
All thoracic levels can be accessed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree