Chapter 9 The Vertebral Subluxation Complex
After reading this chapter you should be able to answer the following questions:
| Question 1 | How are homeostatic neural mechanisms altered by the subluxation complex? |
| Question 2 | What methods do chiropractors use to assess the subluxation complex? |
| Question 3 | How do chiropractors reduce the effects of subluxation complex? |
Many chiropractors maintain clinical practices for 40 or 50 years, and they do so because of the profound effects they have witnessed after patients receive a chiropractic adjustment. Patients return again and again because they feel the chiropractor offers something special, something different from the classic medical encounter. In this regard, we believe that there are vitalistic, psycho-spiritual aspects of patient care that occur during the hands-on chiropractic encounter. While science cannot describe this immaterial aspect of chiropractic care, much data now exist regarding spinal dysfunction that can help to describe the positive physiological outcomes related to pain relief, reduction of visceral symptoms, and feelings of wellness.1,2 Readers should be aware that such research does not validate the existence of subluxation or that subluxations are corrected by the adjustment. We can only say with certainty that the chiropractic clinical encounter offers positive outcomes, which is the likely reason why chiropractic has lived on despite attempts to sanction and eliminate the profession.
Subluxation Complex History and Development
It was believed that, due to birth trauma and normal childhood injuries, most people had atlas subluxations. Clearly, this theory places spinal subluxation as the cause of most diseases. To date, this theory has yet to be supported by objective evidence and essentially creates an incongruent educational scenario for chiropractic students. The result is that they learn about chiropractic technique and theory in one classroom and then learn about basic sciences in another classroom without any perceivable connection between the two. In essence, chiropractic students would begin college and enter two different educational tracks, the subluxation and adjusting track that trains one to be a chiropractor who adjusts the spine, and the separate and distinct basic science track that allows one to pass boards and obtain a chiropractic license.
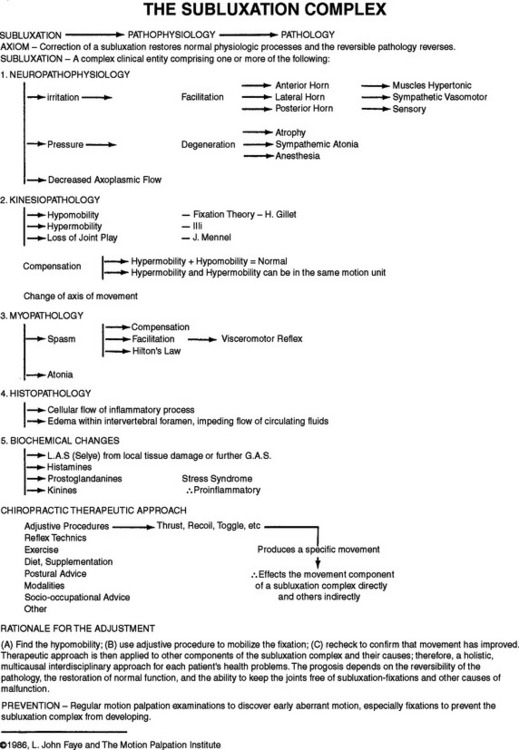
This educational disconnect was obvious to Faye while he was teaching at Anglo-European College during the 1960s. He also realized that chiropractors were essentially left with no conceptual model of subluxation to utilize in clinical practice, save for the bone-out-of-place theory. After much thought and study, in 1967 Faye presented his students with the term subluxation complex and the associated heuristic model that was eventually popularized in the late 1970s and early 1980s in the United States by the Motion Palpation Institute (Figure 9-1).
Faye’s original intent was to create a heuristic model of subluxation, that is, a speculative formulation to serve as a guide for the investigation of the subluxation. The original subluxation complex was to serve three main purposes: (1) that chiropractors would be able to relate subluxation to the world in kinesiologic, physiologic, and pathophysiologic terms that are already accepted, (2) that chiropractic would have a dynamic and scientific model of subluxation that could be appropriately researched, and (3) that chiropractors could properly function as holistic, vitalistic doctors with a strong scientific foundation. To date, none of these original intents have been widely understood or practically realized. In fact, the original dynamic subluxation complex has been converted by some into a static so-called component model3–5 that has been utilized for describing a condition that can only be affected by an adjustment.
Readers should be aware that Figure 9-1 was utilized throughout the 1970s and 1980s prior to publication in Schafer and Faye’s 1989 text.6 Notice the components of the chiropractic therapeutic approach for subluxation reduction include the following:
8. Other (open-ended to include for new techniques in patient care that fall within the scope of chiropractic care)
This armamentarium of treatments was recommended because the adjustment cannot magically resolve all the components of the subluxation complex, such as inflammation, the stress reaction, or atrophic muscles. In fact, it is entirely possible that the profound analgesic effect of the adjustment can mask the presence of underlying pathologies.7 This is certainly inconsistent with the goals of a holistic, vitalistic doctor of the type that Faye envisioned chiropractors to be. Seaman8 considered this problem and also thought the terms subluxation and subluxation complex might be too strongly associated in the minds of chiropractors with an “adjustment only” treatment approach. He proposed the term joint complex dysfunction and also listed causes and treatments that turned out to be consistent with Faye’s original model. Thereafter, Seaman emphasized getting at the biochemical causes,9,10 while others, including DeFranca,11 Liebenson,12 Murphy,13 Stude,14 and Troyanovich,15 focused on addressing the deconditioned myopathological spine with exercise. Each of the authors subsequent to Faye also understood that the subluxation complex, or spinal dysfunction, could not be effectively addressed with the adjustment alone.
As outlined in Figure 9-1, the adjustment is thought to affect the movement component directly and may have an indirect effect on the other components. Thorough resolution of the subluxation complex depends on maintaining joint motion with adjustment and other passive forms of therapy, such as myofascial care and various electrical modalities, and on removing the other causes of disease, such as poor nutrition, sedentary lifestyle, smoking, and other unhealthy factors. Without utilizing this holistic, vitalistic approach, the chiropractor functions exactly like the medical doctors we criticize for not getting at the cause of the patient’s problem. These may be hard words to swallow for some, but the assessment is nonetheless accurate.
Consider a patient who develops the subluxation complex and back pain (a symptom of some of the subluxation syndromes) due to bad posture, a lack of exercise, and a proinflammatory diet. Medical doctors will medicate or perform surgery on dysfunctional joints, while chiropractors adjust them. If neither addresses the causes, then there is no philosophical difference between medical and chiropractic doctors, just different methods of treating a disease. We use the term disease because certain components of the subluxation complex (histopathology and biochemical changes) are found in all diseases.16,17
How should we view the subluxation complex? First, it should be considered a concept or conceptual model, not as a definitive entity that exists only if all components are present. Second, the subluxation complex should be viewed as a pathology, which by definition is represented by cell and/or tissue changes or adaptations that are no longer considered normal in the context of biomechanics, biochemistry, physiology, or anatomy.17 Like other diseases, the subluxation complex has no definitive or measurable beginning point, and we cannot arbitrarily state that we have cleared our patients of this condition with an adjustment or a combination of treatments mentioned in Figure 9-1. Third, the subluxation complex should be viewed as a generator of symptoms, such as pain and visceral or autonomic symptoms.2 The subluxation complex is also likely to act as a stressor that participates in driving Selye’s general adaptation syndrome.2,18 Fourth, the subluxation complex should be viewed as a local condition that is a reflection and/or a component of systemic body dysfunction or deconditioning, i.e., ill health. The term deconditioning syndrome describes patients with (1) the degeneration and atrophy that occurs in hypomobile and hypermobile spinal tissues, referred to in this chapter as the subluxation complex, (2) a reduction in cardiovascular fitness, (3) pain, and (4) subclinical chronic inflammation that drives both the subluxation complex and other chronic diseases.8,10,19 It should be clear that the deconditioning syndrome is not a synonym for the subluxation complex; rather, the subluxation complex is a component of the deconditioning syndrome.
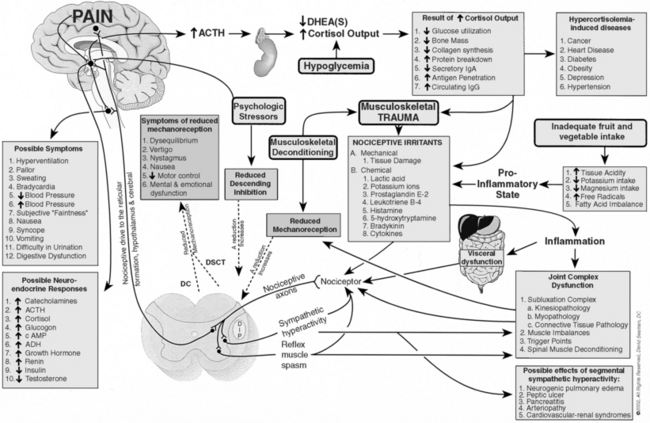
With these four perspectives of the subluxation complex in mind, the chiropractor has to make a choice. We can manipulate joints to theoretically “put bones back in place” or to “treat” mechanical low back pain, which can result in positive clinical outcomes. Or we can strive to be holistic, vitalistic doctors who offer multiple therapeutic approaches to improve both spinal and systemic function and bring the body closer to a state of optimal physical, mental, and social well-being, i.e., health. Figure 9-2 illustrates the deconditioning process and related treatments.
Subluxation Complex: A Term of Convention
Faye proposed the term subluxation complex because the classic chiropractic subluxation that conceptually eludes other practitioners and is only amenable to chiropractic care has not been demonstrated to exist. The question of whether bones do move out of place by themselves, occlude the intervertebral foramen, press on spinal nerves, and interfere with the transmission of mental impulses has not been resolved by the publication of any credible evidence that lends support to this theory, nor is there proof that this type of lesion can be corrected with an adjustment. We are not saying definitively that this historical variety of subluxation does not exist; only that convincing evidence does not support its existence or postadjustment correction. Further, our view is consistent with that of Langworthy, Smith, and Paxon, who published a text in 1906 entitled Modernized Chiropractic, wherein they proposed that chiropractic adjustments address motion restriction, not bones out of place.20
To date, a significant body of literature has demonstrated that injury and sedentary lifestyles will produce changes in spinal mobility,21–24 alterations in neurological activity,2,8,25–27 spinal muscle atrophy,28–30 histopathological changes,21,22,24 and proinflammatory biochemical changes,8,10,17 i.e., the subluxation complex. Clearly, the articular subluxation (see Part One) and the subluxation complex are different concepts about spinal dysfunction. The only similarity is the word subluxation; the modifying word complex changes the character of the lesion as outlined in Figure 9-1.
Faye would have preferred to drop the word subluxation. He knew, however, that simply trying to change the subluxation paradigm from a static and mechanistic model to a dynamic and vitalistic one would be difficult enough, much less simultaneously suggesting that we no longer utilize the word subluxation at all. The term subluxation complex was selected as a matter of convention that included a dynamic model dating back to 1906. Faye’s hope was that the chiropractic profession would move smoothly toward a dynamic model consistent with physiological and pathophysiological evidence of the day. Regrettably, this has not happened to an adequate degree, exemplified by the fact that different chiropractors, different chiropractic colleges, and different chiropractic associations define subluxation in very dissimilar fashions. (See Chapter 1.) Some still advocate the notion that subluxation is solely a bony misalignment that can be corrected by replacing the malpositioned vertebra while others embrace the “subluxation complex” but do not comprehend that it is a heuristic model.
