6 The thoracic spine
CHAPTER CONTENTS
Introduction
The spinal column forms the keel of the human body, and is exposed to a variety of metabolic, mechanical, and circulatory stresses that contribute to pain. The thoracic spine (T-spine) receives relatively little attention compared with its cervical and lumbar neighbours; this may be attributed to difficulties associated with movement analysis or the belief is that it is less commonly implicated in clinical pain syndromes (Edmonson & Singer 1997). However, within clinical practice the T-spine is frequently found to be a source of musculoskeletal dysfunction. The clinical syndrome of whiplash injury includes neck and upper thoracic pain, as well as cervicogenic headaches (Hong & Simonds 1993), together with more subtle presentations of chest, viscerosomatic, and somatovisceral pain patterns. However, much of the clinical theory, particularly in relation to the influences on spinal posture and movement, is untested (Edmonson & Singer 1997), and equally no consensus on interventions has been established. In comparison to the cervical or lumbar spine, there have been few studies on the effect of manipulation and mobilization techniques for the upper body (Atchinson 2000). An understanding of skeletal, facial, and muscular innervation of the T-spine is essential for effective management of pain and dysfunction.
Skeletal structures
T1 to T8
The T1 toT8 vertebrae are classified as typical vertebrae, the compressive load on T1 being about 9% of body weight increasing to 33% at T8 and 47% at T12 (White 1969). The vertebrae articulate with corresponding ribs and costovertebral joints, the upper three to four nerve roots supplying the medial arm and axilla via the brachial plexus. The T2 vertebra ascends to the mid-dorsal level and acromion; it may well influence shoulder pain and dysfunction (Hoppenfield 1977). The costovertebral synovial joints are rich in proprioceptive innervation and are often a source of costovertebral dysfunction with presentation of pain. The T5 to T8 vertebrae are relatively immobile, providing greater stability, together with the thoracic cage, against anterior flexion, facilitating rotation at approximately 10° between T5 and T8. Posterior extension is limited by the shape of the zygapophysial facets and spinous processes (Mootz & Talmage 1999) (Table 6.1).
Table 6.1 Thoracic range of movement guideline
| Movement | Measurement | Vertebral level |
|---|---|---|
| Flexion | 23° | T1 to T12 |
| Extension | 10° | C7 to T12 |
| Lateral flexion | 20° to 40° | C7 to T12 |
| Rotation | 20° | T1 to T12 |
| Costovertebral expansion excursion | Inhalation: 6.5 mm Exhalation:13 mm | T8 to T10 |
Adapted from Evans (1994).
T9 to T12
The extent to which features of spinal degeneration and pathoanatomy are related to symptoms remains unclear, and the influence of motion segmental degeneration on the mobility of the thoracic spine has not been established (Edmonson & Singer 1997). Thoracic disc herniations are uncommon lesions that are asymptomatic in most patients (Sheikh et al 2008), and unless affected by Scheurmann’s disease, any increased kyphosis in adolescent individuals may be attributed to poor habitual posture rather than structural changes or reduced joint mobility. As the thoracic kyphosis increases with age the associated anatomical changes and decreased mobility will only be ameliorated by compensatory changes in the lumbar and cervical regions and the shoulder girdle (Edmonson & Singer 1997).
Careful observation during active movement testing is required, and thus, any upper thoracic symptoms should include an assessment of the cervical and cervicothoracic junction. Mechanical provocation should include resisted, assisted, active, and passive movements, as well as ischaemic compression (Mootz & Talmage 1999). The sensitivity and specificity of many physical examination processes for recording thoracic range of motion (ROM) are limited (Deyo et al 1992), and these should be contextualized within the overarching results of careful questioning and examination of all structures. Palpation for tenderness is a crucial part of manual therapy assessment for musculoskeletal dysfunction. Mid-thoracic tenderness is not a normal finding in asymptomatic subjects, and as such, it should be viewed as a possible source of pain-presenting structures (Keating et al 2001).
Joint movement assessment
Palpation helps determine the range and quality of motion of individual joints but pure passive movement is difficult to determine at the T-spine (Mootz & Talmage 1999). There are four essential categories of joint play (Maitland 1986):
Reliability studies on motion palpation and joint play have shown much variability (Haas et al 1995), as have discussions about the direct application of manual forces to affect the underlying thoracic joint and restore function (Bereznick et al 2002; Hertzog et al 1993). Generally, direct manipulation techniques are employed in the presence of somatic impairment when tissue reactivity is low, tissue stiffness is dominant, and minimum pain at the end of available range is demonstrated (Maitland 1986). In contrast, indirect or positional release techniques are applied to soft tissues and joints in the presence of somatic impairment when this is associated with high levels of tissue reactivity with associated nociceptive hypertonicity (Chaitow et al 2002).
Pain arising from the thoracolumbar joints may be referred (via the terminal branches of the dorsal rami) into the lower lumbar spine, buttocks, and inguinal area (Dreyfuss et al 1994; Grieve 1988). Careful spinal mobilization and manipulative techniques may be implicated in this area, but only with evidence of the absence of any underlying pathology or neurological involvement. Sustained neural apophyseal glides (SNAGs) (Mulligan 1995) are important in the context of painful movement dysfunction associated with degenerative change (Edmonson & Singer 1997), providing normal physiological load-bearing, and combining elements of active and passive physiological movement with accessory glides along the zygapophysial joint plane (Edmonson & Singer 1997; Mulligan 1995). The Mulligan (1995) concept encompasses a number of mobilizing treatment techniques that can be applied to the spine, including natural apophyseal glides (NAGs), SNAGs, and spinal mobilizations with limb movements (SMWLMs).
Thoracolumbar fascia
The thoracolumbar fascia (TLF) is a critical structure in transferring load from the trunk to the lower extremities (Vleeming et al 1995). The anatomy of the TLF is complex, providing attachment for numerous paraspinal and abdominal muscles, as well as stability to the pelvic girdle when movement of the upper and lower extremities is undertaken. Muscle control in posture and locomotion is reliant on multifactorial integrated systems, the quality of muscle function depending directly on central nervous system (CNS) activity (Janda 1986). Functional stability is dependent on integrated local and global muscle function. Mechanical stability results from segmental (articular) and multisegmental (myofascial) function. Any dysfunction presents as a combination of restriction of normal motion and associated compensations (i.e. give) to maintain function (Comerford & Mottram 2001). Strategies to manage mechanical stability dysfunction require:
Stability re-training targets both the local and global stability systems; the strategy is to:
Biopsychosocial influences
Emotional states have a huge impact on basic muscle tone and patterning, influencing muscle and visceral tone both locally and globally (Holstege et al 1996). Even more pertinent to physical intervention is the existence of the sympathetic chain, which is routed along the length of the T-spine and has ganglia in close proximity to the head of each rib. The result is that abdominal and visceral pain may refer to various thoracic levels, and these need to be assessed together with joint structures.
Autonomic nervous system
Sympathetic fibres leave the spinal nerve from levels T1 to L2 to join the sympathetic chain via the white rami communicantes. They travel for up to six T-spinal segments before synapsing with between 4 and 20 postganglionic neurons. The postganglionic neurons exit via the grey rami communicantes to rejoin a peripheral nerve and are distributed to the target tissues (Evans 1997). These nerves supply vasoconstrictor fibres to arterioles, secretory fibres to sweat glands, and pilomotor fibres to the skin (Craven 2008). The head and neck are supplied by levels T1 to T4 and the upper trunk and upper limb by T1 to T9 (Bogduk 2002). The paired sympathetic trunk consists of ganglia and nerve fibres, and extends along the prevertebral fascia from the base of the skull to the coccyx (Craven 2008). There are two complementary parts of the autonomic nervous system (ANS); the sympathetic nervous system (SNS), which controls excitatory fight or flight reflexes, and the parasympathetic nervous system (PNS), which controls inhibitory rest and repose reactions. These two complementary, but contrasting and contradictory, systems leave the CNS at different sites, and have opposing effects through adrenergic or cholinergic endings.
Visceral fibres pass to the thoracic viscera by postganglionic fibres to:
The greater splanchnic nerve (T5 to T10) ends in the coeliac plexus, while the lesser one (T9 to T10/T11) ends in the aortic and renal plexus. The lumbar sympathetic trunk (L1 to L5) supplies the pelvic viscera, rectum, bladder, and genitalia via the hypogastric nerves, whilst the inferior plexus (S2 to S4) receives parasympathetic branches from the nervi erigentes (Craven 2008).
The parasympathetic nervous system
The PNS is comprised of cranial and sacral components that cause constriction of the pupils, decreases in heart rate and volume, bronchoconstriction, increase in peristalsis, sphincter relaxation, and glandular secretion, whilst the pelvic component inhibits the detrusor muscle of the bladder (Craven 2008).
The cranial outflow is conveyed to the oculomotor nerve (III), facial nerve (VII), glossopharyngeal nerve (1X), and vagal nerves (X). Knowledge of the neural innervation and response of the PNS and SNS is essential for any proposed manual intervention. The insidious nature of thoracic pain and the associated postural dysfunction and stress (DeFranca & Levine 1995) may predispose the ganglion to mechanical pressure (Bogduk 1986), ischaemia (Conroy & Schneiders 2005), and somatic dysfunction via the CNS (Shaclock 1999).
Central pain mechanisms are deeply embodied in the psychophysical problem of pain, and are becoming increasingly recognized as playing a major role in the generation and maintenance of pain and disability associated with neuromusculoskeletal problems. Central mechanisms participate in all pain states, both acute and chronic. They are universally influenced by psychological and physical factors, whether or not a specific pathology can be identified. Common misconceptions that arise are that manual therapy operates on peripheral mechanisms without influencing the central ones and that, when a central problem exists, psychological management is preferable. In reality, as key players in the healing process, central mechanisms are profoundly affected by manual therapy even when it is directed at a peripheral problem. Treatment of peripheral mechanisms can be performed through central techniques because both peripheral and central mechanisms are always part of the same clinical problem. Consequently, manual therapy must integrate central mechanisms into clinical practice as a means of improving therapeutic efficacy and to prevent the descent of acute pain into chronic pain. Hendler (2002) suggested that 25–75% of cases of misdiagnosed complex regional pain syndrome type I (CRPS1) are actually upper extremity nerve entrapment affected more often by the scalenes and pectoralis minor muscles. Given the mounting evidence that chronic muscle pain syndromes may be sympathetically driven or maintained, it may be pertinent that chronic thoracic pain should be approached from the hypothetical perspective of muscle spindles under constant sympathetic excitation, meaning that the term ‘sympathetic intrafusal tension syndrome’ should replace myofascial pain syndrome as the appropriate description (Berkoff 2005) (Table 6.2).
Table 6.2 Common features and associated disorders of sympathetic intrafusal tension syndrome (SITS)
| Presenting symptomsa | Associated symptomsa |
|---|---|
| Constant stiffness/discomfort at C7 area | Sleep disturbance |
| Constant stretching, rubbing, or pressure of pain area | Bruxism and temporo-mandibular joint pain |
| Active TrPts in scapular muscles reproduce pain pattern | Pain increased with stress |
| Gradual chronic pain fluctuations with no acute attacks | Worse on waking and end of day |
a Clinical diagnosis of SITS may be made on the presence of:
Adapted from Berkoff (2005).
Uncovering stressful condition-stimuli and evaluating their potential clinical relevance is vital. Relaxation, breathing, biofeedback, and cognitive behaviour therapy techniques are all useful in the management of increased sympathetic sensitivity. Here, the management of physical measures to alleviate pain and discomfort must be integrated in a multidisciplinary manual and biopsychosocial approach; a purely biomedical approach to physical therapy is too reductionist. Therapy needs to shift from symptomatic treatment to an emphasis on education, rehabilitation, facilitation of ownership, personal responsibility, and continuing management (CSAG 1994), in order to achieve longer lasting results and restoration of function.
The onset of acute chest pain, which may be very distressing for patient and family, is a major health problem in the Western world, and the most common reason for hospital admissions (McCaig & Nawar 2004). In over 50% of cases, the aetiology appears to be non-cardiac (Chambers et al 1999; Eslick et al 2001) and often no definitive diagnosis can be made (Panju et al 1996). Many thoracic dysfunctions have a mechanical cause originating from the T-spine, and referring to the upper extremities, chest, and cervical and lumbar spine, together with reverse referral patterns (Lee 2003; Proctor et al 1985; Wickes 1980).
The heart, pleura, and oesophagus are all potential generators of visceral pain in the T-spine. Sensory fibres from cardiac and pulmonary structures are routed through T1 to T4 and T5. Irritable bowel syndrome (IBS) is accompanied by altered visceral perception and back pain (Accarino et al 1995; Zighelboim et al 1995), and patients often demonstrate visceral and cutaneous hyperalgesia via viscerosomatic neurons (Tattersal et al 2008). The overlap between fibromyalgia syndrome (FMS) and IBS is considerable, with 70% of patients with FMS reporting chronic visceral pain and 65% of those with IBS having primary FMS (Veale et al 1991).
Chronic visceral pain syndromes are more common in women than men and manifest such conditions as abdominal pain, migraine, and FMS (Table 6.3), reflecting the influence of hormonal factors on the algesic response both peripherally and centrally. The direct effect of oestrogen, progesterone, and testosterone on organ function, and psychological and social factors cannot be underestimated within the assessment process (Giamberardino 2000; Heitkemper & Jarrett 2001).
Table 6.3 Myofascial and visceral pain syndromes: viscerosomatic pain presentation
| Pain referral pattern | Visceral involvement | Physiological processing |
|---|---|---|
| Pectoralis major Pectoralis minor Scapula Forearm | Myocardial infarction | Afferent interactions Increased sympathetic reflexes Increased fluid extravasation Oedema Sympathetic hypersensitivity |
| Lumbar Groin Thigh Right upper abdominal quadrant Abdominal oblique Rectus abdominus | Urethral colic Biliary colic | |
| Lower quadrant muscle Pelvic pain and tenderness Low back Abdominal muscle wall Iliopsoas Adductors Piriformis Pelvic floor Right shoulder Rotator cuff C5 and C6 | Ovarian/uterine pain Urethral colic Dysmenorrhoea Cystitis Chlamydia Bladder and bowel dysfunction Sexual dysfunction Vulvodynia Liver and gall bladder Phrenic nerve irritation | Increased hypersensitivity and visceral tone of bladder |
| Mediastinal Pleura Impingement syndrome Frozen shoulder | Diaphragmatic irritation Gall bladder dysfunction |
Adapted from Gerwin (2002).
Recent findings have indicated that spinal manual therapy produces concurrent hypoalgesia and sympathoexcitatory effects (Sterling et al 2001). Therefore it is pertinent that, with regard to patients exhibiting sympathetically maintained pain or increased hypersensitivity of the SNS, manual mobilization may indeed add to both hypersensitivity and pain pattern. Thus great care should be taken in both the examination of and intervention in any hypersensitive thoracic states.
Myofascial component
Myofascial interscapular pain can confuse clinicians because it can be composite pain referred from as many as 10 different muscles (Whyte-Ferguson & Gerwin 2005) (Fig. 6.1).
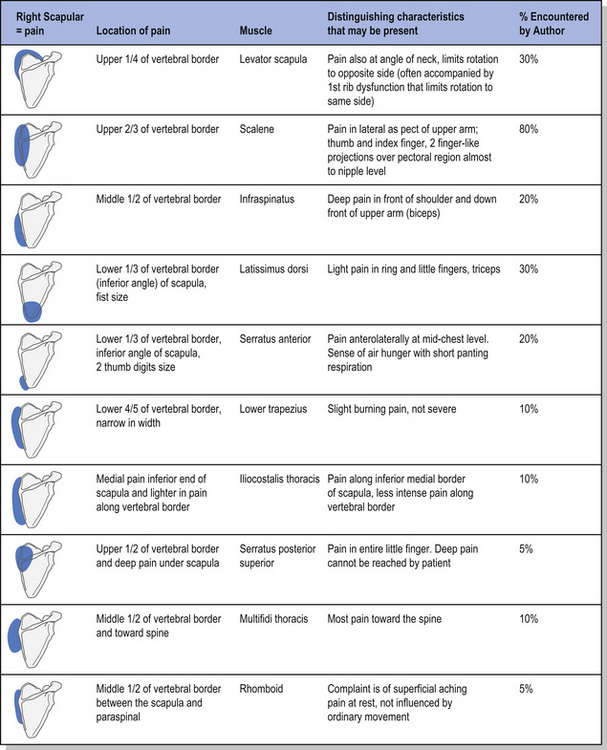
Figure 6.1 Interscapular pain table.
Reproduced with kind permission from Lucy Whyte Ferguson & Robert Gerwin (2005), Clinical Mastery in the Treatment of Myofascial Pain, Lippincott Williams and Wilkins.
One of the commonly overlooked causes of interscapular pain, one responsible for more than 80% of reported cases, is the scalene muscle complex which refers pain into three distinct areas (Spanos 2005):
The term T4 syndrome represents a clinical pattern involving upper extremity paraesthesia, and pain with or without symptoms into the neck and/or head (Maitland 1986). Even today the syndrome is poorly defined and agreed upon (Grieve 1994). Equally, it appears to be a catch-all phrase used by clinicians for patients whose varied problems seem to be derived from the upper T-spine and are not at all confined to T4 segmental vertebrae. It is not an uncommon presentation in clinical practice. Pain may be caused by a variety of structures (Evans 1997):
The sympathetic nerves supply forms a path for expression of T4 syndrome with pain referral occurring in the somatic nerves, referring from a proximal structure supplied at one level to a peripheral structure supplied at the same level (Evans 1997). Evans (1997) suggested that it might not only be the joint that is involved but also the arteriole. Sustained or extreme postures can lead to relative ischaemia, a repetitive strain injury with sympathetic symptoms, and repeated injury and repair, often seen in the more demanding upper quadrant sports such as rowing, gymnastics, and javelin, and prolonged poor posture in the workplace.
Recent findings demonstrating that cervical spinal manipulation produces concurrent hypoalgesia and sympathoexcitatory effects have led to the proposal that spinal manipulation may exert its initial effects by activating descending inhibitory pathways from the dorsal periaqueductal grey area of the midbrain, producing increased pressure-pain thresholds on the side receiving the treatment. Visual analogue scale (VAS) scores decreased along with superficial neck flexor muscle activity (Sterling et al 2001). Manual therapy may include both mobilization (low-velocity oscillatory techniques) and manipulation (high-velocity thrust techniques). Often little difference is found in reported conclusions about the effectiveness of manual therapy in using these techniques (Hurley et al 2005). Thoracic spine manipulation is applied only if extension restriction of T1 to T4 has been identified based upon palpatory examination and gliding motion of the upper thoracic dorsal vertebrae (Fernández de las Peñas et al 2004). Thoracolumbar joint manipulation should be applied in all patients with the aim of restoring free movement at T12 to L1 because the biomechanical analysis of whiplash injury implies a compression spine dysfunction at this level (Panjabi et al 1998; Yoganandan et al 2002). Inconsistencies in manual force application during spinal mobilizations in existing studies suggest that further studies are needed to improve clinical standardization of manual force application (Snodgrass et al 2006).
Determining the source of propagating pain structures is imperative and often complex for the successful resolution of thoracic pain. Manual examination of muscles, joints, fascia, and spinal dysfunction has been the subject of much criticism because of poor reproducibility and validity (Stochkendahl et al 2006). What is paramount is a clear clinical reasoning pathway in order to eliminate, select, and treat appropriate presenting pain structures for effective management and rehabilitation, to prevent the development of chronic pain syndromes.
6.1 Acupuncture interventions with thoracic spine dysfunction
Stressors are physiological or psychological perturbations that throw the body out of homeostatic balance; the stress response is the set of neural and endocrine adaptations that help us re-establish homeostasis. In traditional Chinese medicine (TCM) a balance between Yin and Yang (homeostasis) ensures both physical and mental health and well being, Acupuncture is believed to aid the restoration of homeostasis. With prolonged stress, increased corticotropin releasing factor is secreted from the hypothalamus into the hypophysial–pituitary circulation, along with a pituitary release of adrenocorticotropic hormone, which rapidly releases glucocorticoids. Glucocorticoids are central to the stress response, targeting energy storage, increasing cardiovascular tone, and inhibiting anabolic processes such as growth, reproduction, healing, inflammation, and immunity (Sapolsky 1992). The stress response now becomes as damaging as the stressor itself. Stressors disrupt physiological regulatory mechanisms, leading to diseased states and altered responses of the psychoneuroimmune system.
It has been estimated that 80% of all illness is stress-induced (Friedman et al 2003; Sapolsky 1992; Walling 2006). One purpose of any healthcare system is to diagnose and treat dysfunctions of the homeostatic mechanisms of any individual in order to maintain the higher level of health and to prevent disease. However, increasingly within the Western world, interventions are directed towards the symptoms of failure of that homeostatic system. The integrated use of acupuncture within a physiotherapeutic toolbox may offer the clinician the ability to directly affect homeostatic stability as a means of restoring health or preventing further disease. The science of neuroimmunology, when combined with the art of TCM acupuncture, may enable the endocrine and immune system to regulate a cascade of cellular processes and changes, through the stimulation of neuropeptides, via needle insertion at selected points in order to maintain, rebalance, and restore health and well being. When Yin and Yang systems are balanced, the neuropeptides are free flowing (Qi) and a sense of well being pervades (Shen). Stress prevents the free flow (Qi stagnation) of peptide-signalling molecules (Pert 1997), creating blockages (Qi excess or stagnation) and weakness (Qi deficiency) that may lead to disease. Reduced output of endorphins and norepinephrine may lead to anxiety and depression (Shen disturbance) (Pert 1997).
A continuous interaction via action potentials within the nerve fibres, which may in fact be acupuncture meridians, exists between the autonomic, central, and endocrine systems. Action potentials are generated in response to a stimulus, whether physical or emotional, positive or negative, and thus, pathological over- or underactivity of neurotransmitters may cause neurological or psychiatric disease (Pert 1997; Sapolsky 1992
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree











