The Wrist 
The wrist is a complex arrangement of multiple bones, ligaments, and cartilage, which bridges the hand with the forearm, and allows for a significant degree of physiologic motion. Being central to the majority of daily living activities, wrist is one of the most commonly injured sites of the musculoskeletal system. The wrist is composed of the following.
 The carpus, comprising eight bones, which are arranged in two rows and articulate among themselves in a manner of three-dimensional cohesion, forming the midcarpal and intercarpal joints
The carpus, comprising eight bones, which are arranged in two rows and articulate among themselves in a manner of three-dimensional cohesion, forming the midcarpal and intercarpal joints
 The radiocarpal and ulnocarpal joints
The radiocarpal and ulnocarpal joints
 The distal radioulnar joint (DRUJ) compartment, in which the distal radius articulates with the adjacent ulna
The distal radioulnar joint (DRUJ) compartment, in which the distal radius articulates with the adjacent ulna
 The five carpometacarpal (CMC) joints, in which the carpus articulates with the metacarpal bones
The five carpometacarpal (CMC) joints, in which the carpus articulates with the metacarpal bones
Whereas the CMC joints can communicate with the midcarpal and intercarpal joints, the radiocarpal joint and DRUJ are tight isolated compartments.
The inherently unstable structure of the wrist is balanced by multiple intrinsic (intercarpal) and extrinsic (connecting forearm to wrist bones) ligaments. These ligaments can be involved by various pathologies, potentially leading to carpal imbalance, distortion in force transmission, and progression to permanently altered biomechanics, chondral wear, and degenerative changes. A systematic imaging analysis and structured reporting is essential for optimal diagnostic assessment of the wrist structures. This chapter discusses the imaging evaluation approach and describes how to fill in the structured checklist in Box 1. Conceptual details of related MR physics and imaging protocol are discussed in the chapter on MR protocol optimization.
 IMAGE EVALUATION
IMAGE EVALUATION
The below-outlined stepwise interpretation approach is only a practical guide, and all wrist structures should be evaluated in multiple planes for optimal assessment. This will also help the readers perceive which structures are best depicted/evaluated on which particular plane.
1. Line up the similar plane fat-saturated (fs) and non-fs images and synchronize them for tandem evaluation.
2. Start with the coronal images to check for carpal and DRUJ effusions. On proton density-weighted (PDW) images, check the scapholunate (SL) and lunotriquetral (LT) intervals, ulnar variance, Gilula’s three arcs, intercarpal spaces (for possible carpal coalition, type II lunate facet hamatolunate chondromalacia), scaphotrapeziotrapezoid (STT) joint, radiocarpal, CMC and metacarpophalangeal (MCP) joints. On fsPDW images, look for bone marrow edema and bone or soft tissue cysts and evaluate the membranous portions of the SL and LT ligaments, triangular fibrocartilage complex (TFCC), radial and ulnar collateral ligaments (UCLs) while correlating with non-fsPDW images.
3. On sagittal images, check the radiolunate and lunocapitate alignment. In case of SL ligament tear, the SL angle should be measured by superimposing sagittal images depicting the scaphoid and lunate axes since these bones are not in the same plane. This is also a good plane to evaluate the dorsal (dorsal intercarpal [DIC] ligament and radiocarpal ligament) and volar extrinsic (radioscaphocapitate, radiolunotriquetral, or long radiolunate) ligaments, the short radiolunate ligament, TFCC disc, and the ulnolunate and ulnotriquetral ligament attachments of the TFCC. It serves as the secondary plane to evaluate the extent of flexor/extensor tenosynovitis, tendon tears or retraction, and ganglion cysts.
4. The evaluation continues on axial images, where the flexor and extensor tendons should be assessed for tendinosis, tear, and tenosynovitis. The axial plane is also optimal for assessing the volar and dorsal bands of the SL and LT ligaments (findings can be secondarily correlated with coronal images), the neurovascular bundles, carpal tunnel, Guyon canal, as well as the thenar, hypothenar, and interosseous muscles. Subsequently, evaluate the pisotriquetral (PT) joint and DRUJ, the volar and dorsal radioulnar ligaments, and finally, check for mass lesions and other incidental findings, such as os styloideum, lunula, etc.
 BOX 1: The Structured Report: Wrist
BOX 1: The Structured Report: Wrist
The checklist for structured reporting of MR imaging of the wrist. For each field, Normal is considered default in the dictation whereas the rest of the elements describe various pathologies that could be encountered during imaging evaluation. See Appendices 1 and 2 at the end of the chapter for sample completed reports of normal and abnormal examination results.
Exam: MRI of Wrist
FINDINGS:
Alignment: [<Normal / Abnormal>]
Ulnar variance: [<Neutral / Negative / Positive>]
Distal radioulnar joint: [<Congruent / Subluxation>]
Scapholunate dissociation: [<Absent / Present> <DISI / VISI / Midcarpal instability>]
Fluid:
Carpus joint effusion: [<None> <Small / Moderate / Large>]
Distal radioulnar joint effusion: [<None> <Small / Moderate / Large>]
Intrinsic ligaments:
Scapholunate ligament: [<Intact> <Thickened> <Acute sprain (<Dorsal / Membranous / Volar band>)>]
Lunotriquetral ligament: [<Intact> <Thickened> <Acute sprain (<Dorsal / Membranous / Volar band>)>]
Ulnar side:
Triangular fibrocartilage: [<Intact> <Degeneration> <Acute sprain (<Central / Peripheral>)>]
Lunate facet: [<Present / Absent>]
Hamate–lunate joint: [<Normal / Chondrosis / Osteoarthritis>]
Ulnocarpal impaction: [<None / Ulnolunate / Ulnotriquetral>]
Extensor compartment:
I: [<Normal> <Tenosynovitis / Tendinosis / Tear>]
II: [<Normal> <Tenosynovitis / Tendinosis / Tear>]
III: [<Normal> <Tenosynovitis / Tendinosis / Tear>]
IV: [<Normal> <Tenosynovitis / Tendinosis / Tear>]
V: [<Normal> <Tenosynovitis / Tendinosis / Tear>]
VI: [<Normal> <Tenosynovitis / Tendinosis / Tear>]
Flexor compartment:
Flexor retinaculum: [<Normal> <Thickened / Bowed / Discontinuous>]
Flexor tendons: [<Normal / Tenosynovitis / Tendinosis / Tear>]
Carpal tunnel: [<Normal> <Effaced deep fat pad>]
Median nerve: [<Normal> <Hyperintense> <Proximal enlargement with distal flattening>]
Guyon canal: [<Normal> <Hyperintense ulnar nerve>]
Articular:
Thumb–carpometacarpal/Metacarpophalangeal joints: [<Normal> <Osteoarthritis>]
Scaphotrapeziotrapezoidal joint: [<Normal> <Osteoarthritis>]
Pisiform–triquetral joint: [<Normal> <Effusion> <Ganglion>]
Extrinsic ligaments:
Radial collateral ligament/Ulnar collateral ligament: [<Normal> <Attenuated> <Acute Sprain>]
Dorsal intercarpal ligament/Volar extrinsic ligaments: [<Normal> <Acute Sprain>]
Bones: [<Normal / Otherwise normal>]
Muscles: [<Normal>]
Vessels: [<Normal>]
Other: [<None>]
Impression:
[<In the order of importance with acute findings first>.]
 HOW TO FILL THE STRUCTURED REPORT
HOW TO FILL THE STRUCTURED REPORT
ALIGNMENT: [<Normal / Abnormal>]
Ulnar variance: [<Neutral / Negative / Positive>]
Distal radioulnar joint: [<Congruent / Subluxation>]
Scapholunate dissociation: [<Absent / Present> <DISI / VISI / Midcarpal instability>]
The wrist bones and their alignment are best evaluated on non-fs images. Normal alignment refers to articular surface congruency (convexity of an articular surface matching with the concavity of the opposite articular surface) at the DRUJ, radiocarpal, and intercarpal joints (Figs. 1–3). On the coronal images, similar to the plain radiographs, Gilula A, B, and C lines (following the proximal aspect of proximal carpal row, distal aspect of the proximal carpal row, and proximal aspect of the capitate–hamate articulations, respectively) should be smooth curves with no abrupt step-off(s); and on the axial image, the scaphoid should not protrude beyond the line connecting dorsal aspects of scaphoid and lunate (Fig. 4). Most patients with instability present with one or more symptoms, such as pain, swelling, clicking during physical examination or feeling of wrist clunk. The lesions could involve one bone in isolation, such as in pisiform subluxation or, more commonly, multiple carpal bones. The resulting dynamic instability and maltracking of bones can be detected earlier and more confidently with kinematic evaluation under fluoroscopy, kinematic MRI or 4D CT, whereas conventional MRI depicts anatomic abnormalities in more advanced cases with static carpal malalignments.
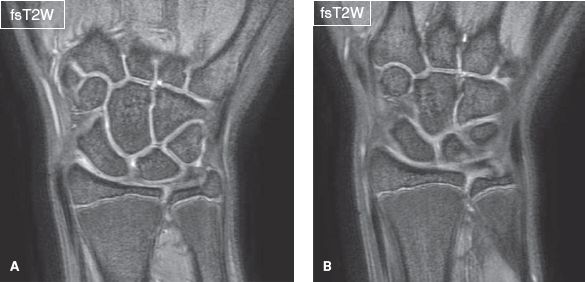
Fig. 1: Normal wrist anatomy. Sequential coronal gradient-echo images (A, B) show articular surface congruency at the distal radioulnar, radiocarpal, and intercarpal joints.
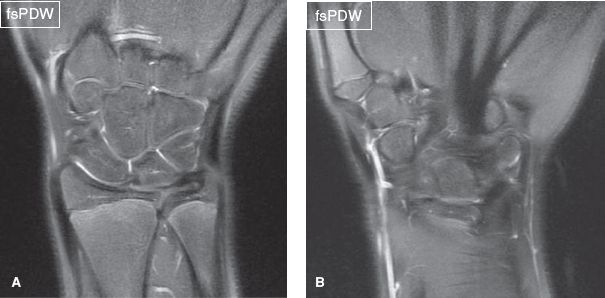
Fig. 2: Normal wrist anatomy. Sequential coronal spin-echo images (A, B) show articular surface congruency at the distal radioulnar, radiocarpal, and intercarpal joints.

Fig. 3: Normal carpal alignment. A: Sagittal image in neutral position shows the concavity of the lunate matches with the convexity of the capitate (green and purple lines, respectively). B: Notice similar congruity in the extended position.
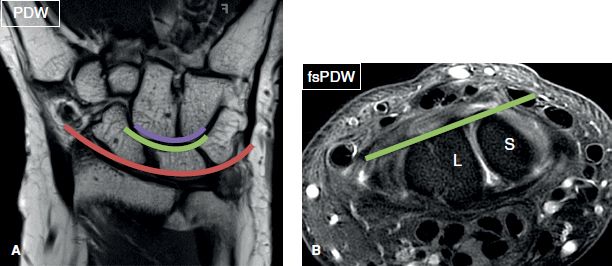
Fig. 4: Gilula lines. A: Coronal image shows the three parallel Gilula lines (A is red, B is green, C is purple). B: Axial image shows articular surface congruency at the scapholunate (SL) space with no dorsal protrusion of the scaphoid (S).
Ulnar variance refers to the relative lengths of the distal articular surfaces of the radius and ulna. It is defined as neutral, positive, or negative based on whether the distal articular surface of the ulna is aligned with the distal articular surface of the radius, or lies >2 mm distal, or >2 mm proximal to the latter, respectively (Figs. 5, 6). Negative ulnar variance is believed to be associated with osteonecrosis of the lunate (Kienböck’s disease), and positive ulnar variance with ulnocarpal abutment and TFCC tears. However, one should note that ulnocarpal abutment can also be seen in the setting of neutral or negative ulnar variance. Of the several measurement methods available to evaluate the congruity of the DRUJ, the easiest and reproducible are (1) the congruency method, which looks for simple congruency between the arc of the sigmoid notch and the convexity of dome of ulnar head, and (2) Mino’s method, in which two lines are drawn through the dorsal and volar aspects of the distal radius at the level of sigmoid notch, excluding the Lister tubercle. The distal ulna should normally be located between these lines or within 10% to 20% of these confines, otherwise dorsal or volar subluxation exists (Fig. 7). Detection of chronic insufficiency or acute tears of volar and distal radioulnar ligaments can assist in the clinical diagnosis of dorsal and volar DRUJ instability, respectively. If available, comparison with the contralateral wrist is also useful. At the level of the DRUJ, the location of the ulnar styloid process in the axial plane reveals the position of the wrist: The styloid process is located volarly, dorsally, and medially when the wrist is in pronation, supination, and in neutral position, respectively. Other etiologies that may be implicated in DRUJ instability include sigmoid rim fracture, sigmoid notch hypoplasia, complex radial fractures, ulnar styloid fracture (especially involving its base), and ulnar head abnormality from prior injury or partial resection. On the coronal images, other imaging findings that may indicate DRUJ subluxation, include radial shortening, widening of DRUJ space, and negative ulnar variance of greater than 5 mm.
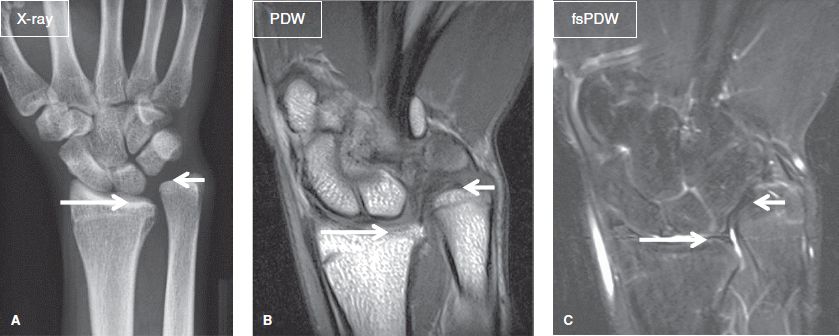
Fig. 5: Positive ulnar variance. On anteroposterior radiograph (A) and respective coronal MR images (B, C), the distal articular surface of the ulna (short arrows) lies more than 2 mm distal to the distal articular surface of the radius (long arrows).
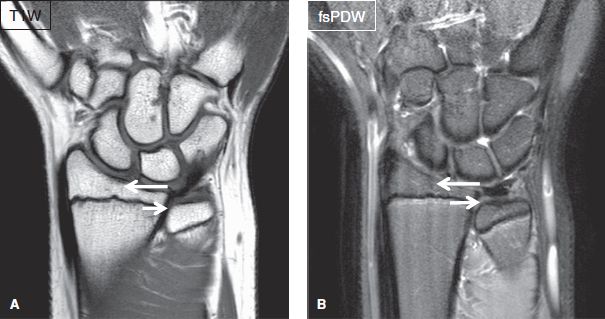
Fig. 6: Negative ulnar variance. On coronal MR images (A, B), the distal articular surface of the ulna (short arrows) lies more than 2 mm distal to the distal articular surface of the radius (long arrows).
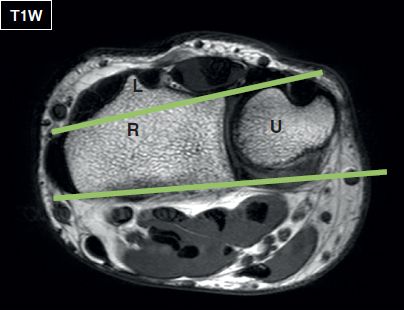
Fig. 7: Normal DRUJ alignment. Two lines are drawn through the dorsal and volar aspects of the distal radius (R) at the level of sigmoid notch, excluding the Lister tubercle (L). The distal ulna (U) should normally be located between these lines or within 10% to 20% of these confines, otherwise dorsal or volar subluxation exists.
The bones of the proximal carpal row (scaphoid, lunate, triquetrum) move as an intercalated segment, which is stabilized by multiple ligaments. The segment has no muscular attachments, and its motion follows the movements of the distal carpal row and forearm bones. Therefore, intercalated instability refers to incongruent movement between the proximal and distal carpal rows. Instability can also be defined as dissociative, nondissociative, or adaptive. Dissociate instability refers to instability related to incongruent carpal bones in the same row (implying intrinsic ligament injury) whereas nondissociate instability indicates instability involving incongruent intercalated segments (implying extrinsic ligament injury). Adaptive instability is related to prior trauma, such as radius fracture.
The integrity of the intercalated segment may be disrupted in cases of SL or LT dissociation. On coronal images, the SL interval is normally less than 3 mm and on sagittal images, the SL angle ranges between 30 and 60 degrees, with values between 60 and 80 degrees considered borderline normal. In SL dissociation, there is diastasis (≥3 mm) of the SL space (Fig. 8), the scaphoid undergoes volarflexion (rotatory subluxation) and dorsal displacement with narrowing of the radioscaphoid space whereas the triquetrum pulls the lunate into dorsiflexion. The resulting deformity is termed as dorsal intercalated segmental instability (DISI) and is characterized by increased (>80 degrees) SL angle, increased (>30 degrees) lunocapitate angle, increased radiolunate (>15–20 degrees) angle, and radiodorsal shift of the lunate with loss of lunocapitate interspace congruency. Clinically, Watson test is performed to evaluate SL instability. The examiner places a thumb over the patient’s scaphoid tubercle, applying dorsal pressure. The wrist is then moved from ulnar to radial deviation. A painful “clunk” reflects positive test for SL instability. If radiographs are available, comparison to the other side is quiet useful. Secondary radiographic findings include, lunate overlap on capitate on the PA view and more vertical position of the scaphoid. DISI usually involves SL ligament tear with injury to the extrinsic ligaments (commonly radioscaphocapitate ligament). The entity may also develop in cases of unstable scaphoid waist fractures, which allow the distal scaphoid pole to translate proximal and volar while the proximal pole remains attached and tilts dorsally with the lunate. Other radiographic signs include, foreshortening of the scaphoid (ring sign) and a triangular-shaped lunate (due to rotation). In advanced stages of SL instability, the capitate migrates proximally between the scaphoid and lunate, forcing the two bones further apart, in a configuration known as SL advanced collapse (SLAC) (Fig. 8). The condition is most commonly caused by trauma (associated with other imaging evidence of trauma findings) or calcium pyrophosphate arthropathy (associated with chondrocalcinosis and cystic degenerative changes of carpus). Another related entity is scaphoid nonunion advanced collapse (SNAC), which also shows proximal capitate migration similar to SLAC, however, it occurs in the setting of nonunited scaphoid fracture.
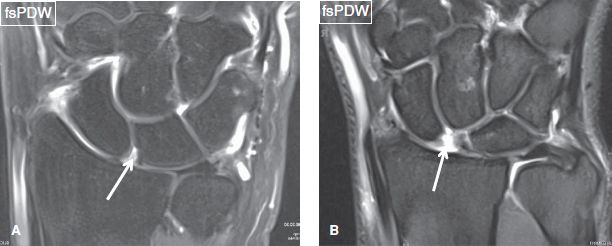
Fig. 8: Scapholunate dissociation and SLAC. Coronal images from different patients demonstrate complete tears (arrows) of the scapholunate ligament. In (A), there is widening of the scapholunate space in keeping with SL dissociation while in (B) there is proximal capitate migration in keeping with a SLAC wrist.
In LT dissociation, the lunate and scaphoid tilt volarly and the capitate dorsally, in a deformity known as volar intercalated segmental instability (VISI), which is depicted as decreased (<30 degrees) SL angle and increased (>30 degrees) lunocapitate angle (Fig. 9). VISI involves disruption of the LT & volar radiolunotriquetral ligaments, as well as attenuation or rupture of the dorsal radiotriquetral (DIC ligament) attachments. The entity may result from trauma, and has been associated with rheumatoid arthritis and Kienböck’s disease (Fig. 10). Lunottriquetral instability is evaluated clinically using Ballottement test or compression test. The Ballottement test is performed by securing the pisotriquetral unit with the thumb and index finger of one hand and the lunate with the other hand. Volar and dorsal stresses are placed on the LT joint. The criteria for a positive test are increased excursion of the triquetrum and accompanying painful crepitus. The compression test involves painful displacement of the triquetrum ulnarly during radioulnar deviation. In VISI lesions, one should check for DRUJ or TFCC injury, since the latter associations are common. Bilateral VISI deformity should raise the suspicion of Marfan syndrome.
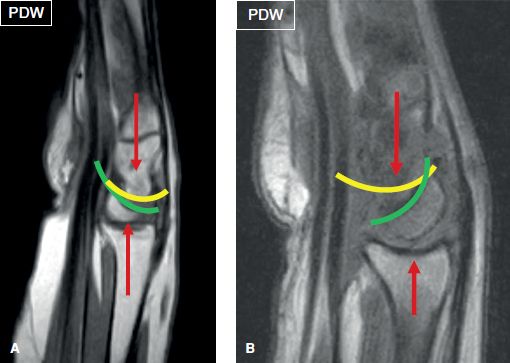
Fig. 9: DISI vs VISI. A: Dorsal intercalated segmental instability. Sagittal image shows loss of colinearity between the lunate and capitate (yellow and green lines) with normal alignment of radius and capitate (red arrows). The lunocapitate angle is increased and scapholunate angle measured 88 degrees. B: Volar intercalated segmental instability complicating a case of rheumatoid arthritis. Sagittal image shows loss of colinearity between the capitate and lunate (yellow and green lines) with volar tilt of lunate. Note maintained colinearity between radius and capitate (red arrows). The scapholunate and lunocapitate angles were measured 10 degrees and 50 degrees, respectively.
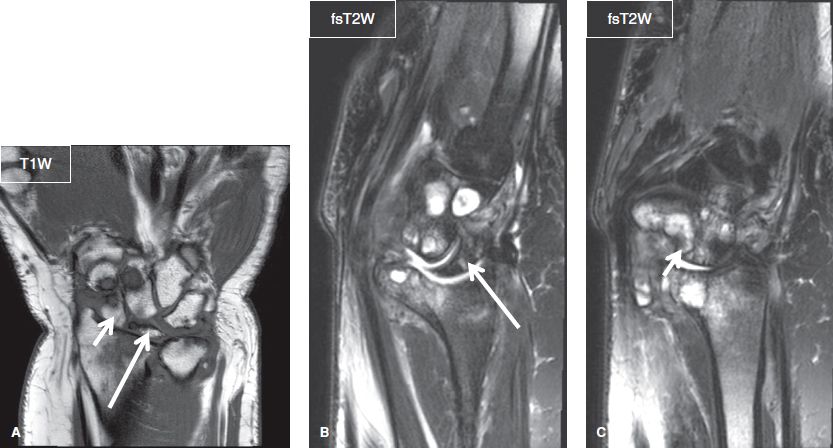
Fig. 10: Volar intercalated segmental instability complicating a case of rheumatoid arthritis. Coronal (A) and sagittal (B, C) images show scattered cystic–erosive changes of the wrist bones. Notice SLAC wrist (A), volar tilt of the scaphoid (short arrows), and lunate (long arrows) (B, C). The scapholunate and lunocapitate angles were measured 9 degrees and 76 degrees, respectively.
Instability may propagate around the lunate with maintenance of colinearity between radius and lunate. This perilunate instability progresses from the SL and capitolunate joints to the LT joint. About 25% of perilunate instabilities are missed at initial presentation and can present as carpal tunnel syndrome. Based on severity, it can be classified as follows.
 Stage I—is characterized by SL and volar radioscaphocapitate ligament injury, along with scaphoid instability
Stage I—is characterized by SL and volar radioscaphocapitate ligament injury, along with scaphoid instability
 Stage II—in which there is dorsal subluxation of the capitate relative to the lunate along with opening of the space of Poirier (V-shaped area of weakness in the palmar wrist formed by the volar carpal ligaments)
Stage II—in which there is dorsal subluxation of the capitate relative to the lunate along with opening of the space of Poirier (V-shaped area of weakness in the palmar wrist formed by the volar carpal ligaments)
 Stage III—established with radiotriquetral (long and short radiolunate) ligament failure and triquetral dislocation
Stage III—established with radiotriquetral (long and short radiolunate) ligament failure and triquetral dislocation
 Stage IV—in which the lunate dislocates from the radiolunate fossa following failure of the radiocarpal (radiocapitate, radiotriquetral), and DIC ligaments.
Stage IV—in which the lunate dislocates from the radiolunate fossa following failure of the radiocarpal (radiocapitate, radiotriquetral), and DIC ligaments.
Midcarpal instability refers to incongruity at the midcarpal spaces and abrupt step-offs in Gilula B and C lines. The entity may manifest as excessive dorsal tilt of the lunate and dorsal subluxation of the capitate at the lunocapitate joint, due to insufficiency of the deltoid (arcuate or midcarpal) ligament and occasionally of the volar extrinsic radioscaphocapitate ligament. Therefore, there is loss of radiocapitate alignment. Another variant is triquetrohamate incongruency, due to insufficiency of the deltoid ligament and occasionally of the long radiolunate ligament. In general, SL instability is more common than midcarpal instability, which is also more common than LT instability.
Carpal translocation can occur in any direction but is more common in the ulnar direction. In the latter case, the lunate shifts out toward the ulnar aspect of the radiocarpal joint, and exhibits greater than 50% subluxation from the lunate fossa of the radius. The condition is most commonly seen with rheumatoid arthritis (entire carpus may translocate) and trauma (scaphoid may remain in place or entire carpus may translocate), but authors have also seen it occurring in an idiopathic fashion and involving both wrists simultaneously.
FLUID:
Carpus joint effusion: [<None> <Small / Moderate / Large>]
Distal radioulnar joint effusion: [<None> <Small / Moderate / Large>]
Coronal images are most useful to assess for radiocarpal joint and DRUJ effusions, and axial images for PT joint effusion. These joints have thin synovial linings and normally contain a small amount of fluid for nutrition and lubrication. Joint effusion is noted when excessive fluid causes distention of the joint capsule (Fig. 11). Findings such as synovial thickening, intra-articular debris, loose bodies, synovial diverticula(e), and ganglion cysts should also be reported, as they may be associated with underlying internal derangement and/or injury (Figs. 12, 13). Capsular injuries may occur from recent or prior trauma and manifest as irregularity, attenuation, and/or thickening of the joint capsule. Synovial diverticulae (unilocular with wide communication with the joint space) commonly arise from the PT recess of the joint and the volar aspect of the radioscaphoid joint. Ganglion cysts (uni- or multilocular cysts with narrow or obliterated neck) reflect chronic processes and these lesions can be painful, even if they are small. The neck of the ganglion should be identified as it can lead the reader to the site of its origin and help identify underlying synovial or ligament injury (Fig. 14). Common locations and associated injuries include DIC ligament, volar band SL, and peripheral TFCC tears.
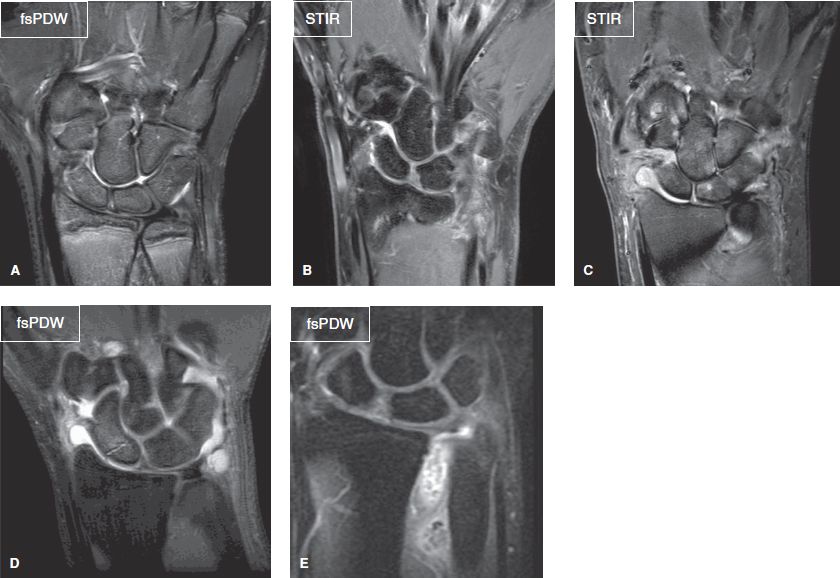
Fig. 11: Normal and abnormal joint fluid. Coronal images from different cases demonstrate normal joint fluid (A), small (B), moderate (C), and large (D) effusions in the wrist joints. In (E), there is large effusion isolated to the distal radioulnar joint with synovial chondromatosis.
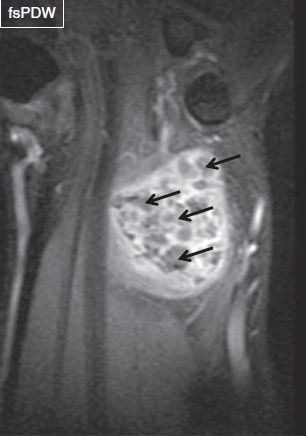
Fig. 12: Primary osteochondromatosis. Coronal image shows large effusion in the distal radioulnar joint containing numerous nodular lesions (arrows) of intermediate signal.
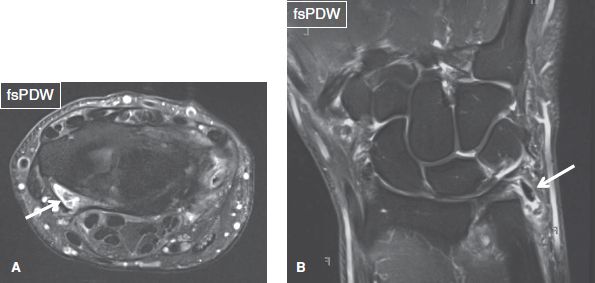
Fig. 13: Intra-articular loose bodies. Axial (A) and coronal (B) images from different patients exhibit loose bodies (arrows) within the radiocarpal and ulnocarpal joints, respectively.
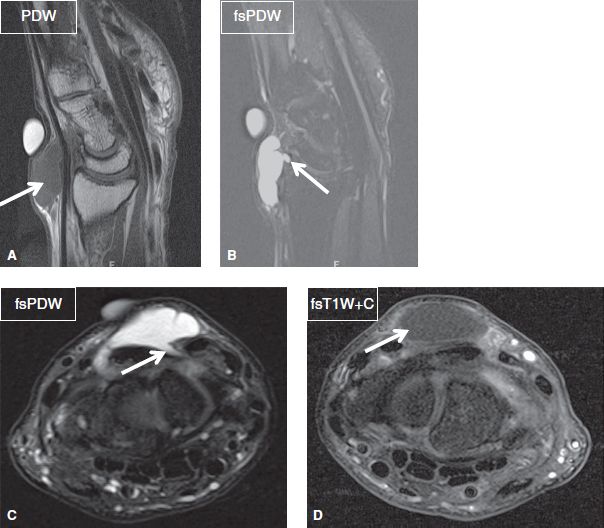
Fig. 14: Ganglion cyst. Sagittal (A, B) and axial (C, D) images show a ganglion cyst (arrow in A) with the neck extending beneath the dorsal intercarpal ligament (arrows in B, C). Notice minimal peripheral enhancement (arrow in D), confirming the cystic nature of the mass lesion.
INTRINSIC LIGAMENTS:
Scapholunate ligament: [<Intact> <Thickened> <Acute sprain (<Dorsal / Membranous / Volar band>)>]
Lunotriquetral ligament: [<Intact> <Thickened> <Acute sprain (<Dorsal / Membranous / Volar band>)>]
The SL and LT ligaments are clinically and biomechanically important wrist stabilizers, which link the bones of the proximal carpal row. They both feature dorsal band, volar band, and a thin central membranous (proximal) portion, which in combination create a water-tight seal between the radiocarpal and midcarpal spaces.
The SL ligament stabilizes the palmar rotation force of the scaphoid against the dorsal rotation force of the lunate. It is approximately 18 mm long and 2–3 mm thick. The volar band is composed of thin oblique fibers and is the weakest and most vulnerable to tear, particularly at its scaphoid attachment. The dorsal band is the thickest, strongest, and functionally the most important part of the ligament. The volar and dorsal bands are best evaluated on axial images, where they appear as band-like structures, with the former featuring homogeneous signal intensity and the latter showing minimally heterogeneous striate morphology. The membranous portion is best depicted on coronal image, where it features heterogeneous signal and appears band-like at its dorsal aspect, triangular at its central aspect, and trapezoidal at its volar aspect (Figs. 15, 16).
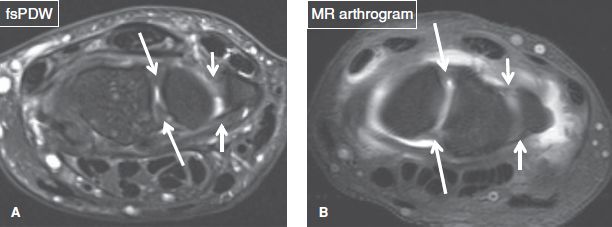
Fig. 15: Normal intrinsic ligaments. Axial conventional (A) and arthrography (B) images demonstrate the normal dorsal and volar bands of the scapholunate (long arrows) and lunotriquetral (short arrows) ligaments.
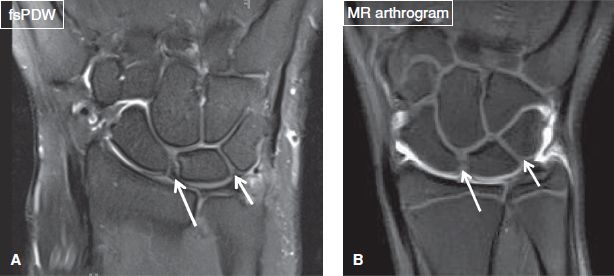
Fig. 16: Normal intrinsic ligaments. Coronal conventional (A) and arthrography (B) images demonstrate the normal membranous bands of the scapholunate (long arrows) and lunotriquetral (short arrows) ligaments.
The LT ligament preserves the relationship of the lunate to the triquetrum, allowing the latter to move from a proximal to a distal position during ulnar deviation. In contrast to the SL ligament, the dorsal band of the LT ligament is relatively thinner whereas the volar component is thicker, stronger, functionally more important and interdigitates with longitudinally oriented fibers of the lunocapitate ligament. Similar to the SL ligament, the dorsal and volar bands of the LT ligament are best seen on axial images and the membranous portion is well seen on coronal images. The ligament appears triangular or, less commonly, linear or bar-like in shape and normally demonstrates uniform low signal intensity. Normal variant includes a thin line of increased signal intensity inside the body of the ligament but not completely traversing through its entire thickness.
SL and LT ligament tears may be categorized as complete or incomplete, on the basis of whether there is involvement of all or only some components of the ligament, and as full-thickness or partial-thickness, based on whether they extend through the entire thickness of the ligament band or leave a portion intact. Acuity of tear is suggested by adjacent fascial edema, fluid, or signs of recent trauma. Primary signs of SL ligament injury (sprain) include fluid-like signal or discontinuity of the ligament on fsPDW or fs T2-weighted (T2W) images, distorted morphology with fraying, irregularity, thickening, and/or thinning and complete absence of the ligament (Figs. 8, 17–20). Secondary signs, which may help in identifying the ligament injury include traction-related avulsive cystic/enthesopathy changes at the osseous attachment, SL dissociation (SL interval >3 mm), soft tissue ganglia from associated capsular injuries or ligament degeneration, and carpal arch (Gilula arc) disruption. Differentiation between types of tears is clinically important because partial-thickness tears may self-resolve without ever causing carpal instability whereas full-thickness tears and complete ligament disruptions often lead to carpal instability. Complete disruption of the dorsal or volar bands is suggestive of trauma or may be associated with rheumatoid arthritis whereas isolated perforations of the membranous portion are commonly degenerative in nature and asymptomatic. Concomitant injury to adjacent volar extrinsic (radioscaphocapitate) ligament results in static instability (rotary subluxation or DISI).
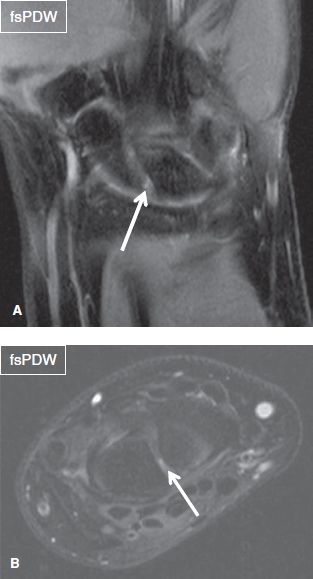
Fig. 17: Scapholunate ligament incomplete injury. Coronal (A) and axial (B) images show full-thickness tear (arrows) of the volar band of the scapholunate ligament.

Fig. 18: Complete scapholunate ligament injury. Coronal image exhibits complete tear (long arrow) of the scapholunate ligament with scapholunate dissociation. Also note tears of the styloid (arrowhead) and foveal (short arrow) attachments of the triangular fibrocartilage.
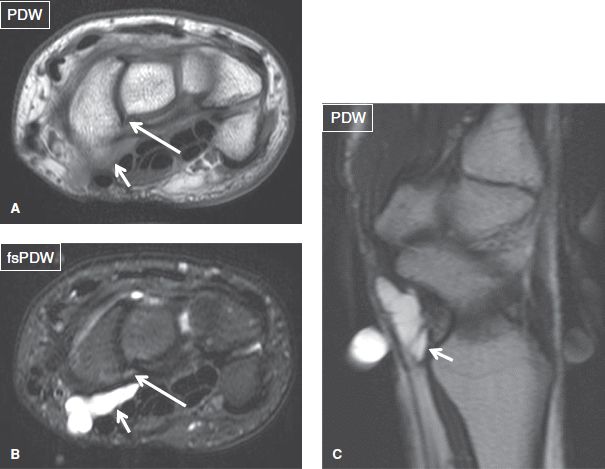
Fig. 19: Scapholunate ligament injury with ganglion formation. Axial (A, B) and sagittal (C) images show partial tear of the volar band of the scapholunate ligament (long arrows) with an associated ganglion (short arrows).
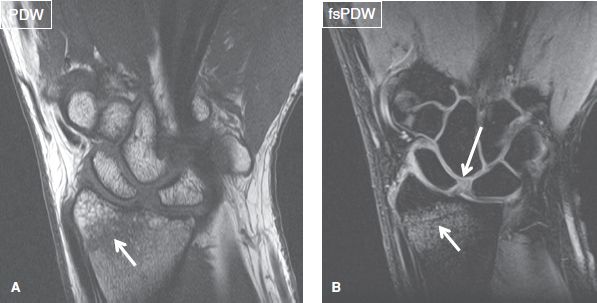
Fig. 20: Acute complete scapholunate ligament injury. Coronal images (A, B) exhibit widening of the scapholunate space due to complete tear (long arrow) of the scapholunate ligament. Also note an acute fracture of the distal radial epiphysis (short arrows).
Tears of the LT ligament are much less common than SL ligament tears, occurring only about one-sixth as often. Degenerative perforations are usually asymptomatic and often associated with ulnocarpal abutment (see below). They typically involve the membranous portion of the ligament, leaving the volar and dorsal portions intact. Again, one should search for secondary signs, such as traction-related avulsive cystic changes or enthesopathy at the osseous attachments, LT curve step-off, and soft tissue ganglion from associated capsular injury or ligament degeneration (Figs. 21, 22). Associated widening of the LT interval is usually evident. A complete LT ligament tear is usually not sufficient for development of static carpal collapse or VISI. There is often associated capsular and extrinsic ligament damage (DIC ligament). Based on severity, ulnar-sided perilunate instability can be classified as follows.
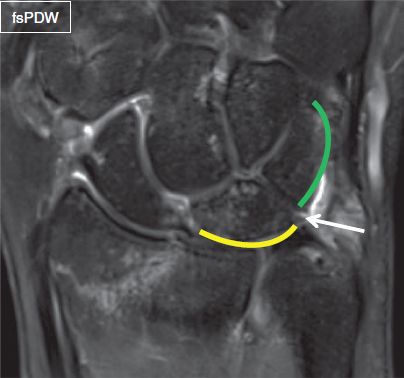
Fig. 21: Lunotriquetral ligament injury. Coronal image exhibits perforation of the membranous portion (arrow) of the lunotriquetral ligament. There is step-off at the Gilula A line (yellow and green lines). Also note nondisplaced fracture of the distal radius.

Fig. 22: Lunotriquetral ligament injury. Coronal image exhibits perforation of the membranous portion (arrow) of the lunotriquetral ligament with contrast extension from radiocarpal joint into the midcarpal space. Notice step-off at the Gilula A line on this arthrography image.
 Stage I—characterized by partial or complete tear of LT ligament (no VISI)
Stage I—characterized by partial or complete tear of LT ligament (no VISI)
 Stage II—defined as complete LT ligament tear along with disruption of the palmar LT ligaments (dynamic VISI)
Stage II—defined as complete LT ligament tear along with disruption of the palmar LT ligaments (dynamic VISI)
 Stage III—characterized by complete LT ligament tear, disruption of the palmar LT, and dorsal radiocarpal ligaments (static VISI)
Stage III—characterized by complete LT ligament tear, disruption of the palmar LT, and dorsal radiocarpal ligaments (static VISI)
Finally, multi-ligament degeneration or tears are not uncommon in the setting of advanced inflammatory arthropathy, such as rheumatoid arthritis (Fig. 23).

Fig. 23: Scapholunate and lunotriquetral ligament injury. Coronal image exhibits complete tear of the scapholunate ligament (short arrow) and perforation of the membranous portion of the lunotriquetral ligament (long arrow). Notice step-off at the Gilula A line on this arthrography image in a patient with rheumatoid arthritis.
ULNAR SIDE:
Triangular fibrocartilage ligament: [<Intact> <Degeneration> <Acute sprain (<Central / Peripheral>)>]
Lunate facet: [<Present / Absent>]
Hamate–lunate joint: [<Normal / Chondrosis / Osteoarthritis>]
Ulnocarpal impaction: [<None / Ulnolunate / Ulnotriquetral>]
The TFCC is composed of fibrocartilaginous and ligamentous structures situated in the ulnocarpal space. It allows force transmission from the carpus to the ulna, cushions the ulnar fovea and lunate during ulnar deviation of the wrist, and provides DRUJ and ulnocarpal stability. It consists of various components, including the triangular fibrocartilage disc, UCL, meniscus homolog, ulnocarpal (ulnolunate and ulnotriquetral) ligaments, extensor carpi ulnaris (ECU) tendon sheath, volar and dorsal radioulnar ligaments, and DRUJ capsule (Fig. 24).
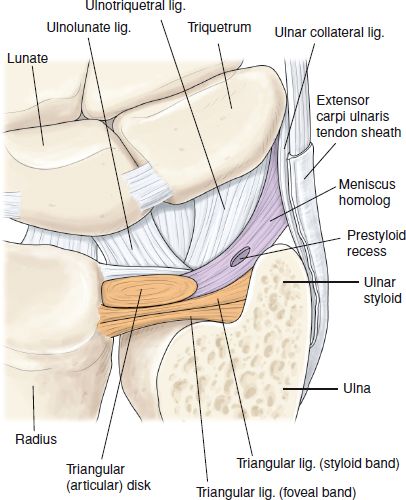
Fig. 24: TFCC complex showing various components of the complex.
The bowtie-shaped articular disc is anchored to the ulnar side of the distal radius and attaches as two distinct bands onto the ulnar styloid process and ulnar fovea, and more distally onto the hamate, triquetrum, and base of the fifth metacarpal bone. The disc is best depicted on coronal images and normally features homogeneous low signal intensity on all pulse sequences but occasionally appears slightly brighter on the gradient-echo images (Fig. 25). The two ulnar insertions are composed of fibrofatty and vascularized connective tissue, and, thus, normally feature a striated configuration, which is particularly evident on 1.5T and 3T MR images. The space between the two insertions is filled by vascularized connective tissue, which is known as the ligamentum subcruentum. The latter normally features intermediate signal intensity, which should not be misinterpreted as a tear. The hyaline cartilage, which is located underneath the lateral portion of the TFCC attachment to the radius, normally exhibits intermediate signal intensity and should not be misinterpreted for radial-sided tear (Fig. 26). The thickness of the disc is inversely proportional to the degree of ulnar variance. In case of a neutral variant, it is approximately 5 mm thick at the ulnar side and 2 mm at the radial side but becomes thicker in subjects with negative ulnar variance and thinner (and thus weaker) in individuals with positive ulnar variance, possibly explaining the increased vulnerability of the latter population to TFCC degenerative tears and maceration. The ulnolunate and ulnotriquetral ligaments are evaluated on coronal and sagittal images (Fig. 27). The dorsal and volar radioulnar ligaments attach bone to bone versus TFCC connects ulna to the radial cartilage. These ligaments are best seen on axial and coronal images.
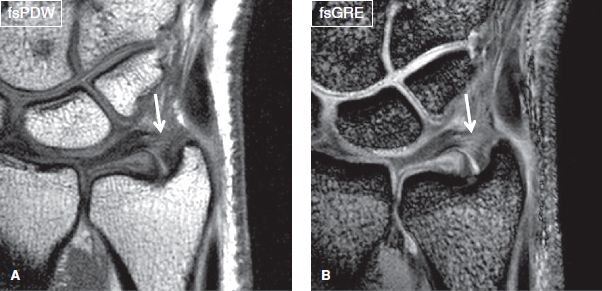
Fig. 25: TFCC appearance on different coronal (A, B) sequences. Notice mild brightness on GRE sequence (arrows) as compared to the conventional spin-echo sequence, a normal variant.
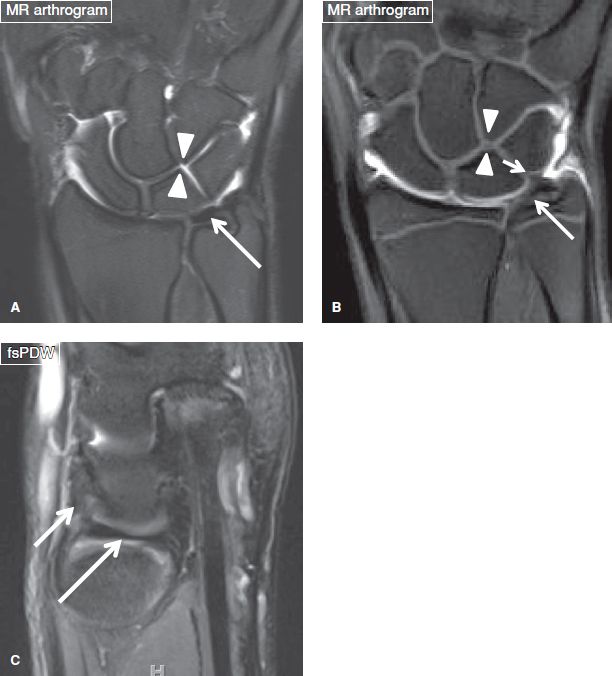
Fig. 26: Normal TFCC. A, B: Coronal arthrography images exhibit normal triangular fibrocartilage disc (long arrows) and ulnolunate ligament (short arrow). Also note type I (arrowheads in A) and type II (arrowheads in B) lunate facets. Notice normal cartilage undercutting the lateral TFCC attachment to the radius. C: Sagittal image shows normal ulnolunate ligament (short arrow) attaching the disc to the lunate dorsal surface.
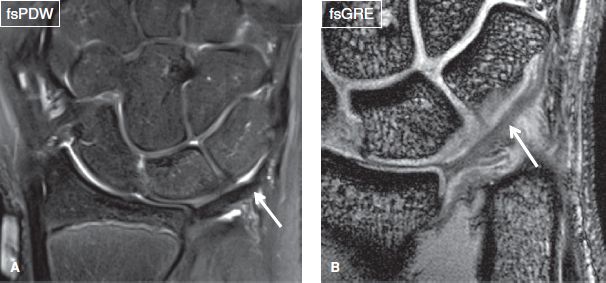
Fig. 27: TFCC complex. Coronal images (A, B) show the ulnotriquetral ligament (arrows).
Degeneration of the TFCC disc is commonly seen as asymptomatic finding that appears as intrasubstance intermediate signal on T1-weighted (T1W) and PDW images, which does not increase to fluid-like signal on fsPDW/fsT2W images. The signal alteration may be associated with disc thickening, thinning, or fraying of the edges. The signal may be more pronounced in patients with positive ulnar variance and could reflect ulnocarpal abutment-related derangement.
TFCC disc tears can be asymptomatic or symptomatic and these lesions appear either as detachment of the radial or ulnar disc attachments, or as fluid-like signal/gaps in the disc margins, which disrupt one or both articular surfaces (surface tears) (Figs. 28–36). TFCC tears can occur toward the foveal aspect or toward the carpus, and depending on the location of the lesion, the surgical approach may vary from arthroscopy to open approach. Tears are traditionally classified as peripheral (when located at the foveal or styloid attachments), central (when located in the middle of the disc, usually encountered more toward the radial side), or radial-sided (when the radial attachment of the disc is avulsed). Associated findings of TFCC tear include abnormal morphology, attenuation and/or discontinuity of the disc, avulsive bone marrow cystic changes and edema at the ulnar styloid or foveal attachments, and extension of fluid and/or edema along the medial aspect of the distal ulna, proximal to the base of the styloid process. TFCC disc tears may also be associated with stripping of the UCL from the ulna, abnormal morphology of the normally triangular-shaped meniscus homolog, sprains of the ulnocarpal (ulnolunate and ulnotriquetral) ligaments, avulsion of the tip or base of the styloid process (best seen on PDW images), tendinosis, tear, tenosynovitis, or subluxation of the ECU tendon (with extensor retinaculum or subsheath injury, best seen on axial images), and soft tissue or intraosseous ganglion formation. TFCC disc perforations are identified based on a common finding of fluid distention of the DRUJ, but this latter finding is nonspecific, as it can also be present in isolated arthritis or inflammation of the joint. Reporting the transverse location of TFCC tears is important for patient management. The TFCC has good vascularity toward its ulnar side; therefore, peripheral tears are expected to heal if the torn edges are held in close contact, or are surgically repaired. The indications for repair include, large tears, unstable tears, or symptomatic tears. If symptomatic, central perforations are treated with débridement. Treatment of radial-sided tears depends upon the coexistence of DRUJ ligament tears or instability. Traumatic and degenerative tears of the TFCC are graded according to the Palmer classification (Table 1), in which simultaneous pathology of the LT ligament upgrades the stage of the TFCC injury and alters the treatment options.
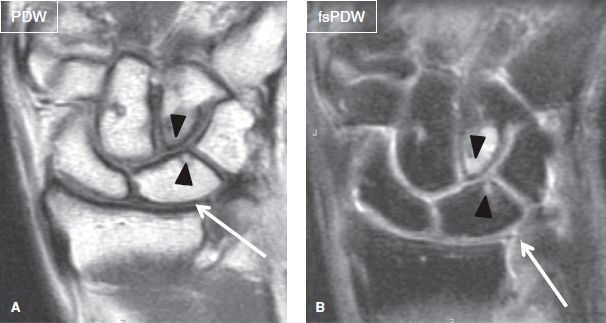
Fig. 28: Triangular fibrocartilage disc perforation. Coronal images (A, B) show central perforation (arrows) of the triangular fibrocartilage disc. Also note type II lunate with associated hamatolunate osteoarthrosis (arrowheads).
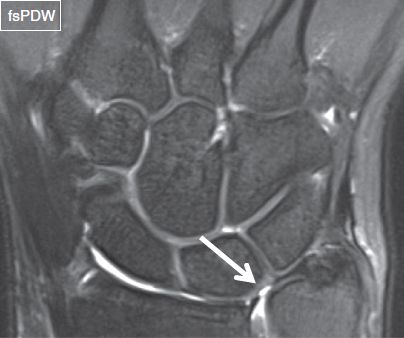
Fig. 29: Triangular fibrocartilage disc injury. Coronal image shows central perforation (arrow) of the triangular fibrocartilage disc. Notice type II lunate facet with hamatolunate chondrosis.
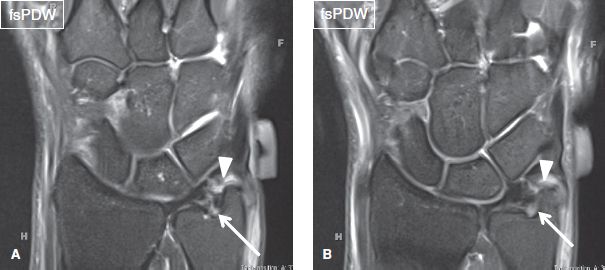
Fig. 30: Grade II sprain of the triangular fibrocartilage disc. Sequential coronal images (A, B) show partial tear of the foveal (arrows) and styloid (arrowheads) attachments of the triangular fibrocartilage disc. Notice subcortical cyst at the foveal attachment of the disc.
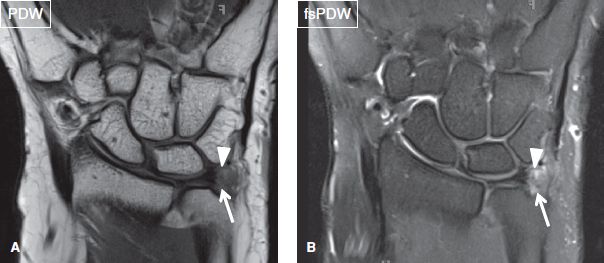
Fig. 31: Triangular fibrocartilage disc injury. Coronal images (A, B) exhibit near-complete tears of the foveal (arrows) and styloid (arrowheads) attachments of the triangular fibrocartilage disc.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