The Subluxation Complex Is Not Synonymous with Back Pain
Pain is a symptom that is considered a component of subluxation syndromes, but it need not be present for the subluxation complex to exist. Similarly, heart disease, cancer, diabetes, Alzheimer’s disease, cirrhosis, osteoporosis, and all other chronic diseases are known to exist long before symptoms appear. Why should this be any different for the subluxation complex? Research has clearly demonstrated that pathologic changes of the spinal column, which we call the subluxation complex, may exist without symptoms. Consider that significant disc herniations can be present in individuals without back pain31 and that atrophic changes and fatty infiltration of spinal muscles exist in 45% of asymptomatic individuals.29
Strained and biomechanically stressed tissues will release chemical mediators of inflammation that constitute the biochemical changes of the subluxation complex. It is known that the cells of injured discs and joint tissue release chemical mediators, such as proinflammatory eicosanoids (prostaglandin-E2, leukotriene-B4, thromboxane-A2) and proinflammatory cytokines, such as interleukin-1 and tumor necrosis factor.32,33 These biochemical changes that we associate with the subluxation complex can stimulate spinal nociceptors and generate the back pain we commonly encounter.2,9,10 Initially, such biochemical changes can occur without obvious signs of degeneration, inflammation, and nociception and without the generation of symptoms—the way that every chronic disease begins.17
In summary, it is clearly inappropriate to equate the subluxation complex with low back pain; rather, the subluxation complex should be viewed as a promoter of low back dysfunction and as component of the deconditioning syndrome. Moreover, it is important to understand that treatment of the subluxation complex and the deconditioning syndrome does not end merely because back pain resolves.
Who Suffers with the Subluxation Complex?
It is important to recall that the subluxation complex was originally defined as a spinal condition characterized by neuropathophysiology, kinesiopathology, myopathology, histopathology, and biochemical abnormalities, pathological changes that occur in most diseases/dysfunctional tissues.17 We must further remember that the subluxation complex is merely the word chiropractors use to describe pathological changes that occur in the spine and extremities; it is not an entity that is peculiar to the chiropractic profession.
If we were to say that loss of function or motion, altered visual appearance, focal tenderness, warmth, instability, and neurovascular dysfunction are all clues that reveal the subluxation complex, most chiropractors would agree. However, such examination findings were listed in an article about sports injuries of the elbow that stated these findings “are all clues to elbow injury.”34 If a chiropractor trained in extremities were to encounter these findings, he or she might reasonably refer to the condition as a subluxation complex of the elbow.
Waddell23 explains that the key concept for osteopathy, chiropractic, manual medicine, and physical therapy is painful musculoskeletal dysfunction. This painful dysfunction arises in response to abnormal forces imposed on or generated within the musculoskeletal system that relate to abnormal posture or abnormal joint movement. He advances the term musculoskeletal dysfunction, which includes several components, such as abnormalities of posture, abnormal joint movement (hypermobility and hypomobility), muscle dysfunction, connective tissue dysfunction, muscle imbalances, and neurophysiologic changes that include abnormal sensory input and abnormal neurophysiologic processing.23 Clearly, Waddell’s description of musculoskeletal dysfunction is nearly identical to our subluxation complex. Additionally, Kirkaldy-Willis24 provides a similar description of pathological changes that occur in the spines of patients with back pain. The work of Waddell and Kirkaldy-Willis gives the distinct impression that anyone with back pain must suffer from pathological changes in the spine that chiropractors call the subluxation complex. In other words, the subluxation complex is a collection of pathologies and pain is a potential symptom.
Concerning the terminology used to describe the subluxation complex, readers should be aware that pain is an outcome of neuropathophysiology as are visceral symptoms.1,2 Consider that under normal circumstances, nociceptors are not activated. They have very high thresholds for activation, requiring a noxious, injurious stimulus. Accordingly, pain is due to tissue injury or abnormalities that initiate the firing of the normally quiescent nociceptive system. This equates with the terms neuropathophysiology or nervous system irritation when put in the context of historical subluxation complex terminology. Nerve interference is an inappropriate term when we are dealing with an increased level of nervous system activity in the presence of pain. Palmer wrote that the “transmission of physiological impulses, which by augmentation or diminution, become pathological.”35
Just how common is back pain, a neuropathophysiologic manifestation of the subluxation complex? In a study commissioned by the Merck Corporation, we are told that 9 out of 10 Americans suffer with some sort of pain.36 Low back pain remains the leading cause of lost work days and the sixth most costly medical condition with a recurrence rate of 70% to 90%,37 which suggests that the subluxation complex is a quite a common condition.
How common is the myopathology component of the subluxation complex? Lumbar paraspinal muscles in 74 so-called healthy volunteers ranging in age from 19 to 74 years were examined with MRI. Subjects in all age groups demonstrated paraspinal muscle degeneration, the degree of which increased with age. Muscle degeneration was characterized by diminished muscle size and infiltration of fat. Muscle degeneration is stated to be as common as disc degeneration in the lumbar area.28 In a follow-up study, the authors evaluated the trunk muscles in chronic low back pain patients and in matched control subjects; all participants ranged in age from 30 to 47 years. A total of 45% of so-called healthy controls were deemed to have paraspinal muscle degeneration. The percentage rises for those in the moderate and severe pain groups and actually reaches 100% in the severe pain group.29
Evidence indicates that all first-time low back pain sufferers will experience multifidus inhibition and atrophy that does not resolve spontaneously after resolution of the pain.30 Such myopathology is thought to be a reason why low back pain recurrence is so common. Exercise training to promote co-contraction of the multifidus and transverse abdominis resulted in significantly less recurrence of low back pain in the exercise group compared to controls. One year after treatment, there was a 30% recurrence of low back pain in the exercise group and an 84% recurrence in control group. Two to three years after treatment, there was a 35% recurrence in the exercise group and a 75% recurrence for controls.38
As stated above, paraspinal muscle degeneration in the lumbar spine is as common as lumbar disc degeneration. When computed tomography was utilized to study 52 “normal” subjects, it was determined that herniated discs were present in 20% of those under the age of 40 and in 27% of subjects over 40. In another study, 67 “normal” subjects were evaluated with MRI. Herniated discs were found in 20% of those younger than 60 years of age and in 36% in those older than 60 years. Degenerated discs were present in 46% of those younger than 60 years of age and in 93% in those older than 60 years.31
We should mention that we do not consider these degenerative changes in the disc to be normal merely because the patients were symptom free; rather, they represent spinal pathology, i.e., the subluxation complex, which had yet to manifest symptomatically in this cohort. Such pathological changes in the disc represent degeneration of part of the three-joint complex of the spine (two zygapophyseal joints and the intervertebral disc). This condition can lead to progressive deterioration of the spine, raising the likelihood that pain will manifest at some point in the future.24 We offer this view of disc disease for the purpose of comparing it with other degenerative diseases, such as atherosclerosis and cancer. Such diseases do not manifest symptoms for most of their course of development until the end, when it is usually too late. No one would suggest that asymptomatic cancer or atherosclerosis are not real conditions or problems that should be addressed; we believe the same holds true for the subluxation complex.
The term histopathology refers to microscopic tissue changes that occur when spinal muscles, joints, and discs undergo degeneration; it is known that all tissue degeneration is associated with histopathological changes17 and the reduced mobility promotes histopathological changes.21,22 Recent animal research by Cramer et al.39 has demonstrated that zygapophyseal joints undergo degenerative histopathological changes within four weeks of spinal immobilization. Osteophytes developed in the articular processes and degenerative changes occurred on the articular surfaces. (See Chapter 4.) We cannot clinically visualize histopathology in the spinal joint complex; however, it is important to realize that it is present in degenerated tissues and is intimately associated with biochemical abnormalities.
Herniated discs and arthritic joints are characterized by biochemical abnormalities because they produce a variety of inflammatory/nociceptive mediators including proinflammatory cytokines such as tumor necrosis factor (TNF) and interleukin-1, −6, and −8 (IL-1, IL-6, IL-8), prostaglandin E2 (PGE2), leukotriene B4 (LTB4), thromboxane A2 (TXA2), nitric oxide, histamine, and bradykinin. These mediators are produced by infiltrating macrophages and also by resident cells of the injured tissues including histiocytes, fibroblasts, myofibroblasts, endothelial cells, and chondrocytes.32,33
One outcome of inflammatory mediator release is nociception and pain. In this sense, inflammation drives the experience of pain. Because inflammation and nociception are so common in the joint complex, the use of antiinflammatory medications is significant. In the United States, more than 30 billion nonprescription NSAIDs and more than 70 million prescription NSAIDs are sold each year.40 During a 12-month period, the prescription volume for the COX2-inhibitors, Celebrex and Vioxx, exceeded 100 million.41
As described above, all of the various aspects of the subluxation complex are commonly found in the population from which our patients are derived. For this reason, it is rational to state that the subluxation complex as defined in this chapter is a common condition. We know that most people have back pain (neuropathophysiology)36,37,40,41; most people have spinal muscle degeneration (myopathology)19,28–30,38; most people have spinal disc/connective tissue degeneration (histopathology)21,22,31,39; and most people have problems with inflammation (biochemical abnormalities).32,33,40,41 Finally, movement restrictions (kinesiopathology) are a natural outcome of such degenerative changes in the joint complex, and it is agreed that reduced spinal joint motion is a common clinical finding.21–24 Additionally, spinal histopathology, myopathology, and biochemical changes are regularly discussed in refereed journals including Spine, The Spine Journal, European Spine Journal, and Journal of Spinal Disorders. Also routinely discussed are related alterations in spinal mobility (kinesiopathology) and neurological changes (neuropathophysiology), such as increased nociception, that typically lead to the experience of pain.
Bone-out-of-Place Subluxation versus Mechanical Low Back Pain
The reductionist approach to back pain has recently been modified, and we are now told that back pain has mechanical, chemical, and psychological causes,42 echoing the words of D.D. Palmer some 100 years ago when he wrote that disease is cause by trauma, toxins, and autosuggestion.35
The Subluxation Complex as a Pathological Process
On a practical level “pathology deals with the study of deviations from normal structure, physiology, biochemistry, and cellular and molecular biology.”16 The subluxation complex generally refers to pathological changes that occur in the spine,4–6 and its clinical character depends on the combination of injured tissues and the extent of injury.
As stated earlier, Palmer35 explained that trauma, toxins, and autosuggestion are the determining causes of disease. We are exposed to such injurious stimuli over a lifespan and, sooner or later, the outcome is pathology; when this occurs in the spine and extremities, we refer to it as the subluxation complex. Back pain researchers agree and indicate that the risk of developing low back pain is greater when there is a lack of fitness or the person is in poor health (a predisposition to trauma), when there are psychosocial issues (autosuggestion), and if one is a smoker (i.e., toxins),43 which dispels the foolish idea that back pain is solely mechanical.
D.D. Palmer’s view of disease is also consistent with the writings of modern pathology. Pathology is known to be caused by diverse agents, including oxygen deprivation, physical agents, chemical agents and drugs, infectious agents, immunologic reactions, genetic derangements, and nutritional imbalance.17 These injurious agents are known to express injury potential in the same fashion. No matter if the cause of the initial injury was physical, hypoxic, or infectious, five stereotypical biochemical themes will mediate the expression of cell injury and cell death, including (1) defects in cell membrane permeability, (2) free radicals, (3) ATP depletion, (4) intracellular calcium and loss of calcium homeostasis, and (5) irreversible mitochondrial damage.17 These biochemical themes apply to all pathologies, suggesting that we must consider them in the context of the subluxation complex.
Biochemical Injury Theme 1: Defects in the Cell Membrane
Each cell type found in the spine contains an external limiting membrane called the plasma membrane, or cell membrane, a dynamic structure consisting of various lipids, proteins, and carbohydrates. It is intimately connected with the extracellular compartment by numerous membrane receptors that signal the intracellular compartment. The lipid component of the cell membrane is extremely important for membrane fluidity and in the context of creating inflammatory potential. Phospholipids and cholesterol are the lipid substances that make up the cell membrane and generally are present in a 1 to 1 ratio.44
The phosphatide portion and saturated fatty acid are assembled within the body. The polyunsaturated fatty acid is obtained from our diets and is referred to as an essential fatty acid, either an omega-6 (n6) or omega-3 (n3) fatty acid. Omega-6 and omega-3 fatty acids are found in both vegetable and animal foods, and a 1:1 dietary ratio is thought to be ideal for promoting appropriate inflammatory and healing responses.45 Ratios greater than 3:1 are thought to promote excessive inflammatory responses.
Linoleic acid is found in all grains and grain products, such as cereal, pasta, and bread; the average n6:n3 ratio is 20:1 for these foods.46 Seeds contain almost exclusively n6 fatty acids, as do their oils including corn, sunflower, and safflower oils. This creates a ratio that exceeds 100:1. Peanuts, a legume and not a nut, have ratios that also exceed 100:1.47 Processed foods that have n6 oils added to them have very high ratios, such as potato chips that boast 60:1.46 Meat and eggs from grain-fed animals have ratios well above 3:1.48,49
Linolenic acid is the n3 fatty acid that we convert into eicosapentaenoic acid (EPA), which is then inserted into the cell membrane phospholipid. EPA is the precursor to antiinflammatory eicosanoids (prostaglandin E3, leukotriene B5, and thromboxane A3). In foods such as fruits and vegetables, the n6:n3 ratio is quite favorable, ranging from about 3:1 to 1:3.46 Fish, grass-fed beef, and wild game range from about 3:1 to 1:7.46,48,49
With a 1:1 dietary ratio of linoleic (n6) to linolenic acid (n3), we would get a similar ratio of arachidonic acid to eicosapentaenoic acid, allowing for an appropriate inflammatory response. However, the dietary ratio of n6 to n3 fatty acids has been maintained at about 20:1 or greater for the past half-century or longer,45 resulting in an excessive and persistent inflammatory response and an increased incidence of inflammatory diseases such as cancer, heart disease, Alzheimer’s disease, and arthritis.10,45
In the context of cells and tissues directly related to the subluxation complex, research has shown that normal cartilage has low levels of pro-inflammatory n6 fatty acids. As we age, concentrations steadily increase—a trend that is especially pronounced in osteoarthritic cartilage. Lipid accumulation in chondrocytes generally precedes local tissue degeneration in several models of degenerative arthritis. Histological severity of osteoarthritis has been related to accumulation of arachidonic acid,50 an n6 acid and a precursor of the previously mentioned proinflammatory eicosanoids.
Biochemical Injury Theme 2: Free Radicals
Pathology texts tell us that cell membranes, enzymes, circulating lipids, and DNA are at risk of injury from free radicals.17 In particular, consider that free radicals can damage cell membranes, resulting in the release of arachidonic acid and its subsequent conversion to proinflammatory eicosanoids. Thus there is interplay between biochemical injury themes 1 and 2.
Free radicals are generated by many normal body reactions. The free radicals that are most compromising to us are the ones produced by our own bodies. Consider that immune cells fend off invaders by releasing free radicals that can also damage cell membranes. Internal biological processes, including ATP synthesis, liver detoxification processes, prostaglandin synthesis, phagocytosis, xanthine oxidase, and the normal degradation of catecholamines,51 also generate free radicals. Even at rest we produce free radicals; production increases during exercise.52
Although free radicals are produced by our bodies, we need outside support if we are to mount an effective defense against them. Only through the liberal consumption of fruits and vegetables are we able to provide our bodies with the antioxidant nutrients needed to fight free radical activity. The consumption of olive oil and red wine also provides powerful antioxidants.53 Additionally, recent research has demonstrated that restricting caloric intake is an effective way to reduce the body’s generation of free radicals.54,55
It is thought that free radical attack may be one of the final common denominators of cell injury. Such attacks may be responsible for the progression of all diseases,56 including conditions that are considered to be components of or related to the subluxation complex, such as disc herniation. Lipofuscin, known as the aging pigment, is produced by the oxidation of lipids or lipoprotein. At the time of disc surgery, lipofuscin has been found in regions associated with strong histologic degeneration, including the nucleus pulposus and the inner and middle layers of the anulus fibrosis. Lipofuscin was found in the discs of individuals older than 20 years of age.57
Free radicals are also involved in articular cartilage degeneration and arthritis, with chondrocytes playing a significant role. Although we typically view them as producers of cartilage, we saw earlier that their cell membranes concentrate arachidonic acid and become proinflammatory.50 These small cells are also able to generate abnormal production of a hydrogen peroxide free radical that can damage joint cartilage proteoglycans, hyaluronic acid, and collagen.50,58 Chondrocytes from osteoarthritic cartilage also release proinflammatory inducible nitric oxide, which acts as a potent free radical.59 It is also known that a chondrocyte-derived lipid peroxidation product called malondialdehyde (MDA) mediates oxidation of cartilage collagens. White cells such as macrophages are a likely source of the free radicals that induce the production of MDA via oxidization of the fatty acids within the phospholipids of chondrocyte cell membranes.60
Biochemical Injury Themes 3 to 5: Related to ATP Synthesis
The final three themes that mediate the expression of cell injury include ATP depletion, intracellular calcium and loss of calcium homeostasis, and irreversible mitochondrial damage. They are described collectively because they are interrelated. For example, mitochondrial damage will deplete ATP, which can disrupt calcium homeostasis. Calcium ions are highly concentrated in the extracellular compartment. Without adequate mitochondrial function and ATP synthesis, excess calcium may enter the cell and cause cell injury and death.17 The seriousness of this relationship should not be taken lightly because most diseases are likely to be driven at least in part by this process, including the normal aging process.17,61–64
The cellular synthesis of ATP utilizes three biochemical pathways. Glycolysis occurs in the cytoplasm; the Krebs cycle and electron transport occur in the mitochondria. Tissues highly dependent on oxygen and ATP, such as the cardiac muscle, skeletal and smooth muscle, the central and peripheral nervous system, the kidney, and pancreatic beta cells are especially susceptible to defective mitochondrial function. There is evidence that mitochondrial dysfunction and reduced ATP synthesis play an important role in atherosclerosis, Alzheimer’s disease, Parkinson’s disease, diabetes, and aging.62
The interrelationship among the biochemical themes of injury continues here because it is known that free radicals damage mitochondria. During a lifetime, mitochondrial DNA (mtDNA) undergoes a variety of mutations. The bioenergetic decline associated with mitochondrial mutations, often coupled with nuclear DNA damage, are thought to contribute to the reduced function of cells and organs, especially in postmitotic tissues.63 On a histological level, postmitotic tissues such as skeletal muscle develop what has been referred to as a “damage mosaic.”63 Skeletal muscle atrophy and muscle fiber type changes occur.63 Between the ages of 20 to 80, there is about a 40% decrease in skeletal muscle mass.64 Such changes clearly have an impact in the manner in which we view the subluxation complex as our patients age.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree