Scapulothoracic Dysfunction, Burners, Stingers, Thoracic Outlet Syndrome, and Miscellaneous Nerve Injuries
Marc R. Safran MD
Anthony C. Luke MD, MPH
The scapula is a triangular, flat bone that lies along the posterior thoracic wall. The stability of the scapula depends mainly on the 17 muscles that are attached to it.
The scapula is an essential structure for proper biomechanics for the shoulder, because it offers a stable foundation for movement. Disorders of the scapula and the nerves surrounding the glenohumeral joint can result in significant dysfunction and pain involving the shoulder.
Scapular “dyskinesis” describes loss of the normal motion and positioning of the scapula.
The patient with a scapular problem often presents with a history of shoulder impingement or pain. Common complaints among throwing athletes are difficulties generating force and pain over the posterior aspect of the shoulder.
Blunt trauma or repetitive microtrauma from nerve traction or compression are the common causes of neurogenic winging encountered in athletes. The long thoracic nerve is vulnerable to direct injury because of its subcutaneous location as it exits the pectoralis muscle at the fourth and fifth ribs and travels along the rib cage.
Brachial plexus neuropathy presents with temporary burning, stinging, or tingling that occurs when the head is forcefully bent sideways. These injuries are commonly referred to as stingers or burners. Symptoms typically last for seconds to minutes, but in 5% to 10% of cases, a neurological deficit can last for hours, days, or even weeks. When treating the symptoms, it is important to rule out underlying factors that may predispose the athlete to more serious injury.
Nerve compression, nerve traction, or a direct blow to the brachial plexus are the three main mechanisms for a stinger or burner.
Thoracic outlet syndrome (TOS) refers to a symptom complex of upper extremity pain and paresthesias involving compressions of neurovascular structures.
A subtle cause of shoulder pain and weakness involves compression or traction of the suprascapular nerve. Overhead and throwing athletes often are affected because of repetitive trauma. A diagnosis of suprascapular nerve entrapment often is made clinically, based on a thorough history and physical examination.
Apart from the pathology of the glenohumeral joint, disorders of the surrounding nerves and scapula can result in significant dysfunction and pain involving the shoulder. The scapula is an essential structure for proper biomechanics of the shoulder, because it offers a stable foundation for movement. Proper coordination and positioning of the scapula and glenohumeral joint is necessary for efficient and effective shoulder motion. Nerve injuries around the shoulder can cause weakness of the scapular stabilizers and the rotator cuff muscles, which can result in improper and symptomatic mechanics of the shoulder. This chapter reviews problems involving the scapula and the nerves around the shoulder that often are overlooked and, possibly, underdiagnosed. The concept of scapulothoracic dysfunction or dyskinesis is introduced, and specific nerve injuries around the neck and shoulder are discussed.
Scapular “dyskinesis” describes loss of the normal motion and positioning of the scapula (1). Several specific pathologies are associated with abnormal function of the scapula.
Scapular dyskinesis, scapular crepitus or “snapping scapula,” and scapular bursitis are discussed in this section, and scapular winging caused by nerve injuries are discussed in the following section.
Scapular dyskinesis, scapular crepitus or “snapping scapula,” and scapular bursitis are discussed in this section, and scapular winging caused by nerve injuries are discussed in the following section.
Basic Science
Anatomy
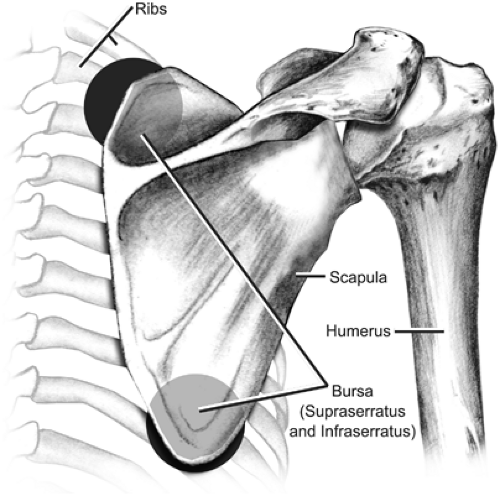
The scapula is a triangular, flat bone that lies along the posterior thoracic wall. The “plane of the scapula” at rest is approximately 30 to 40 degrees in the frontal plane and is tipped anteriorly by approximately 10 to 20 degrees (2). Its attachment to the axial skeleton involves the acromioclavicular and sternoclavicular joints and the clavicle, which acts as a strut (3). The stability of the scapula depends mainly on the muscle attachments and their dynamic stabilizing functions. Seventeen muscles have their origin or insertion on the scapula (4). The subscapularis and the serratus anterior muscles lie between the scapula and the thoracic wall. Several bursae also exist around the scapula, between it and the chest wall. Anatomical bursae include the infraserratus and supraserratus bursa, and adventitial bursae can develop, particularly around the superomedial angle and the inferior angle (5) (Fig 8-1). Some experts believe that these occur as an adaptation to repetitive movements or abnormal mechanics around the scapula. Cadaveric studies have demonstrated anatomical variants involving the superomedial border and the inferior pole of the scapula, which may or may not contribute to clinical symptoms (6).
Biomechanics
The scapula is a functional link that stabilizes the shoulder and allows a longer lever arm for force generation (7). Scapular movement allows the articular surface of the head of the humerus to remain relatively centered with respect to the glenoid. During abduction of the upper extremity, the scapula moves laterally for the first 30 to 50 degrees of glenohumeral joint abduction, followed by rotation about a fixed axis in abduction, resulting in approximately 65 degrees of rotation through full abduction of the shoulder (3,8).
Abnormal scapular motion can result in subacromial impingement in patients with an inability to position the acromial arch away from the humeral head. Several muscles attaching to the scapula work as force couples to stabilize the scapula during movements of the upper extremity. For proper acromial elevation, the appropriate force couples are the lower trapezius and the serratus muscles, working together, paired with the upper trapezius and rhomboid muscles (3). Nerve injuries, such as those to the spinal accessory nerve innervating the upper trapezius or long thoracic nerve supplying the serratus anterior, have been estimated to cause abnormal scapular function in less than 5% of cases (3). Consequently, the more common cause of scapular dysfunction is felt to be from muscle inhibition or weakness caused by painful conditions of the shoulder (1).
“Snapping scapula” is an unusual condition described as a “tactile-acoustic phenomenon occurring as a consequence of some anomalous condition existing between the thoracic wall and the undersurface of the scapula” (9). Friction between the scapula and the chest wall is a normal, physiological phenomenon that results from muscle action and typically is asymptomatic. The snapping scapula is associated, however, with a louder, grating or snapping sound, which can be pathologic. The underlying causes can be divided into bony and soft-tissue problems (Table 8-1). Although rare, osteochondroma is the most common scapular tumor and may
present as a mass on the deep surface that projects into the scapulothoracic space. A Sprengel deformity, which is a congenital abnormality causing a dysplastic scapula; a Lushka tubercle, which is an exostosis over the superomedial border of the scapula; and scapular or rib fracture malunion are other bony causes of a snapping scapula (9,10).
present as a mass on the deep surface that projects into the scapulothoracic space. A Sprengel deformity, which is a congenital abnormality causing a dysplastic scapula; a Lushka tubercle, which is an exostosis over the superomedial border of the scapula; and scapular or rib fracture malunion are other bony causes of a snapping scapula (9,10).
Table 8-1 Reported Causes of Snapping Scapula Syndrome | |
|---|---|
|
Evaluation
History
The patient with a scapular problem often presents with a history of shoulder impingement or pain around the scapula. Difficulties in generating force and pain over the posterior aspect of the shoulder are common complaints among throwing athletes. Previous history of shoulder or neck problems should be clarified to identify potential underlying structural or nerve pathologies. Some individuals may report crepitus around the back of the shoulder. Scapular sounds occur in from 8% to 70% of the normal population (10) and do not always represent symptomatic pathology. The intensity of the sound does not parallel the severity of symptoms, nor does it suggest a specific underlying cause (11).
Physical Examination
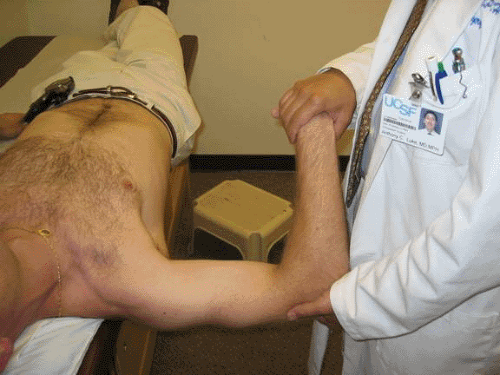
A postural evaluation should examine for cervical hyperlordosis, thoracic kyphosis, or scoliosis. Signs of atrophy should be noted in the trapezius, supraspinatus, infraspinatus, and inferior trapezius areas, suggesting either a peripheral nerve injury or disuse—in turn suggesting a chronic problem. Scapular motion can be observed for asymmetry by having the patient perform repeated flexion of the shoulder (e.g., 10 times), because abnormalities may not appear until the patient’s muscles fatigue. Tightness of the posterior capsule may be suggested by decreased internal rotation of the affected arm with the shoulder at 90 degrees of flexion and the elbow flexed to 90 degrees, similar to the Hawkin test but in abduction (Fig 8-2). Wall push-ups can be used to assess for weakness of the serratus anterior, which is demonstrated by elevation of the inferior and/or medial border of the scapula. Kibler (3) has suggested three scapular tests. The scapular assistance test involves manually stabilizing the inferior scapula and elevating it as the arm is flexed. The scapular retraction test involves manual stabilization of the medial border of the scapula with flexion of the arm. A decrease in impingement symptoms is considered to be a positive in both tests. The lateral scapular slide test assesses any asymmetrical differences in distances from the spine to the medial border of the scapula in three positions: the hands at the side, the hands on the hips, and the arms abducted at or below 90 degrees with glenohumeral internal rotation. A difference of 1.5 cm between measurements suggests weakness with scapular retraction and most commonly is seen during testing with the patient’s arms abducted (3). Pseudo-winging represents a scapular prominence that is forced out by a deep surface lesion characterized by a palpable mass, scapular grating, prominence at rest, and presence of normal scapulohumeral rhythm (12).
Imaging
Radiographs of the scapula and chest wall may demonstrate bony abnormalities of the scapula, such as osteochondroma growth from the scapula or the ribs or previous scapular fracture malunion (13). Osteochondromata can be difficult to see on anteroposterior (AP) radiographs. A tangential scapulolateral view or computed tomographic (CT) scan often is needed to demonstrate the bony lesion. Magnetic resonance imaging (MRI) is the preferred test to evaluate for a soft-tissue mass, such as an elastofibroma, or to identify scapular bursitis, although it may not necessarily demonstrate pathology in all cases.
Additional Studies
Electromyography (EMG) can be considered 3 months after the injury to rule out injuries, particularly to the spinal accessory nerve and the long thoracic nerve. Follow-up EMGs should be performed at 6- to 12-week intervals to assess for improvements if changes in denervation are observed (13).
Management
Nonoperative Management
Management of scapulothoracic dysfunction involves addressing, if possible, the underlying problem, whether that problem is an internal derangement of the shoulder, glenohumeral joint instability, rotator cuff tendinopathy, or scapular lesion. Restoration of muscle activation patterns is the next step to recover normal, asymptomatic movement. Postural exercises are important to re-establish proper, stable positioning of the scapula for better glenohumeral joint movement. Rehabilitation exercises often focus on improving shoulder range of
motion and muscular flexibility and on strengthening the scapular stabilizers, especially the serratus anterior, rhomboids, levator scapulae, and all three portions of the trapezius muscles (2,14).
motion and muscular flexibility and on strengthening the scapular stabilizers, especially the serratus anterior, rhomboids, levator scapulae, and all three portions of the trapezius muscles (2,14).
Adjuncts for treatment include nonsteroidal anti-inflammatory medications and injection therapy, mainly when symptoms of pain are affecting rehabilitation. A local injection of a long-acting anesthetic and a corticosteroid into the area of maximal tenderness (i.e., the bursa) can be helpful, but care must be taken to stay in the proper plane to avoid the risk of pneumothorax. Extension, internal rotation, and adduction of the shoulder, similar to the lift-off test position (15), can elevate the scapula to facilitate injection at the superomedial angle of the scapula. Placing the arm into abduction to 60 degrees and forward flexion to 30 degrees may assist with injection of the inferomedial scapular bursa. A figure-eight bandage may help to remind patients to maintain proper posture. Taping the scapula from the proximal aspect of the clavicle over the upper trapezius toward the thoracic spine in the orientation of the lower trapezius muscle is a common adjunct in rehabilitation. In normal patients, no changes in EMG activity have occurred with taping (16); however, taping may provide benefits for patients with abnormal shoulder function. A new tool in the armamentarium of proprioceptive rehabilitation of scapulothoracic function is the “Alignmed S3” brace, and although scientific studies are lacking, early clinical experience with this brace by the senior author and other clinicians is promising for relieving symptoms and improving scapulothoracic function.
Operative Management
Snapping scapula and painful scapulothoracic problems can be managed surgically by decompressing this articulation through removal of the documented bony prominences into the scapulothoracic space from the scapula or ribs and excision of thickened bursa. Bony resection of the medial scapular border, particularly the superomedial scapular border, even without definitively identified bony deformity, has been recommended (6,13). Although these procedures have been commonly performed as open procedures with good success (17), anatomical feasibility studies and subsequent clinical success has been reported with endoscopic surgical decompression of bony prominences in patients with snapping scapula syndrome (18,19). Galinat (18) reported 66% good to excellent results in six patients with 2-year follow-up who were treated with excision of a 3-cm triangle of bone from the superomedial angle of the scapula after failing nonoperative treatment. Recently, Ciullo (20) used isolated endoscopic resection of bursal adhesions, a more conservative approach, in those with subscapular snapping scapula syndrome with good success.
Return to Play
The literature is lacking when it comes to scientific evidence for return-to-play criteria for athletes with scapular problems who have been treated conservatively or operatively. Thus, athletes may return to play on an individual basis. Most clinicians suggest that if symptoms are mild enough, athletes can continue participation in their sport and be released to play. If the pain is persistent, clinical signs of soft-tissue injury are observed, and/or the athlete is ineffective in performing his or her activity, then consider withdrawal from play—or at least modification of his or her training until adequate treatment can be done and symptoms improve.
Scapular winging, like “scapular dyskinesis,” describes dysfunction of the scapula, usually as a consequence of nerve injury causing weakness or paralysis to one of the scapular muscles. The most common cause of neurogenic winging is injury to the long thoracic nerve, resulting in paralysis of the serratus anterior muscle. Other causes of winging are injury to the spinal accessory nerve, causing trapezius nerve palsy, and damage to the dorsal scapular nerve, causing rhomboideus palsy.
Basic Science
Anatomy
The long thoracic nerve is formed by the C5, C6, and C7 nerves distal to the scalene muscles (Fig 8-2). The long thoracic nerve is approximately 22 to 24 cm in length (21,22). The nerve passes under the brachial plexus, below the clavicle, and under the first or second rib. The nerve runs along the chest wall in the midaxillary line to the outer border of the serratus anterior, where it sends branches to each of serratus anterior muscular digitations.
The serratus anterior is the primary upward rotator of the scapular during abduction of the arm, and it stabilizes the shoulder during scapular protraction. The muscle arises from the first through ninth ribs, and it inserts onto the costomedial border of the scapula. The upper fibers of the serratus anterior insert onto the superior angle of the scapula and stabilize the scapula during the initial stages of abduction, whereas the middle fibers insert onto the vertebral border of the scapula. The lower fibers of the serratus anterior insert onto the inferior angle of the scapula.
The spinal accessory nerve is the 11th cranial nerve and provides the motor innervation to the trapezius muscle (23). The nerve passes from the base of the skull via the jugular foramen into the upper third of the sternocleidomastoid muscle. The nerve then travels subcutaneously, along the floor of the posterior cervical triangle, to innervate the trapezius muscle, which is a large, flat muscle that is divided into the upper, middle, and lower groups of muscle fibers. The upper fibers work to elevate and rotate the scapula, the middle fibers function in retracting and stabilizing the shoulder blade, and the lower fibers depress and rotate the scapula downward (24). Therefore, the trapezius muscle has important roles in the proper function of the shoulder, including abducting the
shoulder, stabilizing and rotating the scapula during overhead activities, and preventing drooping of the shoulder (25).
shoulder, stabilizing and rotating the scapula during overhead activities, and preventing drooping of the shoulder (25).
The dorsal scapular nerve originates from the C5 nerve root. This nerve travels deep into or, in some cases, through the levator scapulae to supply the rhomboid muscles (13).
Biomechanics
Blunt trauma and repetitive microtrauma from nerve traction or compression are the common mechanisms causing neurogenic winging encountered in athletes. The long thoracic nerve is vulnerable to direct injury because of its subcutaneous location, because it exits the pectoralis muscle at the fourth or fifth ribs and travels along the rib cage (26). Also, repeated tilting and lateral rotation of the head away from the affected extremity with the arm raised overhead, such as during the serving motion in tennis, may cause stretching of the long thoracic nerve (27). This nerve has several points of fixation, including the scalene medius muscle and the superior aspect of the serratus anterior, which can result in traction to the nerve with certain repetitive movements and possible vascular intimal injury (22). Areas of potential compression include the scalene muscles (medius and posterior), the first rib, between the clavicle and the second rib, between the second rib and the coracoid, the inferior angle of scapula, or inflamed bursae along the course of the long thoracic nerve (13,21,22,28). Traction over a fascial band from the inferior aspect of the brachial plexus extending to the proximal aspect of the serratus anterior has been postulated as another potential cause, because in cadavers, the nerve has been shown to bowstring over this band with the arm in abduction and external rotation, accentuated by proximal and medial migration of the scapula (29). Poor epineural blood supply may make the nerve susceptible to damage from repeated traction and compression (22).
Open injury to the long thoracic nerve is unusual without penetrating trauma or a complication of surgical procedures in the axillary region (e.g., surgery for breast cancer or to relieve thoracic outlet compression) (30,31,32).
Other reported causes of nerve injury include viral illnesses and immunizations, but the pathology is not clearly understood (21). Horwitz (28) suggested that a viral etiology might affect the multiple bursae noted along the course of the nerve, resulting in transient nerve injury that usually disappears spontaneously. Brachial neuritis or neuralgic myotrophy, also known as Parsonage–Turner syndrome, is a condition affecting the brachial plexus. The exact etiology is still unknown, but an autoimmune cause is suspected. Tsairis et al. (33) found that 25 of 99 patients affected with brachial neuritis reported a history of antecedent or concurrent upper respiratory tract infection or flulike symptoms.
Because of its subcutaneous location in the neck, the spinal accessory nerve is mainly damaged. In sports, this can occur with blunt trauma (e.g., contact with a hockey or lacrosse stick) (34). Otherwise, penetrating trauma, such as a stab wound or ballistic injury, is needed to injure the nerve. Injury to this nerve has been a reported complication following surgical procedures including radical neck dissection for tumor, carotid endarterectomy, excision of subcutaneous mass or cyst, or cervical lymph node biopsy.
Seddon (35) introduced a classification for peripheral nerve injury that has been applied to injuries to the brachial plexus by Clancy et al. (36). Neurapraxia involves a reversible axonal dysfunction with focal demyelinization following minor injury. The axon continuity is preserved, and the nerve does not undergo distal degeneration (37). Typically, this is seen in compression nerve injuries, and it most likely represents the majority of burners and stingers. Axonotmesis has more variable recovery, because there loss of continuity of axons and damage to the tissue elements of the nerve occur (37). Finally, neurotmesis involves “physiologic disruption of the entire nerve” (37). Wallerian degeneration results from deterioration of myelin, and axons become disorganized distal to the point of injury. With denervation, the associated muscle atrophy reaches a relatively stable state at 60% to 80% weight loss by approximately 4 months (37). Ideally, function can improve if reinnervation of the motor end plates can be achieved within approximately 12 months of denervation; earlier reinnervation has better outcomes (37).
Evaluation
History
Athletes with a long thoracic nerve injury often complain of pain or discomfort about the shoulder, neck, and/or scapular area. Most often, athletes will complain of an insidious onset of weakness. They may present with shoulder impingement symptoms or pain around the scapula. Overhead activity usually is difficult, and they may demonstrate weakness with forward elevation and overhead motions. Especially early in the process, the pain may not be severe enough to stop sports. Athletes may note a loss of serving speed or power. Affected athletes may be involved in a sport requiring repetitive use of the upper extremity, or they may describe blunt trauma and traction on the neck or shoulder or landing on their side with the arm outstretched. Isolated serratus anterior paralysis may result from direct injury or after carrying objects on the shoulder without any significant injury. Traction injury to the long thoracic nerve has been identified in tennis as well as other sports, including volleyball, archery, golf, gymnastics, bowling, weight lifting, soccer, hockey, and riflery.
Athletes with injury to the spinal accessory nerve similarly complain of disabling pain, weakness, and deformity. These athletes also cite the inability to fully elevate or abduct their upper extremity overhead. Weakness is noted with forward elevation, particularly above the shoulder level. Drooping of the shoulder and loss of normal shoulder function also can result in painful symptoms of shoulder impingement.
Physical Examination
On physical examination, decreased active forward elevation and loss of power/strength often are noted (56). On examination from behind, the subject will have winging, especially
of the inferior border and particularly with forward elevation and/or wall push-ups (Fig 8-3). The subject also may have uncoordinated scapulohumeral rhythm. A thin or muscular subject may have wasting or atrophy of the serratus anterior.
of the inferior border and particularly with forward elevation and/or wall push-ups (Fig 8-3). The subject also may have uncoordinated scapulohumeral rhythm. A thin or muscular subject may have wasting or atrophy of the serratus anterior.
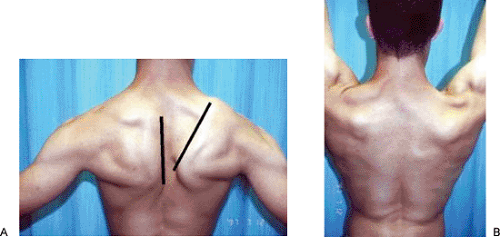
Injury to the spinal accessory nerve [cranial nerve (CN) XI] should be ruled out, because it also can produce scapular winging clinically, asymmetry of the neckline, winging of the scapula, and weakness in abduction as a result of the resultant paralysis of the trapezius. The trapezius will have weakness and atrophy, and the sternocleidomastoid also can be involved. Typically, the patient has difficulty abducting the extremity above the horizontal plane and often is unable to shrug the affected shoulder, although rested levator scapulae can produce a normal shrug test (38). Winging will involve the superomedial aspect of the scapula as it is displaced laterally, rotating both downward and outward (Fig 8-4), and will occur with the arms in abduction but not with the arms in forward elevation.
Imaging
Plain radiographs often are nondiagnostic but still should be obtained in cases of trauma and to assess for a cervical rib injury, which can be a cause of long thoracic nerve injury. Radiographs demonstrate marked inferior subluxation of the humeral head 2.5 weeks after the onset of symptoms in a patient with paralytic brachial neuritis affecting the deltoid and rotator cuff. Other imaging studies, such as CT and MRI, are not particularly helpful unless other cervical pathology is present, although the latter may demonstrate atrophy and denervation of the muscle on T2-weighted films (39).
Additional Studies
Both EMG and NCV studies are helpful to confirm the etiology of neurogenic scapular winging and to document the
severity of nerve injury. These studies can be performed as early as 3 weeks and can be repeated every 3 to 6 months to follow recovery. For spinal nerve pathology, conditions of the trapezius, sternocleidomastoid, and potentially transferable muscles (e.g., levator scapulae, rhomboideus major, and rhomboideus minor) usually are assessed.
severity of nerve injury. These studies can be performed as early as 3 weeks and can be repeated every 3 to 6 months to follow recovery. For spinal nerve pathology, conditions of the trapezius, sternocleidomastoid, and potentially transferable muscles (e.g., levator scapulae, rhomboideus major, and rhomboideus minor) usually are assessed.
Management
Nonoperative Management
Nonoperative treatment for scapular winging includes activity modification, symptomatic management, physical therapy (including maintaining shoulder range of motion and strength of compensatory muscles), and possibly, bracing. Athletes should be reassured and informed that most cases of atraumatic long thoracic nerve injury subside within 6 to 9 months (21) and that almost all cases resolve satisfactorily within 12 months (27,33,40,41). The athlete should avoid lifting heavy objects or participating in activities that exacerbate symptoms and place the nerve at risk. Nonsteroidal anti-inflammatory or other medications for neurogenic pain can be useful for control of symptoms. It should be stressed to the patient that he or she could maintain full glenohumeral range of motion. Furthermore, strengthening exercises should focus on the scapular stabilizers, particularly the trapezius, rhomboids, and levator scapulae, which will be stressed more to compensate for the dysfunctional serratus anterior. Taping commonly is used to support the scapula. Use of an orthosis has been recommended to help hold or support the scapula to the chest wall (42), but success is inconsistent. This has been reported to relieve pain, to control the stability of the scapula, and to prevent overstretching of the serratus anterior (32).
Because of the relatively good prognosis for spontaneous recovery, the mainstay of initial management is a nonoperative program. The natural history of atraumatic long thoracic nerve palsy is resolution within 1 year (43); however, cases resulting from Parsonage–Turner syndrome (brachial plexitis) may take as long as 2 to 3 years to resolve (21). Even so, it has been reported that conservative treatment will not be successful in approximately one-quarter of patients with a long thoracic nerve injury (40).
Return to Play
Return-to-play recommendations should be made on an individual basis (44). Hershman et al. (45) recommended that an athlete who has recovered a plateau in of adequate strength may be allowed to return to sports; however, if full strength has not been recovered, the athlete may need to limit his or her activities, particularly in contact sports.
Operative Management
The indications for surgery in patients with scapular winging caused by long thoracic nerve injury include penetrating trauma or persistent pain and symptoms that persist beyond 1 to 2 years despite adequate conservative treatment and failure of documented EMG improvement in nerve function. Because they are amenable to primary repair and have improved function if the repair is successful, penetrating injuries resulting in long thoracic nerve laceration should be treated with nerve exploration and, possibly, nerve repair. Options for delayed surgical repair of nerve laceration or direct injury include neurolysis and/or nerve grafting when patients show evidence of loss of nerve function (13).
Serratus anterior palsy resulting from chronic long thoracic nerve palsy traditionally has been treated surgically with muscle transfers, scapulopexy, and/or scapulothoracic fusion (46,47,48). Unfortunately, these surgical options for chronic injury to the long thoracic nerve rarely allow an athlete to return to most competitive sports that require arm strength and motion. A variety of muscles have been used as a musculotendinous transfer to control scapular winging, including the pectoralis major (49,50,51,52,53,54), pectoralis minor (55,56,57), rhomboids and teres minor (58,59,60). The senior author’s preference to use the pectoralis major as the muscle transfer for scapular winging caused by long thoracic nerve injury (61).
Recently, reports have appeared of small series or patients treated for long thoracic nerve dysfunction without using a muscle transfer or scapulothoracic fusion. Disa et al. (62) reported excellent results with supraclavicular neurolysis of the long thoracic nerve that was dysfunctional because of nerve compression within the scalene muscles. These same authors also reported excellent results in all four patients who underwent neurolysis 10 to 35 months after the onset of symptoms. Transfer of the thoracodorsal nerve or medial pectoral nerve to the long thoracic nerve has been reported to have good functional results in patients with symptomatic long thoracic nerve injury (63,64).
Brachial plexus neuropathy presents with temporary stinging, burning, or tingling that occurs when the head is forcefully bent sideways. These injuries commonly are referred to as stingers or as burners. The incidence of these injuries is uncertain, because they occur so commonly and are so familiar to athletes and coaches that most do not present for medical care. Symptoms from this syndrome typically last for seconds to minutes; however, in 5% to 10% of cases, the neurological deficit can last for hours, days, or even weeks (65,66). Controversy remains whether damage occurs at the nerve root or at the brachial plexus itself. Management typically involves symptomatic treatment, because the condition usually is self-limited. The important consideration, however, is to rule out underlying factors that may predispose the athlete to more serious, persistent injury.
Basic Science
Anatomy
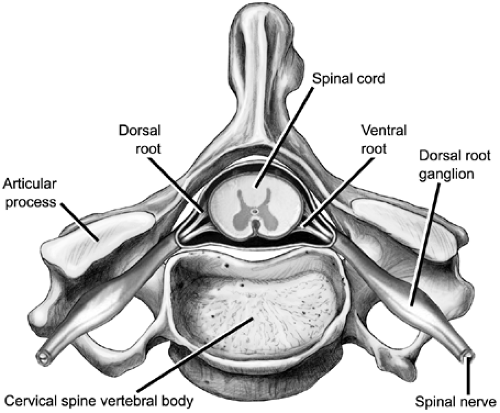
At each segmental level, the dorsal and ventral roots exit the spinal cord and join to form the cervical (or spinal) nerve root. The ventral (or anterior) roots are formed by the motor
nerve fibers leaving the anterior horns cells of the anterior gray area of the spinal cord, whereas the dorsal roots consist of the cell bodies of the sensory fibers. The cervical nerve root enters the neuroforamen, where it forms the dorsal root ganglion (67) (Fig 8-5). Distal to the foramen, the cervical root then divides into a posterior primary ramus, which innervates the paraspinal muscles, posterior elements of the spine and overlying skin, and anterior primary ramus. Several nerves come off the spinal nerves as small branches, such as the dorsal scapular nerve (from the C5 spinal nerve), the long thoracic nerve (C5–C7), and the phrenic nerve (C3–C5). The cervical roots then form the brachial plexus, which supplies motor function and sensation to the upper extremities.
nerve fibers leaving the anterior horns cells of the anterior gray area of the spinal cord, whereas the dorsal roots consist of the cell bodies of the sensory fibers. The cervical nerve root enters the neuroforamen, where it forms the dorsal root ganglion (67) (Fig 8-5). Distal to the foramen, the cervical root then divides into a posterior primary ramus, which innervates the paraspinal muscles, posterior elements of the spine and overlying skin, and anterior primary ramus. Several nerves come off the spinal nerves as small branches, such as the dorsal scapular nerve (from the C5 spinal nerve), the long thoracic nerve (C5–C7), and the phrenic nerve (C3–C5). The cervical roots then form the brachial plexus, which supplies motor function and sensation to the upper extremities.
The cervical nerve roots are more susceptible to injury as a result of traction injury compared with the brachial plexus. The cervical roots do not have the protective epineurium, perineurium, fascicular structure, and fascicular plexiform arrangement that protects the brachial plexus from stretch and compression (68). The plexiform structure of the brachial plexus, with its compliant, surrounding soft-tissue structures, can tolerate a greater amount of tension compared with the cervical nerve roots (69), which pass through bony, rigid canals that can be narrowed by anatomical factors.
Biomechanics
Three main mechanisms have been described that may result in a burner or stinger: (a) nerve compression, (b) nerve traction, or (c) a direct blow to the brachial plexus, resulting in upper trunk or cervical root symptoms, particularly involving C5 and C6. Lower cervical roots are less susceptible to damage, but injury can occur with the shoulder either abducted or fully extended. Controversy remains regarding whether a burner is primarily a brachial plexus or a cervical root injury, a situation that is compounded by the lack of clear demarcation about where the cervical nerve root ends and the brachial plexus begins. Permanent nerve damage can result from recurrent brachial plexus injuries.
Narrowing of the intervertebral foramen occurs with neck extension and with lateral bending, especially when the two motions are combined (70). The narrowing is most pronounced at the C4–C5 and C5–C6 levels. Published series suggest that the extension–lateral compression mechanism is predominately the cause of burners (83% to 85% of cases) (71,72,73). It appears that compression injuries occur in adult populations, whereas traction injuries are more common in children. Burners associated with these mechanisms are seen in athletes with pre-existing (though may be asymptomatic) cervical spine pathology, such as cervical disc disease or degenerative change.
A second mechanism of a burner is nerve traction as the shoulder is depressed and the nerves are fixed proximally. The traction forces are transmitted to the upper trunk of the brachial plexus, especially the upper cervical nerve roots (C5–C6), stretching and injuring these structures (74,75,76). The shoulder can be driven downward, and the head and neck in the opposite direction, while blocking or tackling in football or while landing on the shoulder in wrestling, the second most common sport in which this injury occurs (77). This is suggested to be the most frequent mechanism in younger athletes without cervical stenosis or arthritic change (36,76,77).
Finally, the third mechanism is a direct blow to the Erb point, which lies superior and deep to the medial clavicle, just lateral to the sternocleidomastoid muscle (25). In football, the upper trunk of the brachial plexus can be compressed between the shoulder pad and the superior medial scapula following direct trauma (78,79).
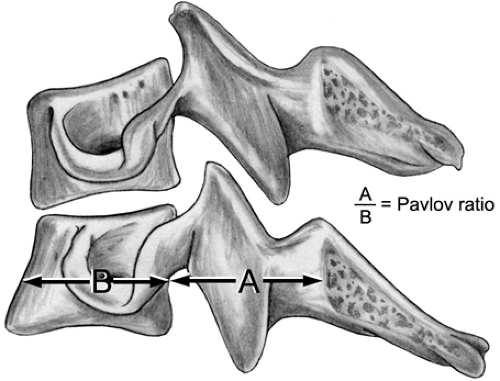
Athletes with recurrent cervical nerve root neurapraxia were found to have disc disease and narrowing of the intervertebral foramen in 93% of cases (71). Several papers have identified an association between the incidence of burners and developmentally narrowed spinal canals. In two series, 47% (72) and 53% (71) of athletes had a Pavlov ratio of less than 0.8, and a significant difference was found between measurements among individuals with a previous history of a burner and controls (80) (Fig 8-6).
Evaluation
History
The athlete with a burner usually complains of a traumatic episode with transient numbness, weakness, and/or electrical pain that shoots down the arm to the hand and that lasts for seconds to minutes. Complaints are almost always unilateral, and the athlete rarely complains of neck pain. It most commonly occurs following blocking or tackling; thus, it more commonly affects those athletes participating in
American football who play as a defensive back, linebacker, and/or lineman (81). Up to 65% of collegiate football players are noted as having had a burner or stinger during their 4-year college career (36,77,79).
American football who play as a defensive back, linebacker, and/or lineman (81). Up to 65% of collegiate football players are noted as having had a burner or stinger during their 4-year college career (36,77,79).
Physical Examination
The athlete with a burner may come off the field shaking his or her arm and hand. If significant neck pain exists, or when neurological symptoms involve two or more extremities, cervical spine precautions should be taken with the athlete until the player is cleared from having a cervical spine injury. A typical examination of a burner includes observation and palpation of the neck region for tenderness, swelling, or deformity. The athlete may hold the neck flexed to alleviate pressure on the cervical root. Palpation around the affected nerve root may cause local pain and aggravate symptoms. The shoulder, clavicle, sternoclavicular, and acromioclavicular joints also should be evaluated for deformity and swelling to rule out any other injury. The range of motion in the neck should be assessed by observing active movement through full motion, including flexion, extension, lateral bending, and rotation. If the range of motion is not significantly restricted and little apprehension is noted with movement of the neck, a Spurling maneuver may be performed by gently, laterally bending and extending the head with mild downward pressure (82). A positive sign is reproduction of symptoms down the arm. In cases of traction injury, lateral bending of the neck away from the symptomatic side may cause stretching of the brachial plexus, reproducing symptoms. A careful examination of sensation and motor strength should be performed on the upper extremities. The most common pattern of symptoms is over the lateral aspect of the arm, along the radial nerve distribution (C5–C6). Special attention should be taken to assess upper trunk function (deltoid, rotator cuff, and biceps) to evaluate the burner and recovery from the injury and to assess the lower trunk (ulnar nerve) to rule out other significant injuries that may be masquerading as a burner. A Tinel sign may be elicited by tapping in the region of the Erb point (superior and deep to the medial clavicle, just lateral to the sternocleidomastoid muscle). With a mild injury, symptoms often resolve quickly (within minutes).
Imaging
For any significant neck injury, radiography of the cervical spine should be performed, including AP, lateral, bilateral oblique, lateral flexion, and extension views. Imaging may be deferred in cases of recurrent burners in which symptoms resolve, but radiography should be considered for any athlete with first-time symptoms. Radiographs should be evaluated for loss of cervical lordosis, spinal stenosis, foraminal stenosis, and instability. Meyer et al. (72) and Kelly et al. (80) have reported that players with a Pavlov ratio of less than 0.8 have an increased risk of experiencing a burner. It should be noted that although athletes with a Pavlov ratio of less than 0.80 demonstrate a higher risk of recurrent stingers, but not of first-time stingers, the level of stenosis did not correlate with the level of stinger symptoms (83).
Magnetic resonance imaging can be helpful in identifying nerve root injuries. In one series, 11 patients with MRIs demonstrating root avulsion had the diagnosis confirmed during surgery, with no false positives (84). Edema in the spinal cord was suggestive of root avulsion. The sensitivity of MRI to detect nerve root avulsions has been reported to be from 81% to 92.9% (84,85). Also, MRI can rule out structural pathologies (86), such as herniated discs, ligamentous injuries, facet injuries, and nondisplaced fractures. Magnetic resonance neurography remains investigational, however, and its role in brachial plexus problems is still being evaluated (87).
Additional Studies
Electrodiagnostic studies can be useful in localizing the site of nerve injury and in quantifying the degree of neurological damage (88). However, EMG and nerve conduction studies are considered only with prolonged neurological symptoms. Continued muscular weakness at 72 hours has been shown to correlate with positive electrodiagnostic testing at 4 weeks (66). EMG may not demonstrate accurate changes until at least 14 days (86). Thus, electrodiagnostic studies have not been helpful in making return-to-play decisions; cases have been reported in which the EMG remained abnormal for more than 4 years after the injury even after full clinical recovery (66,89).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree