Revision Cervical Surgery
Casey C. Bachison
Harry N. Herkowitz†
†Deceased.
DEFINITION
In recent years, the number of patients undergoing cervical spine surgery has risen dramatically. Cervical spine surgery is used to treat a number of common spinal pathologies including the following:
Cervical spinal stenosis
Deformity
Disc herniation
Myelopathy
Trauma
Pathologic conditions such as neoplasia, infection, and metabolic and inflammatory disease
The surgical procedures used to treat these conditions are generally successful but occasionally result in complications that require revision cervical spine surgery. Unexpected life events after spine surgery such as trauma and cancer can cause instability or neurocompression leading to the need for surgical decompression and/or stabilization at the site of previous operative intervention. The more common complications and conditions are defined here.
Pseudarthrosis: The term suggests a “false joint.” Pseudarthrosis is a failure of bone fusion or nonunion at the site of attempted arthrodesis. Diagnosis is made after 6 months to 1 year following the index surgery. Pseudarthrosis may occur following anterior or posterior cervical procedures.
Adjacent segment degeneration (ASD) occurs when there are degenerative changes at unfused levels adjacent to prior cervical fusion. ASD is believed to result from excessive motion at the level adjacent to an arthrodesis as it compensates for the fused segment. Some controversy exists whether the degeneration occurs as a result of prior arthrodesis or as a result of natural progression in an individual already prone to degenerative disc disease.
Postlaminectomy kyphosis (PLK) is a kyphotic deformity of the cervical spine that develops as a result of previous surgery in which the posterior elements of the spine, including the spinous process and lamina, were removed. Removal of the posterior tethering structures, including the spinous processes and the associated supraspinous and interspinous ligaments, predisposes individuals to this condition.
Hardware/construct failure: Plates, screws, and rods may loosen or break if bone healing is prolonged or inhibited. Allograft and autograft bone used for structural support of the spine are subject to loading forces that can cause the graft to collapse. Poor bone quality in the patient may allow hardware to migrate or bone graft to subside.
Same segment disease/residual compression is persistent or recurrent pain is present at the level of previous decompression. Same segment disease results from failed stabilization or inadequate decompression at the site of the initial cervical surgical procedure.
Pathologic conditions may be the inciting event for the index surgical procedure or may result in the need for revision surgery. Tumor, infection, trauma, and inflammatory conditions such as rheumatoid arthritis and ankylosis spondylitis may lead to instability, deformity, or neurocompression after an index cervical procedure.
ANATOMY
Vertebrae
The cervical spine consists of seven specialized vertebrae.
Transverse foramina are present bilaterally for the passage of the vertebral artery.
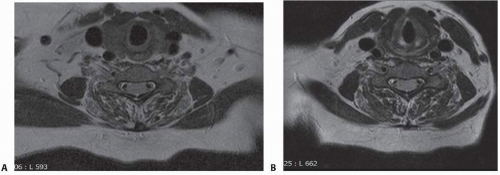
The vertebral artery generally enters the cervical spine at C6. Occasionally, it will enter at C7 or C5. The artery may also enter the spine at different levels on either side of the cervical spine in the same patient. Magnetic resonance imaging (MRI) should be obtained prior to surgical intervention to ascertain the site of vertebral artery entry and any anomalies present along its excursion (FIG 1).
The spinous processes of C6-C2 are bifid. C7 does not possess a bifid spinous process but is more prominent than the other cervical vertebrae. C7 is often referred to as vertebra prominens.
Discs
An intervertebral disc is present between each of the cervical vertebrae from C2 through T1.
The occiput to C1 and the C1-C2 articulation do not have intervertebral discs and articulate through true synovial joints.
Each disc consists of an outer annulus fibrosus and inner nucleus pulposus.
Between the annulus fibrosus/nucleus pulposus complex and the vertebral body, a cartilaginous endplate is present. The removal of this cartilaginous endplate is pivotal to a successful interbody arthrodesis. Failure to remove the cartilaginous endplate increases the likelihood of pseudarthrosis.
Ligaments
A supraspinous ligament runs dorsally over the top of the spinous processes.
Then, an interspinous ligament is present between two spinous processes at each level.
An anterior longitudinal ligament runs along the front of the spine adherent to the ventral aspect of the vertebral body.
A posterior longitudinal ligament (PLL) runs along the dorsal aspect of the vertebral body and intervertebral discs. It forms a barrier between the discs and the dura/spinal cord.
Normal lordosis of the cervical spine averages 14.4 degree.27
Weight-bearing axis of the cervical spine passes through the posterior column.18
Loss of the posterior tension band after resection of the lamina and spinous processes may lead to kyphosis and a shift in the weight-bearing axis of the spine to the anterior column.
PATHOGENESIS
Pseudarthrosis
Pseudarthrosis occurs when bone fails to form at the site of attempted arthrodesis. Multiple factors may play a role in the formation of pseudarthrosis.
Risk factors include the following28:
Multilevel fusions
Metabolic abnormalities
Smoking
Infection
Excessive motion
Smoking is associated with lower fusion rates in cervical and lumbar fusion. Hilibrand et al9 found a higher rate of fusion in nonsmokers (81%) than in smokers (62%). In contrast to the effect of smoking on anterior cervical fusion, some studies found smoking did not decrease posterior cervical fusion with lateral mass instrumentation and iliac crest bone grafting.
Excessive motion at the site of an anterior cervical discectomy and fusion (ACDF) is associated with increased rates of pseudarthrosis. Use of anterior cervical plating has been shown in multiple studies to decrease the rate of pseudarthrosis.4,23
Corpectomy with the use of autogenous strut grafting should be considered when a multilevel anterior cervical decompression and fusion is performed in patients who are unable or unwilling to stop smoking prior to surgical treatment.9
ASD
As previously noted, some controversy exists whether the degeneration of adjacent segments occurs as a result of prior arthrodesis, which may place increased demands on a level above or below a fusion, or whether the degeneration is a result of natural progression in an individual already prone to degenerative disc disease.
Deformity (PLK)
Causes of PLK include the following:
Removal of the posterior restraints of the cervical spine, namely posterior bony arch and the supraspinous and interspinous ligaments. Resection of greater than 50% of the facet has been shown to lead to instability.17
Attenuation or failure of the restraints secondary to radiation
Neglect of deformity during index procedure
Removal of the posterior arch/facets leads to instability, which causes the weight-bearing axis of the spine to shift anteriorly.
Once the axis shifts anteriorly, the posterior cervical musculature fatigues and the kyphosis progresses.1
The load is then transferred to the anterior vertebral bodies and discs.
The likelihood of hardware failure of current cervical instrumentation is small.
Anterior cervical hardware or construct failure is an infrequent occurrence; however, complication associated with hardware placement occurs in approximately 22% to 36% of cases.2
Screw breakage or loosening is often the result of a nonunion or pseudarthrosis, and evaluation of the fusion with flexion-extension views or computed tomography (CT) scan is warranted.
Infection, osteoporosis, tumor, and trauma can also lead to hardware failure or graft subsidence after cervical fusion with or without instrumentation.
The use of multilevel interbody fusion versus corpectomies with strut grafting has been shown to decrease the risk of graft extrusion.
Aggressive mobilization and smoking are other potential causes for prolonged healing and hardware failure.
Same segment disease/residual compression
A result of failed or inadequate initial surgical decompression
Truumees and McLain24 outlines four general causes for residual compression after cervical surgery. These are the following:
Failure to perform a complete decompression at the injured/involved level
Failure to decompress adjacent involved levels
Migration of graft or fixation materials into the canal or foramen
Pathologic conditions
The pathogenesis of tumor, infection, and inflammatory conditions such as rheumatoid arthritis and ankylosis spondylitis is beyond the scope of the current text. Failure of the cervical spine as it relates to these conditions is a progressive deterioration of the structural integrity of the bones or erosion of the ligamentous support of the spine. Loss of these structures leads to instability, deformity, or compression of the neural elements.
NATURAL HISTORY
Pseudarthrosis
Lowery et al16 defined pseudarthrosis as follows:
Continued or worsening axial pain 6 months after the initial procedure
Complete radiolucency at the host/graft interface
Vertebral body motion greater than 2 mm on flexion and extension films
Phillips et al18 followed 48 patients with radiographic pseudarthrosis:
Thirty-two patients (67%) developed symptoms.
Sixteen patients remained asymptomatic for 5.1 years.
Nine of the 32 symptomatic patients were pain free for 2 years before trauma caused development of symptoms.
Eighty-two percent of patients developed pseudarthrosis at the most caudal level after multilevel fusion.
Revision surgery led to good or excellent results in all cases (anterior or posterior).
Allograft and multilevel fusion increases the risk of pseudarthrosis.13
Posterior fusion with lateral mass screws leads to high rate of fusion from 0% to 1.4%; less rigid posterior fixation (wiring) has a less reliable outcome.
ASD
Occurs at a rate of 2.9% per year, with 25% of patients developing ASD within 10 years8
Patients with degenerative changes at C5-C6 or C6-C7 at time of initial procedure are at greatest risk for development of ASD.
Eck et al5 measured disc pressures at C4-C5 and C6-C7 before and after simulated fusion at C5-C6 and found a 73% increase in cranial and 45% in caudal disc pressures during flexion.
Deformity (PLK)
Lonstein14 described PLK as a focal, dramatic angulation of the cervical spine after posterior decompression.
Kyphosis is the most common cervical deformity and the most frequent cause is iatrogenic postlaminectomy instability.
Patients with PLK generally have a pain-free period following the index surgical procedure followed by the development of persistent pain.
Risks of PLK as described by Lonstein14:
Age younger than 30 years
Aggressive facetectomy
Removal of more than four laminae
Preoperative deformity
Tumors
Removal of C2 posterior elements (major semispinalis insertion)
Paraspinal muscle weakness
Anterior instability following fracture
Nowinski et al17 studied the effects of progressive facetectomy and recommend posterior fusion when over 25% of the facets are sacrificed for decompression. Some studies found a 25% incidence of kyphosis in patients with bilateral facet resection.
Facet capsular resection of greater than 50% increases the risk of progressive deformity.27
Hardware/construct failure
Hardware complications following ACDF have been characterized in 22% to 36% of cases.12
Graft extrusion and malalignment have been described in up to 6% of cases following anterior cervical fusions.12
When failure occurs, the risk of injury to the tracheoesophageal structures is minimal.15
Immediate removal of failed hardware is rarely necessary and should only be considered if there is evidence of dysphagia or risk to the spinal cord or nerve roots.
Careful and long-term follow-up in patient with loose or broken hardware assures that significant progression of the failure does not occur.
Same segment disease/residual compression
Results from failed or inadequate initial surgical procedure
ACDF, posterior cervical fusion, posterior foraminotomy, and micro-ACD ranged from 5% to 36%.12
Hardware complications following ACDF have been characterized in 22% to 36% of cases.
Residual compression after an index spine procedure may result from the following24:
Failure to perform a complete decompression at the injured/involved level
Failure to decompress adjacent involved levels
Migration of graft or fixation materials into the canal or foramen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree