Transforaminal and Posterior Lumbar Interbody Fusion
Saad B. Chaudhary
Mitchell F. Reiter
DEFINITION
Several arthrodesis techniques are available to address the various pathologic processes in the lumbar spine.
The standard lumbar arthrodesis techniques include the following:
Anterior lumbar interbody fusion (ALIF)
Posterior spinal fusion (PSF), which includes two subtypes
Posterior interlaminar and facet fusion
Posterior lateral intertransverse fusion
Combined anterior and posterior fusion (AP fusion or 360-degree fusion)
Posterior lumbar interbody fusion (PLIF) and its variant, the transforaminal lumbar interbody fusion (TLIF)
The PLIF procedure uses a posterior approach to the spine that involves radical discectomy and endplate preparation combined with an interbody fusion using a structural graft or cage with or without supplemental posterior instrumentation.
The TLIF procedure is similar to PLIF with the modification that the interbody region is accessed unilaterally via a more lateral approach in conjunction with pedicle screw instrumentation.
PLIF and TLIF are versatile techniques that offer several advantages over the other fusion methods.3
They allow for pathology in all three columns of the spine to be addressed and for a circumferential fusion to be achieved through a single posterior approach.
They directly address the disc as a potential pain generator in patients with discogenic pain syndromes.
They have demonstrated a high rate of fusion that approximates the arthrodesis rate achieved with a more extensive combined AP fusion procedure.
They allow for direct decompression of the spinal canal if necessary.
They facilitate correction of spinal deformities, including asymmetric disc space collapse, spondylolisthesis, and mild kyphosis.
PLIF and TLIF procedures also avoid some of the drawbacks inherent to ALIF procedures, such as the following:
Vascular injury, higher rates of thromboembolic disease, and retrograde ejaculation in males
PLIF and TLIF have the disadvantage, however, of potential nerve root injury from preparation and instrumentation of the disc space through a posterior approach.
ANATOMY
The standard posterior approach to the lumbar spine is used for posterior interbody fusion techniques.
Applied surgical anatomy considerations for TLIF and PLIF are nearly identical, with both techniques using a midline incision and standard posterior exposure.
Both PLIF and TLIF techniques require interbody access via a posterior annulotomy.
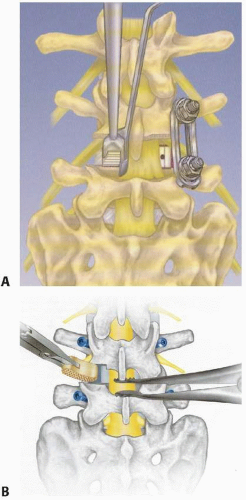
The major difference is that the PLIF procedure uses a bilateral and more medial approach to access the interbody region, whereas the TLIF technique involves a unilateral approach with complete removal of one facet joint to allow more lateral access to the disc space (FIG 1).
As a result, the exiting root is at a greater risk when performing a TLIF, whereas the traversing root and thecal sac are at greater risk with a PLIF.
A masterful understanding of the triangular working window to the annulus and the local neurologic anatomy is critical in order to safely execute the TLIF or PLIF procedure.
The triangular working window consists of the following:
The traversing nerve root and thecal sac form the medial border of the triangle.
The exiting nerve root from the proximal vertebral level forms the lateral border (eg, L4 for an L4-L5 TLIF or PLIF).
The superior aspect of the pedicle of the distal vertebra forms the base of the triangle.
A confluence of epidural veins traveling longitudinally and transversely drapes the floor of the spinal canal and neuroforamen.
With careful exposure, a triangular working window measuring up to 1.5 cm wide and of slightly greater height can be created.
A noncollapsed disc space of an adult lumbar spine averages between 12 and 14 mm in height, with an anteroposterior diameter of about 35 mm.5
PATHOGENESIS
The PLIF and TLIF techniques are most commonly used when addressing the degenerative pathologies of the lumbar spine. The pathophysiologic discussion of the degenerative cascade is beyond the scope of this chapter and is touched upon elsewhere in this book.
Common pathologies include the following:
Spondylolisthesis
Adult deformity
Recurrent disc herniation
Degenerative disc disease/discogenic back pain
The PLIF and TLIF procedures allow for fusion of the anterior column of the spine in the interbody region, which offers several biologic and biomechanical advantages over PSFs:
The anterior column of the spine is known to support 80% of the body’s compressive load; consequently, intervertebral structural grafts are subjected to compressive loading, which facilitates arthrodesis.
Because interbody structural grafts are load-sharing, they significantly reduce the cantilever bending forces applied to posterior spinal implants, thus protecting them from failure.
The interbody space has been shown to provide an optimal milieu for promoting arthrodesis for several reasons:
A large surface area of highly vascular cancellous bone is available.
The disc space represents a relatively shorter gap to span when compared to intertransverse fusion.
The outer annulus serves as a barrier that reduces fibrous tissue ingrowth into the fusion mass during healing of an interbody arthrodesis.
INDICATIONS
Discogenic pain syndromes due to internal disc disruption or degeneration as well as postdiscectomy chronic low back pain are well suited to PLIF or TLIF for several reasons:10,13
These procedures directly address the disc as the pain generator and have been shown to have superior clinical outcomes in treating discogenic pain compared to isolated PSFs, which do not remove and fuse the painful disc.
They allow for restoration of interbody height and some correction of local kyphosis without putting undue stress on the posterior implants.
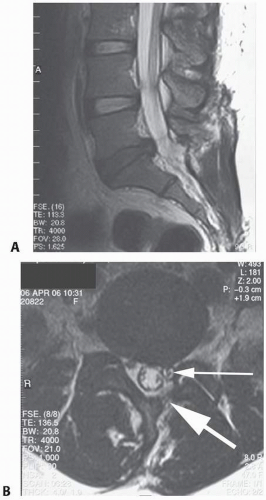
They permit decompression of the exiting and traversing nerve roots indirectly by restoring foraminal height and directly via open laminectomy and foraminotomy. Because of this, PLIF and TLIF are ideally suited to patients with discogenic pain syndromes occurring in conjunction with radicular symptoms caused by herniated disc pathology or stenosis (FIG 2).
Low-grade isthmic spondylolisthesis can also be treated successfully with PLIF and TLIF procedures as an alternative to performing a combined AP fusion.11
In addition to direct and indirect decompression of neural elements, PLIF and TLIF raises the arthrodesis rate over stand-alone posterior fusion.
When clinically indicated and with proper instrumentation, PLIF and TLIF allow for reduction of the spondylolisthesis and slip angle, with restoration of lordosis. In experienced hands and in conjunction with a wide decompression and intraoperative neurologic monitoring, some higher grade spondylolistheses can also be successfully reduced and stabilized with the PLIF and TLIF procedures.
PLIF and TLIF procedures can be a useful adjunct to adult deformity surgeries such as degenerative scoliosis and spondylolisthesis and offer several advantages:
They can be used to provide anterior column support at the caudal end of fusion constructs and the lumbosacral junction without requiring an additional anterior approach to the spine.
They improve the arthrodesis rate, which can be helpful when an interlaminar fusion is not possible because a midline decompression was necessary to address spinal stenosis.
They allow for some additional deformity correction by releasing asymmetrically collapsed disc spaces and providing interbody structural support.
PLIF and TLIF can also help raise the fusion rate in clinically challenging situations posing a high risk for nonunion, such as:
Patients unwilling or unable to quit smoking
Patients with diabetes mellitus or on systemic corticosteroids
Patients on chemotherapy or with an irradiated fusion bed
Revision spinal fusion procedures in which the posterolateral fusion bed is fibrotic and hypovascular
CONTRAINDICATIONS
PLIF should not usually be attempted at the level of the conus medullaris (typically L1-L2) or above, and great caution must be taken using the TLIF procedure at the level of the cord or conus.
Severe osteoporosis is a relative contraindication to these procedures as disc space preparation can result in major endplate violations with subsequent implant subsidence.
Anomalous neural anatomy such as a conjoined nerve root can make the performance of a PLIF or TLIF procedure impossible.
Even in some cases of “normal” nerve root anatomy, local variations in takeoff angles of the exiting and traversing roots can place the roots at risk during interbody approaches. Caution should be exercised in such cases and interbody fusion abandoned if not felt to be safe.
Severe focal kyphosis is poorly addressed with a PLIF or TLIF procedure and is usually better treated with an anterior procedure that allows for release of the anterior longitudinal ligament and annulus fibrosus.
Irreducible higher grade spondylolistheses are not well treated with the PLIF and TLIF procedures as the surface area of the opposing vertebral endplates is minimized.
Severe epidural fibrosis and an active infectious process can result in dural tears, neurologic injury, and possible meningitis.
NONOPERATIVE MANAGEMENT
Before considering PLIF and TLIF surgeries, standard nonoperative management options for the pathologic conditions being addressed should typically be exhausted.
Nonsurgical treatment usually involves a combination of analgesic medications, physical therapy, and activity and lifestyle modification. When applicable, interventional pain management techniques such as trigger point injections, facet blocks, or epidural steroid injections should be considered.
Surgical intervention is usually reserved for patients who remain symptomatic despite several months of nonoperative treatment and whose symptoms are severe enough to justify the risks associated with operative care.
SURGICAL MANAGEMENT
As mentioned earlier, PLIF and TLIF procedures are capable of addressing a wide variety of pathologic conditions and, in specific situations, offer several compelling advantages.
Given their versatility, the well-trained spinal surgeon needs to be aware of the indications for these procedures and must be capable of executing them properly.
Although the usefulness of the PLIF and TLIF procedures is clear, one must remain mindful that these procedures are technically demanding and should be undertaken only after careful training and preoperative planning and with meticulous surgical technique.
Preoperative Planning
Preoperative imaging studies should be reviewed to determine the appropriate size and trajectories necessary for pedicle screw insertion as well as the anteroposterior diameter of the disc space.
Disc space height as well as adjacent disc height and overall lumbar alignment should be measured to help determine optimal interbody implant size.
An assessment should be made whether direct or indirect neurologic decompression will be necessary.
When using the TLIF technique, the interbody approach should be performed on the patient’s symptomatic side if he or she has radicular complaints or from the side of maximal neurologic compression if the lower extremity symptoms are of equal severity.
Although sometimes difficult to assess, the patient’s magnetic resonance imaging (MRI) needs to be studied carefully to identify anomalous neural anatomy such as a conjoined nerve root.
If a conjoined nerve root is suspected, the TLIF should be performed from the opposite side, and the patient should be counseled preoperatively that the interbody portion of the procedure may not be possible because the contralateral side may demonstrate intraoperative nerve root anomalies as well.
For the PLIF procedure, the presence of a conjoined nerve root usually necessitates a unilateral PLIF. If identified preoperatively, conversion to a TLIF should be strongly considered.
Deformity at the level of the planned fusion needs to be assessed so that intraoperative measures can be taken to provide for correction.
Positioning
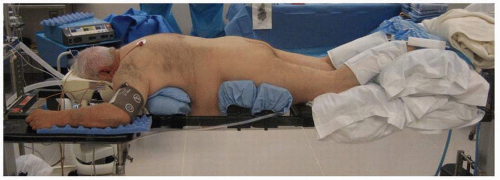
The patient should be positioned prone on an operating room table that allows for fluoroscopic imaging, such as a Jackson spine table (FIG 3).
The abdomen should be free to decompress the vena cava. This maneuver has been found to reduce epidural venous engorgement and bleeding.
A Foley catheter and lower extremity sequential compression devices should be used routinely.
Pillows should be used to keep the knees slightly flexed to minimize tension on the lumbar nerve roots.
Intraoperative physiologic monitoring with somatosensory evoked potentials and “free running” electromyographic monitoring should be considered. Physiologic monitoring will also allow for pedicle screw stimulation testing to help detect any inadvertent pedicle wall breaches.
Approach
The standard posterior approach to the lumbar spine is used, including exposure out to the tips of the transverse processes so that an adequate intertransverse fusion can be performed.
Some surgeons choose to perform a more limited dissection and do not perform the posterolateral portion of the fusion, hoping that by preserving the blood supply and muscular attachments in the intertransverse region, there will be reduced erector muscle dysfunction and fibrosis with improved outcomes.
Minimally invasive TLIF options have been developed and are described in Chapter 19.
For the standard TLIF procedure, the spinous processes and interspinous ligaments can usually be left intact. Preserving these structures minimizes epidural scarring and provides a larger surface area for the posterior fusion.
If decompression of the contralateral side of the spinal canal is required, the TLIF procedure can be modified to include a central laminectomy.
Two exposure options exist for the PLIF procedure, each of which will be discussed in more detail later in the chapter:
Extensive resection, including wide laminectomy with bilateral facetectomies
Limited resection using bilateral laminotomies and medial facetectomies
TECHNIQUES
▪ Transforaminal Lumbar Interbody Fusion
Pedicle Screw Insertion
After exposure, pedicle entry points are identified at the junction of the transverse process with the superior articular process of each vertebra.
A high-speed burr or awl is then used to access each pedicle, followed by use of a pedicle probe and tap to create a proper path for the screws.
Polyaxial pedicle screws are then placed bilaterally in the standard fashion.
Fluoroscopy or image guidance systems and electromyographic responses can be used to aid in proper screw positioning.
If desired, the transverse processes can be decorticated using a high-speed burr or curette before screw insertion. This is recommended to facilitate the posterior arthrodesis as access to the transverse processes becomes somewhat limited once the pedicle screws are in place.
Disc Space Distraction
After screw placement, the next step is to provide posterior distraction to open the posterior portion of the disc space.
Lumbar disc spaces are normally lordotic, which can make insertion of an appropriate-sized interbody cage through the narrow posterior portion of the disc space difficult.
With distraction, the disc space alignment can be neutralized, thereby facilitating access to the interbody region with minimal bony resection.
Several methods of achieving interbody distraction exist, and these can be combined as needed to achieve the desired alignment. The choice of distraction technique is largely based on surgeon preference, as all three methods have been found to be effective.
Distraction option 1: use of rods and screws
Rods can be loaded bilaterally into the pedicle screws, followed by provisional placement of the system’s locking nuts. However, unilateral rod insertion on the contralateral side alone is preferred for unencumbered disc space approach and preparation.
Distraction is then carried out using the rod(s) and a standard distractor (TECH FIG 1A-C).
To allow for the distraction, the rods need to be slightly longer than will ultimately be necessary.
If bilateral rod placement is considered, the polyaxial screw heads should be angled as laterally as possible to maximize the volume of space medial to the rods. This maneuver facilitates later access to the disc space without requiring rod removal.
Alternatively, several systems have pedicle screw distractor instruments that provide distraction off the screws obviating rod insertion.
Lateral fluoroscopy should be used to judge the amount of distraction obtained at the posterior margin of the disc space.
Once adequate alignment is obtained, the system’s locking nuts are tightened to maintain the distraction.
Care should be taken not to excessively distract off the screws in osteoporotic patients as this could lead to screw loosening.
Distraction option 2: spinous process distraction
Distraction can also be achieved by using a lamina spreader placed between the spinous processes (TECH FIG 1D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree