The Thoracolumbar Spine
Donald Chow MD, FRCSC, Dipl Sports Med
The majority of thoracolumbar spine injuries arising from low-velocity sports usually are less catastrophic than some of the athletic injuries involving the more vulnerable cervical spine. The thoracic spinal cord is protected by the relatively larger and less mobile thoracic vertebra and rib cage.
The sports physician may be required to assess for a spinal problem in situations varying from an unconscious athlete on a steep ski slope to a preparticipation examination in a sports medicine clinic.
If the patient has any disorientation or depressed level of consciousness, the spine should be protected with a cervical collar and with log-roll precautions for the lumbar spine.
The primary concern of a sports physician for a severely traumatized athlete should be to assess the airway once the cervical spine has been immobilized, followed by a rapid survey of respiratory and circulatory function.
The initial investigation for the majority of athletes with thoracolumbar pain includes plain-film anteroposterior (AP) and lateral radiographs. The AP view will depict the sagittal alignment as well as congenital anomalies at the thoracolumbar and lumbosacral junction.
The use of computed tomography (CT) enhances the evaluation of osseous structures. This modality better depicts the contents of the spinal canal and any small, lytic lesions in the bone.
Magnetic resonance imaging (MRI) is now the modality of choice to evaluate soft tissues of the thoracolumbar spine. An MRI can depict nerve root compression with various degrees of disc degeneration, ligamentous injury, hematoma formation, and soft-tissue tumors.
The use of blood work, such as a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein, and blood cultures, may be useful to confirm and follow spinal infections.
Management of the athletic spine by the sports physician may vary from the preparticipation examination of an asymptomatic athlete to on-field stabilization of an acute injury in an athlete with neurological deficits. The majority of thoracolumbar spinal injuries may be relatively minor and self-limiting. The incidence of these injuries may vary greatly, ranging from 7% to 27% (1). Serious thoracolumbar injuries may be relatively rare; however, the fear of major neurological loss or mechanical instability may make return to play a difficult task for the athlete. Several comprehensive reference texts are available to the spinal specialist (2,3), so the goal of this chapter is to provide the sports physician with the basic tools for assessing and managing the athlete’s spine.
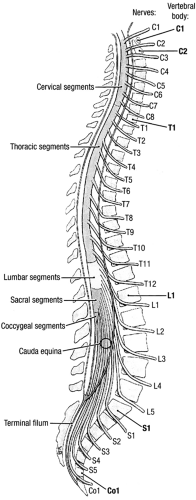
A good background in the anatomy and clinical biomechanics of the thoracolumbar spine will provide the basis for understanding the mechanisms of injury and the principles of management (4). The majority of thoracolumbar spine injuries arising from low-velocity sports usually are less catastrophic than some of the athletic injuries involving the more vulnerable cervical spine. The thoracic spinal cord is protected by the relatively larger and less mobile thoracic vertebra and rib cage. The spinal cord has outer white matter, which contains the myelinated nerve fibers that form the ascending sensory and descending motor tracts. The gray
matter within the spinal cord contains the cell bodies of the nerve roots and is vulnerable to irreversible damage if compressed. The cord ends with the conus medullaris at the level of the L1 vertebra. The spinal nerves, which arise from the cord, usually can re-innervate after a compression injury similar to a peripheral nerve after a compression injury. The cauda equina is a collection of spinal nerves below the level of the conus. The cord and spinal nerve roots are suspended in cerebrospinal fluid contained within the dura mater (5) (Fig 6-1).
matter within the spinal cord contains the cell bodies of the nerve roots and is vulnerable to irreversible damage if compressed. The cord ends with the conus medullaris at the level of the L1 vertebra. The spinal nerves, which arise from the cord, usually can re-innervate after a compression injury similar to a peripheral nerve after a compression injury. The cauda equina is a collection of spinal nerves below the level of the conus. The cord and spinal nerve roots are suspended in cerebrospinal fluid contained within the dura mater (5) (Fig 6-1).
The human body has 12 thoracic and 5 lumbar vertebrae, which consist of the vertebral bodies that support the trunk and the neural arch that protects the neural elements. Transverse and spinous processes act as lever arms to attach the stabilizing muscles and ligaments. The thoracic vertebrae provide attachment of the supporting rib cage at the costovertebral and costotransverse junctions. This buttressing by the “nonfloating” ribs on the neural arch may protect the posterior half of the thoracic vertebral body from axial loading, thus explaining the relatively small incidence of burst fractures in the T1 to T10 levels (6).
The vertebrae articulate with each other by means of a fibrocartilagenous intervertebral disc, two facets joints, and numerous intervertebral ligaments. The avascular disc has an outer, fibrous annulus and an inner, gelatinous nucleus pulposus. The end plates are hyaline cartilage that distributes the pressure of axial loading and allows the diffusion of nutrients into the discs from the adjacent subchondral bone. The disc annulus has innervation only to the outermost layer. This explains the asymptomatic, degenerative tears of the inner annulus layers and the severe pain and reflex spasms that occur with outer annular tears and disc herniations, even when the nerve roots are not being compressed.
The facets are synovial joints on the posterior neural arch that are oriented along the coronal plain in the thoracic spine and the more sagittal orientation in the lumbar spine. This orientation of the thoracic spine facets is more suitable for flexion and rotation, whereas the lumbar facets may allow relatively more flexion and extension as well as lateral bending (4).
The area of bone that connects the lamina to the pedicles and is between the superior and inferior facets is called, appropriately, the pars interarticularis. This portion of the bony neural arch forms the roof of the neural foramina for the exiting nerve roots. A defect in the pars is known as a spondylolysis. This pseudoarthrosis may become painful when compressed between the inferior facet of the cephalad vertebra and the superior facet of the vertebra caudal to the pars involved. The soft tissue of the defect may be a fibrous or a pseudosynovial junction, which may enlarge and compress the exiting nerve root beneath it.
Spondylolisthesis is the forward translation of one vertebral body over another. In athletes, it usually is related to a spondylolysis, because the supporting posterior facets have lost the osseous continuity with the vertebral body. In the older population, degeneration of the facets may lead to an unstable forward translation despite having an intact pars interarticularis. This condition is known as a degenerative spondylolisthesis.
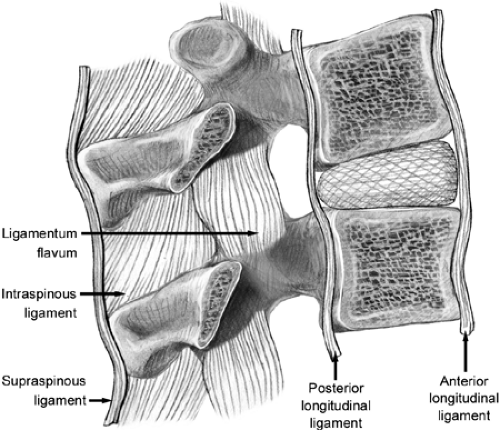
The intervertebral ligaments and thoracolumbar musculature receive the least clinical attention but are the most responsible for providing dynamic stability (7). These well-innervated soft tissues also are the structures involved in the majority of symptomatic spinal injuries, which can be classified as minor strains or sprains. The anterior longitudinal ligament resists hyperextension, whereas the intraspinous,
supraspinous, and facet capsular ligaments resist hyperflexion forces. The ligamentum flavum, which connects the adjacent lamina, is unique in that it contains elastin fibers that allow a tension spring action instead of the fixed-length rope restraints of other ligaments containing predominately collagen fibers (Fig 6-2).
supraspinous, and facet capsular ligaments resist hyperflexion forces. The ligamentum flavum, which connects the adjacent lamina, is unique in that it contains elastin fibers that allow a tension spring action instead of the fixed-length rope restraints of other ligaments containing predominately collagen fibers (Fig 6-2).
The musculature of the thoracolumbar spine can be divided into three groups: superficial, intermediate, and deep. The superficial group consists of the trapezius, latissimus dorsi, the levator scapulae, and the rhomboids, and it helps to stabilize the shoulder girdles. The intermediate muscles of the back consist of the serratus posterior, both superior and inferior, that assist in respiration. The deep muscles of the spine are known as the intrinsic muscle; these include the erector spinae and transversospinalis group of muscles. The intrinsic muscles stabilize the local vertebrae for movements such as extension, rotation, and lateral bending of the spine.
The abdominal muscles of the thoracolumbar spine can be divided into the anterior and posterior groups. The abdominal muscles along with the diaphragm help to stabilize the mobile lumbar vertebra. The rectus abdominis, external oblique, internal oblique, and transversus abdominis muscles form the anterior lateral group. The posterior group includes the psoas, iliacus, and quadratus lumborum muscles (4).
White and Panjabi (7) have defined clinical instability as “the loss of ability of the spine under physiological loads to maintain relationships between vertebra in such a way that there is either damage or subsequent irritation to the spinal cord or nerve roots. In addition there is development of incapacitating deformity or pain due to structural changes.” Clinical instability may result from trauma, degeneration, surgery, or pathologic disease, such as neoplastic or infectious conditions. White and Panjabi (7) also have developed a checklist for thoracic and thoracolumbar instability (Table 6-1).
Table 6-1 Checklist for the Diagnosis of Clinical Instability of the Thoracic and Lumbar Spine | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
History
The sports physician may be required to assess for a spinal problem in situations varying from an unconscious athlete in a difficult environmental presentation, such as on a steep ski slope or in a crumpled racecar, to a preparticipation examination in a sports medicine clinic. The history may be the most important aspect of a clinical evaluation; however, the details of the incident may have to come from on-field officials or other participants if the athlete has a diminished level of consciousness. Occasionally, the true story is not known until videotapes of the incident reveal the directions and magnitude of the force vectors to which the athlete’s spinal column was exposed. Finding or excluding the presence of a spinal injury is much simpler in an alert, awake patient with no other distracting injuries. If the patient has any disorientation or a depressed level of consciousness, the spine should remain protected with a cervical collar and with log-roll precautions for the lumbar spine. Even when the athlete regains consciousness, he or she may have retrograde amnesia of the accident. The firm spine board used for immobilization during patient transport should be removed as soon as possible to prevent serious decubitus ulcers (8).
The most common symptom following injuries to the thoracolumbar spine is pain, and the details regarding the time of onset, quality, location, alleviating and aggravating factors
must be obtained. Associated symptoms, such as weakness and numbness, are important in localizing the area of injury. Constitutional symptoms, such as fever, fatigue, unexplained weight loss, or night pain, may raise flags to investigate for other diseases, such as infections or neoplasms, that may lead to a pathologic fracture of the spine during a session of athletic activity. The location of the predominant pain will be important in determining the neurological status of the condition. The sharp, electrical pain shooting down a single dermatome to the toes is a classical sign of nerve root irritation and is known as radicular pain. When this occurs with nerve roots that form the sciatic nerve (L4, L5, and S1), the term sciatica is used. The term femoratica describes the radicular pain in the dermal distribution of the nerve roots forming the femoral nerve (L2, L3, and L4). If low back pain is predominant with a diffuse, dull aching in the buttocks or upper thighs, this is likely to be referred mechanical back pain. This type of referred pain is best explained to the patient using the classical left arm pain of coronary angina as an example. The converse also is possible, in that conditions in the hips, pelvis, and abdomen may refer pain to the thoracolumbar spine area. Renal calculi, which may be more common in athletes who experience frequent dehydration, may first present with episodes of severe lumbar pain.
must be obtained. Associated symptoms, such as weakness and numbness, are important in localizing the area of injury. Constitutional symptoms, such as fever, fatigue, unexplained weight loss, or night pain, may raise flags to investigate for other diseases, such as infections or neoplasms, that may lead to a pathologic fracture of the spine during a session of athletic activity. The location of the predominant pain will be important in determining the neurological status of the condition. The sharp, electrical pain shooting down a single dermatome to the toes is a classical sign of nerve root irritation and is known as radicular pain. When this occurs with nerve roots that form the sciatic nerve (L4, L5, and S1), the term sciatica is used. The term femoratica describes the radicular pain in the dermal distribution of the nerve roots forming the femoral nerve (L2, L3, and L4). If low back pain is predominant with a diffuse, dull aching in the buttocks or upper thighs, this is likely to be referred mechanical back pain. This type of referred pain is best explained to the patient using the classical left arm pain of coronary angina as an example. The converse also is possible, in that conditions in the hips, pelvis, and abdomen may refer pain to the thoracolumbar spine area. Renal calculi, which may be more common in athletes who experience frequent dehydration, may first present with episodes of severe lumbar pain.
The classical neurogenic claudication symptoms of leg pain and weakness brought on by activities with the spine extended and relieved with flexion of the lumbar spine are suggestive of spinal stenosis. Although this usually is seen in elderly patients, the problem also can occur in younger adults who have the underlying condition of shorter pedicles (commonly reported by radiologists as having congenital spinal stenosis). Typically, these athletes may have difficulty walking more than 100 meters yet will be able to bike more than 10 kilometers. The diagnosis can be confirmed with further spinal imaging.
The patient’s past medical, surgical, family, and social history may be very helpful. This can be especially true in cases of nontypical mechanical or radicular back pain.
Myelopathy resulting from spinal cord compression or vascular insufficiency may involve little or no back pain. Neurological deficits, such as loss of balance, weakness, and numbness, may be the first symptoms. Painless myelopathy needs further investigation to check for neuropathies, such as multiple sclerosis, amyotrophic lateral sclerosis (Lou Gerhig’s disease), or transverse myelitis.
Physical Examination
The examination of the injured athlete’s spine initially may be limited to a cursory four-limb sensory and voluntary motor assessment along with palpation of the entire spine for point tenderness during the log-roll onto a spine board for transport off the playing field. The primary concern of the sports physician with a severely traumatized athlete should be to assess the airway with cervical spine immobilization, followed by a rapid survey of the respiratory and circulatory function. If immediately life-threatening injuries are identified, these are attended to as part of the primary survey (8). The initial palpation of the spine may reveal the location of point tenderness or a deformity, such as a step or gap between spinous processes. A definite motor or sensory level on the trunk indicates a significant spinal injury, and urgent transfer to a medical center capable of investigating and comprehensively treating spinal injuries is required. Gentle testing for hip flexion power with resistance to contraction of the iliopsoas muscle may lead to inhibition of pain if a thoracolumbar fracture is present.
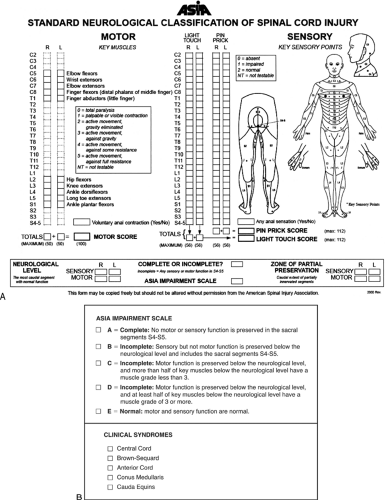
Once a patient is off the field and stabilized hemodynamically, a detailed examination documenting the neurological status is required. The Standard Neurological Classification of Spinal Cord Injury form, which is available from the American Spinal Injury Association, provides easy charting of the patient’s neurological status (Fig 6-3).
The ambulatory athlete with a thoracolumbar spinal injury will include tests to determine neurological deficit, signs of nerve root irritation, any loss of spinal range of motion, and the exact location of tenderness, pain radiation, or paresthesias. Special maneuvers to reproduce the pain also should be carried out (2).
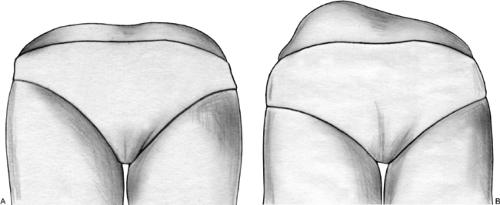
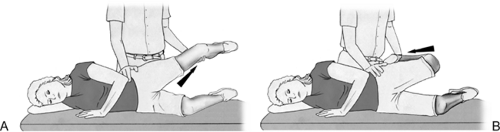
Inspection of the spine for deformity and loss of sagittal trunk balance can be carried out with the standing patient. Also, bruising, café-au-lait spots, or abnormal hair tufts may indicate other underlying pathology. Paraspinal spasm may cause a postural scoliosis and limitation of forward flexion because of pain. Structural scoliosis involves a rotation of the vertebrae and can be detected on the forward-bending test (Fig 6-4). Range-of-motion testing may indicate the location of the source of pain. Pain with trunk extension may be an indication that pain is coming from the posterior elements of the neural arch, such as degenerative facets or a pars defect of spondylolysis. Severe reproduction of shooting pain with forward bending may indicate disc herniation. Reproduction of the shooting pain with straight-leg raise test (the Leseque test) along with the Cram test (positive bowstring sign) indicates irritation of the nerve roots that form the sciatic nerve. Similarly, the femoral nerve stretch test, which flexes the knee while the hip is extended, will detect irritation of the upper lumbar roots that form the femoral nerve (Fig 6-5). The neurological examination will match the clinical relationships with deficits of sensory, reflexes, and motor testing to determine the neurological level. For example, the S1 level deficits will have numbness to the lateral aspect of the foot with weakness of the gastrocnemius muscle and either a diminished or absent Achilles tendon reflex. The patellar tendon reflex may be affected by L3 or L4 nerve root compression. It should be noted that the L5 nerve root does not have a reliable reflex test, but the tibialis posterior tendon may show a slight response (9). The Babinski test is useful in detecting myelopathy. However, it may be positive in patients with brain injury. The rectal examination may be used to check for sacral nerve root or sacral cord segment involvement. In a paraplegic patient
lacking both power and sensation in the lower extremities, the presence of perianal sensation and voluntary contraction of the anal sphincter is an indication of a partial cord injury known as sacral sparing.
lacking both power and sensation in the lower extremities, the presence of perianal sensation and voluntary contraction of the anal sphincter is an indication of a partial cord injury known as sacral sparing.
Cauda equina syndrome occurs with the acute severe compression of the spinal nerves in the lumbar spinal canal and is characterized by bowel and bladder dysfunction. The loss of anal sphincter tone leads to fecal incontinence, and the loss of the bladder tone leads to urinary retention. Severe nerve root irritation signs are found on physical examination.
Examination of the pelvis, with particular attention to the sacroiliac and hip joints, should be performed. The range of motion of the sacroiliac joints is minimal because of the extensive fibrous anterior and posterior ligaments as well as the irregular articular surfaces. In relatively high-velocity impact trauma, the athlete may sustain unstable pelvic injuries that result in open-book or closed-book movement of the iliac wings relative to each other. If vertical shifting of a hemipelvis is present, this indicates a major disruption of the posterior hemipelvis, which would be very unstable for any weight bearing on the ipsilateral limb. These severe pelvic injuries may be associated with spinal fractures as well as hemodynamic instability resulting from massive bleeding into the retroperitoneum.
Most injuries of the lumbar spine may involve tenderness over one or both sacroiliac joints, because the majority of the intrinsic muscles of the lumbar spinal area have their origin on the posterior capsule and/or the bones adjacent to the sacroiliac joints. Stressing of the sacroiliac joints to reproduce pain originating from within the joint can be done with the Patrick test, which involves flexion, abduction, and external rotation of the hip while counterpressure is applied on the contralateral iliac wing. When the sacroiliac joint is inflamed or unstable after trauma, reproduction of the severe
low back pain can occur with this maneuver. In patients with inflammation of the hip joint itself, the pain that is produced by the Patrick test may be referred to the anterior hip and groin region (Fig 6-6).
low back pain can occur with this maneuver. In patients with inflammation of the hip joint itself, the pain that is produced by the Patrick test may be referred to the anterior hip and groin region (Fig 6-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree