and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
Excessive soft-tissue laxity is frequently encountered in severely deformed arthritic knees undergoing TKA. It is usually uni- or biplanar where the lateral side (in varus deformity) or medial side (in valgus deformity) shows excessive laxity with or without an associated posterior laxity (in hyperextension deformity). However, rarely, an arthritic knee undergoing TKA may also show multiplanar or global laxity where there is significant medial, lateral and posterior ligamentous insufficiency along with significant bone loss. Although extremely rare in osteoarthritis or rheumatoid arthritis, severe or global knee instability may be secondary to a neuromuscular disorder (such as post-poliomyelitis, spinal neuropathy) or due to post-traumatic global ligamentous insufficiency.
Introduction
Excessive soft-tissue laxity is frequently encountered in severely deformed arthritic knees undergoing TKA [1]. It is usually uni- or biplanar where the lateral side (in varus deformity) or medial side (in valgus deformity) shows excessive laxity with or without an associated posterior laxity (in hyperextension deformity) [2]. However, rarely, an arthritic knee undergoing TKA may also show multiplanar or global laxity where there is significant medial, lateral and posterior ligamentous insufficiency along with significant bone loss. Although extremely rare in osteoarthritis or rheumatoid arthritis, severe or global knee instability may be secondary to a neuromuscular disorder (such as post-poliomyelitis, spinal neuropathy) or due to post-traumatic global ligamentous insufficiency [2–7].
Lack of competent and functional collateral ligaments makes it extremely difficult for the surgeon to achieve optimum soft-tissue balance in an unstable knee using conventional cruciate-substituting implants. This gets even more challenging when the knee has an associated hyperextension due to lax and stretched out posterior soft-tissue structures. Hence, an unstable knee is one of the rare occasions where a constrained or hinged prosthesis may be required during primary TKA. This chapter outlines the management of instability during primary TKA.
Pathoanatomy
Severe arthritic knee deformities are associated with significant tibio-femoral bone erosions and adaptive changes in the periarticular ligaments and soft tissues. In varus deformities, bony erosion of the medial tibia and femur, periarticular inflammation and osteophytes cause gradually relative shortening and stiffness of the medial soft-tissue structures [2]. The patient subsequently walks with a varus moment at the knee causing gradual adaptive elongation of the lateral soft-tissue structures [2]. Hence, severe varus deformities typically present with medial soft-tissue contracture and excessive laxity on the lateral side. Similarly, in valgus knees, the lateral soft-tissue structures show contracture and there is laxity on the medial side. This scenario may be compounded by additional laxity or contracture of posterior soft-tissue structures if there is an associated hyperextension or flexion deformity. This complex situation results in medio-lateral as well as flexion-extension gap asymmetry.
Although most arthritic knees undergoing TKA can be dealt with using standard cuts, graduated soft-tissue release and a cruciate-substituting knee design, knees with significant laxity or instability need to be tackled differently.
Based on the authors’ experience, instability encountered in arthritic knees undergoing TKA can be classified into three types (Table 10.1): Type 1, severe coronal plane (medial or lateral) laxity; Type 2, severe coronal (medial or lateral) and sagittal plane (posterior) laxity; and Type 3, global (medial, lateral and posterior) laxity. In Type 1 instability, the lateral (in varus deformity) or medial (in valgus deformity) soft-tissue structures may show significant laxity and pose a challenge in equalising the medio-lateral gap balance (Fig. 10.1). In Type 2 instability, in addition to the lax lateral or medial soft-tissue structures, the posterior structures may be attenuated due an associated hyperextension deformity (Fig. 10.2). In Type 3 instability, three sides of the knee (medial, lateral and posterior) shows significant laxity and the patient may present with a subluxated or a dislocated knee joint (Fig. 10.3).
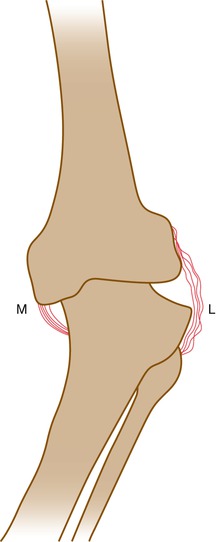
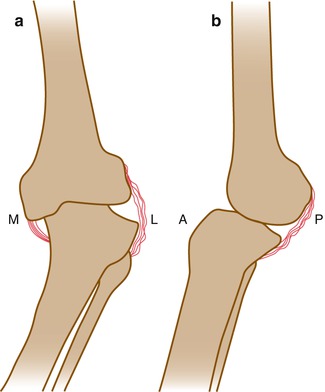
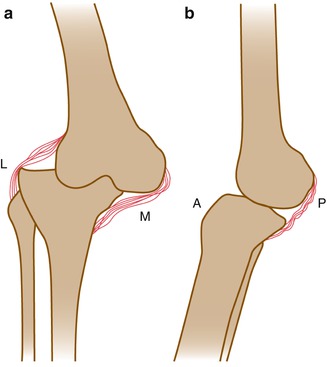
Table 10.1
Classification of instability
Type 1: Severe coronal plane (medial or lateral) laxity |
Type 2: Severe coronal (medial or lateral) and sagittal (posterior) plane laxity |
Type 3: Global (medial, lateral and posterior) laxity |
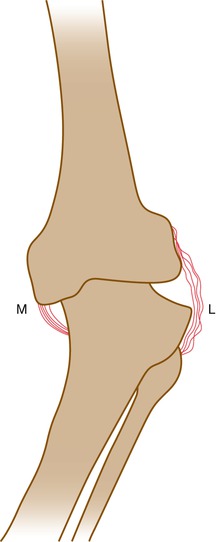
Fig. 10.1
Type 1 instability. The lateral side (L) in varus knees or the medial side (M) in valgus knees shows excessive laxity
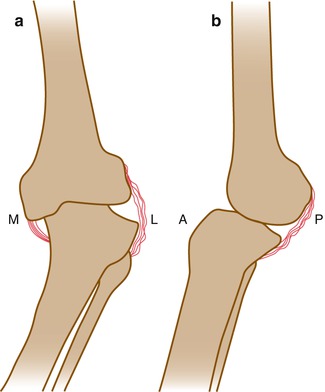
Fig. 10.2
Type 2 instability. The lateral side (L) in varus knees or the medial side (M) in valgus knees (a) and the posterior aspect (P) of the knee (b) show excessive laxity
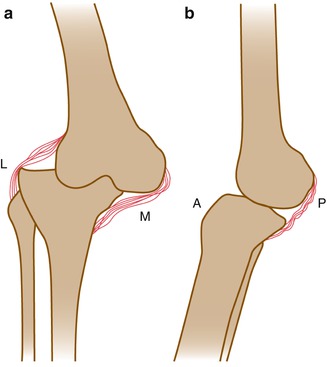
Fig. 10.3
Type 3 instability. The lateral (L), medial (M) (a) and posterior (P) aspect (b) of the knee show excessive laxity
Global laxity as seen in Type 3 instability, although rare, is usually associated with an underlying neuropathic component (Fig. 10.4). A common cause for it is spinal degeneration and the resulting neuropathy involving both lower limbs. Furthermore, many of these patients have not been walking due to severe arthritic pain and knee instability, and the resultant muscular atrophy especially of the knee extensors accentuates posterior instability. Hence, such patients with Type 3 instability who undergo TKA will require prolonged postoperative physiotherapy to improve muscle strength around the knee joint and treatment of the underlying neuropathy.


Fig. 10.4
Clinical photographs of a patient showing global or Type 3 instability. (a) Excessive laxity on the lateral side on applying a varus stress at the knee. (b) Excessive laxity on the medial side on applying a valgus stress at the knee. (c) Excessive laxity posteriorly resulting in a hyperextension deformity at the knee
Surgical Technique
In view of excessive laxity and bony erosion commonly associated with unstable knees, the tibial and the distal femoral cuts need to be conservative (typically less than 8 mm). However, in Type 1 instability where the patient has an associated fixed flexion deformity, the tibial cut needs to be adequate (8–10 mm) since the extension gap may be smaller when compared to the flexion gap. Surgical technique may have to be modified based on the type of instability present.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








