18 The thigh and knee
The knee depends for its stability upon its four main ligaments and upon the quadriceps muscle. The importance of the quadriceps cannot be overemphasised. So efficiently can a powerful quadriceps control the knee that it can maintain stability despite considerable laxity of the ligaments. In many injuries and diseases of the knee the quadriceps wastes strikingly, and to some extent the condition of the muscle is an index of the state of the knee: if it is wasted it is probable that there is a significant abnormality within the joint.
The knee is, in fact, a region where nearly every kind of orthopaedic disorder may be represented.
SPECIAL POINTS IN THE INVESTIGATION OF THIGH AND KNEE COMPLAINTS
History
The history is of particular importance in the diagnosis of disorders of the knee. In a case of torn meniscus, for instance, the history is often the most important factor in the clinical diagnosis. When there has been a previous injury to the knee, the exact sequence of events at the time of the injury and afterwards must be ascertained. Enquiry is made into the mechanism of the injury; what the patient was doing at the time; whether he was able to carry on afterwards. Was he able to finish the game? If not, was he carried from the field or was he able to walk? How soon after the injury did the knee swell? Was he able to straighten the knee fully? If not, how did he eventually get it straight? Was he able to bend it? These and many other details must be elicited by careful questioning because they are so important in building up a picture of what exactly happened to the knee. Caution is necessary in accepting the patient’s story of ‘locking’ at its face value. Many patients speak of ‘locking’ when the knee simply feels stiff and painful, or when it causes momentary jabs of pain on movement. Locking from a torn meniscus means simply that the knee cannot be straightened fully; it can usually be flexed freely. In locking from a loose body within the joint the knee may be jammed so that it will neither flex nor extend, but this is rather uncommon and the knee usually unlocks itself after an interval, or can be freed by judicious manoeuvring.
Steps in clinical examination
A suggested routine for clinical examination of the thigh and knee is summarised in Table 18.1.
Table 18.1 Routine clinical examination in suspected disorders of the thigh and knee
| 1. LOCAL EXAMINATION OF THE THIGH AND KNEE | |
| Inspection | Power (tested against resistance of bone contours and alignment examiner) |
| Soft-tissue contours | Flexion |
| Colour and texture of skin | Extension |
| Scars or sinuses | |
| Palpation | Stability |
| Skin temperature | Medial ligament |
| Bone contours | Lateral ligament |
| Soft-tissue contours | Anterior cruciate ligament: anterior draw test; Lachman test; pivot shift test |
| Local tenderness | Posterior cruciate ligament |
| Measurements of thigh girth | Rotation tests (McMurray) |
| Comparative measurements at precisely the same level in each limb give an indication of the relative bulk of the thigh muscles, and in particular of the quadriceps | (Of value mainly when a torn meniscus is suspected) |
| Movements (active and passive, against normal knee for comparison) | Stance and gait |
| Flexion | |
| Extension | |
| ? Pain on movement | |
| ? Crepitation on movement | |
| 2. EXAMINATION OF POTENTIAL EXTRINSIC SOURCES OF THIGH OR KNEE SYMPTOMS | |
| 3. GENERAL EXAMINATION | |
| General survey of other parts of the body. The local symptoms may be only one manifestation of a widespread disease | |
Determining the cause of a diffuse joint swelling
A diffuse swelling of the knee can arise only from three fundamental causes:
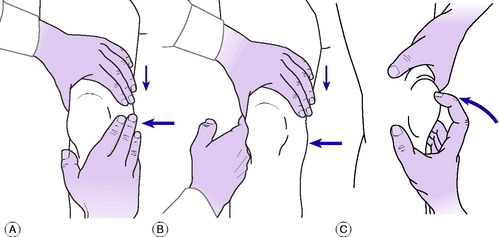
Fluid within the joint. A fluid effusion is best detected by the fluctuation test. The palm of one hand is placed upon the thigh immediately above the patella – that is, over the suprapatellar pouch. The other hand is placed over the front of the joint, with the thumb and index finger just beyond the margins of the patella (Fig. 18.1A). Pressure of the upper hand upon the suprapatellar pouch drives fluid from the pouch into the main joint cavity, where it bulges the capsule at each side of the patella and imparts an easily detectable hydraulic impulse to the finger and thumb of the lower hand (Fig. 18.1B). Conversely, by pressure of this finger and thumb the fluid can be driven back into the suprapatellar pouch, the hydraulic impulse being clearly received by the upper hand. In this way an unmistakable sense of fluctuation can be elicited between the two hands. With practice it is easy to detect even a small effusion in this way. The ‘patellar tap’ test (Fig. 18.1C), in which the patella is tapped backwards sharply so that it strikes the femur and rebounds, though still used, is less reliable. The test is negative in the presence of fluid in two circumstances: first, when there is insufficient fluid to raise the patella away from the femur; and secondly, when there is a tense effusion. If used at all, the ‘patellar tap’ test should be used only as a supplementary method.
Thickening of synovial membrane. A thickened synovial membrane is always a prominent feature of chronic inflammatory arthritis. The thickening is often most obvious above the patella, where the reduplicated membrane forms the suprapatellar pouch. It has a characteristic boggy feel on palpation, rather as if a sheet of warm sponge-rubber had been placed between the skin and the underlying bone. It is worth emphasising that since it is highly vascular, a thickened synovial membrane is always associated with increased warmth of the overlying skin.
Tests for stability
The integrity of each of the four major ligaments is tested in turn.
Testing the medial and lateral ligaments. For this test the joint must be in a position just short of full extension, so that the posterior part of the joint capsule is relaxed: with the knee fully extended even marked laxity of the collateral ligaments can be masked by the intact posterior capsule, held taut. It must be remembered, however, that with the knee slightly flexed the medial and lateral ligaments are normally somewhat slack and allow a little side-to-side wobble. Technique: Support the limb by a hand gripping the ankle region and by the other hand behind the knee, flexing it slightly. Instruct the patient to relax the muscles. Using the more proximal hand as a fulcrum on the appropriate side of the knee, apply first an abduction force to test the medial ligament (Fig. 18.2A) and then an adduction force to test the lateral ligament. If the ligament is torn, the joint will open out more than in the normal knee when stress is applied.
Testing the anterior and posterior cruciate ligaments. The anterior cruciate ligament prevents anterior glide of the tibia on the femur; the posterior cruciate ligament prevents posterior glide. First the ligaments are tested with the knee flexed 90 °. Technique: The patient’s knee being flexed to a right angle and the foot placed firmly on the couch, sit lightly on the foot to prevent it from sliding (Fig. 18.2B). With the interlocked fingers of the two hands form a sling behind the upper end of the tibia, and clasp the sides of the leg between the thenar eminences. Place the tips of the thumbs one upon each femoral condyle. Ensure that the patient has relaxed the thigh muscles. Alternately pull and push the upper end of the tibia to determine the amount of antero-posterior movement. Normally there is an antero-posterior glide of up to half a centimetre; but since the normal is variable it is wise to use the patient’s sound limb for comparison. Excessive glide in one or other direction indicates damage to the corresponding cruciate ligament.
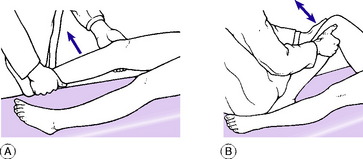
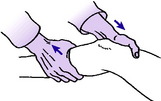
In a second test the ligaments are examined with the knee flexed only 15 ° or 20 ° (Lachman test). One hand supports the thigh just above the knee, gripping the femoral condyles, while the other hand grasps the upper end of the tibia (Fig. 18.3). While the patient relaxes the muscles the extent of any anterior or posterior glide of the tibial condyles upon the femur is determined by push-and-pull movements of the tibia.
Lateral pivot shift. The test for lateral pivot shift is supplementary to the tests described above for deficiency of the anterior cruciate ligament: it may be positive when the foregoing test is equivocal. The test depends on the fact that when the anterior cruciate ligament and the lateral ligament are deficient or lax the pivot between the lateral condyle of the femur and that of the tibia may be unstable. In that event the lateral tibial condylar surface may be displaced forwards in relation to the femoral condyle when the tibia is rotated medially with the knee straight. When the knee is then flexed the subluxation is spontaneously reduced with a visible or palpable ‘jerk’. The test is thus an indication of antero-lateral instability.
Technique. The leg on the affected side is lifted by the examiner’s corresponding hand (the right foot is lifted by the right hand; the left leg by the left hand) so that the knee drops into full extension with the muscles relaxed. The limb is supported under the arm, and with the other hand the examiner then presses against the outer aspect of the limb just below the knee, imparting a valgus strain (Fig. 18.4). At the same time the tibia is rotated medially upon the femur. The knee is now flexed slowly from the straight position. If the test is positive the lateral tibial condyle becomes spontaneously relocated on the femoral condyle when the knee reaches 30 ° or 35 ° of flexion. The relocation is evidenced by a visible or palpable jerk (hence the term ‘jerk test’ sometimes used for the manoeuvre).
Arthroscopy
Arthroscopy can be a useful adjunct to clinical and radiographic examination in the diagnosis of knee complaints (Fig. 18.5). Its use for diagnostic purposes has been largely replaced by MRI, but it is a well’established method of treating a number of intra-articular disorders by minimally invasive operation.
Arthroscopy is usually carried out with the patient anaesthetised, the joint cavity is filled with saline through a hollow needle, and a cannula and telescope are entered at the appropriate site – usually antero-laterally or antero-medially, depending upon whether the surgeon is concerned to inspect mainly the medial or the lateral compartment. By correctly manoeuvring and rotating the arthroscope, and if necessary by the use of alternative sites of entry, almost the whole extent of the interior of the joint can be brought into view with the possible exception of the postero-lateral recess. The information gained can be enhanced by probing the menisci and other intra-articular structures with an instrument introduced at a site away from the arthroscope.
DISORDERS OF THE THIGH
ACUTE OSTEOMYELITIS (General description of acute osteomyelitis, p. 85)
The femur is one of the bones most commonly affected by pyogenic osteomyelitis. The infection is carried to the femur either through the blood stream (haematogenous osteomyelitis), when it usually affects the lower metaphysis; or it is introduced through an external wound, especially in cases of compound fracture. The clinical features and treatment are the same as those of osteomyelitis elsewhere (p. 89).
CHRONIC OSTEOMYELITIS (General description of chronic osteomyelitis, p. 90)
Chronic pyogenic osteomyelitis is nearly always a sequel to acute infection that has been neglected or has responded poorly to treatment. As with the acute disease, the lower end of the femur is affected more often than the upper; but in many cases the infection spreads to involve a large part of the femoral shaft. Clinical features and treatment are like those of chronic osteomyelitis elsewhere (p. 91).
BONE TUMOURS IN THE THIGH
The femur is one of the commonest sites of the important bone tumours.
Benign tumours (General description of benign bone tumours, p. 106)
Giant-cell tumour (osteoclastoma)
The lower end of the femur is a particularly frequent site for this uncommon tumour. The upper end of the femur is affected much less often. The tumour usually arises in young adults. It begins in what was the metaphysial region, but since the epiphysis is fused there is no obstacle to its spread into the articular end of the bone (see Fig. 8.10A&B). The bone is gradually expanded, the cortex becoming very thin and pathological fracture may sometimes occur.
Malignant tumours (General description of malignant bone tumours, p. 112)
Osteosarcoma (osteogenic sarcoma)
This is usually a tumour of childhood or early adult life: when it occurs in patients beyond middle age it is usually a complication of Paget’s disease. Typically it arises in the metaphysis of a long bone, and the lower metaphysis of the femur is the favourite site. The tumour is highly malignant, with a mortality still in the region of 40% or more despite recent advances in treatment. Treatment is discussed on page 117.
Ewing’s tumour
This also occurs mainly in children or adolescents. Unlike most bone tumours, it usually affects the shaft of the bone, which it expands in a fusiform manner. Over it, layer upon layer of new bone is laid down, giving a typical ‘onion-peel’ appearance as seen in the radiographs. Although the tumour responds dramatically to chemotherapy, usually in combination with radiotherapy or surgical excision, the prognosis remains poor, with a mortality in the region of 50 per cent from blood-borne metastases. Treatment is discussed on page 121.
Metastatic (secondary) tumours
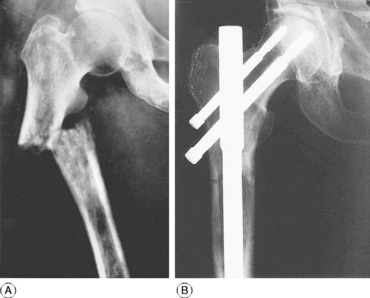
The femur is commonly invaded by metastatic tumours, especially in its proximal half (Fig. 18.6).
Pathology. The tumours that metastasise most readily to bone are carcinomas of the lung, breast, prostate, kidney, and thyroid. The bone structure is usually destroyed by the tumour and pathological fracture is common (Fig. 18.6A).
Treatment. The principles of treatment of metastatic tumours in bone were described on page 126. Most pathological fractures of the femur lend themselves well to internal fixation with a long modified intramedullary nail, though sometimes this requires the addition of acrylic bone cement to achieve stability (Fig. 18.6B). Where massive bone destruction has occurred in the proximal or distal femur, it may be necessary to replace this with a custom prosthesis. This facilitates nursing and greatly increases the quality of life because external splintage can be dispensed with and the patient mobilised.
ARTICULAR DISORDERS OF THE KNEE
PYOGENIC ARTHRITIS OF THE KNEE (General description of pyogenic arthritis, p. 96)
Treatment. Appropriate antibiotic therapy must be started immediately (see p. 98). Local treatment: The joint is rested in a plaster splint in a position of 20 ° of flexion. The purulent effusion is removed daily by aspiration so long as it re-forms or by arthrotomy. Rest is continued until the infection has been overcome; thereafter active movements are encouraged.
TUBERCULOUS ARTHRITIS OF THE KNEE (General description of tuberculous arthritis, p. 98)
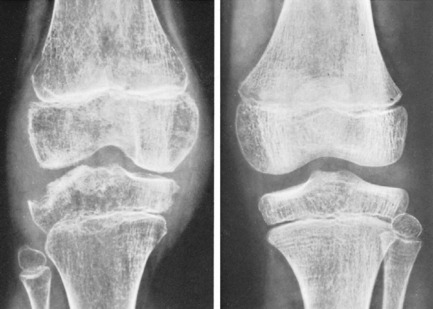
Radiographic features. The earliest change is diffuse rarefaction throughout the area of the knee (Fig. 18.7). Later, unless the disease is arrested, there is narrowing of the cartilage space and erosion of the underlying bone.
Treatment. Constitutional treatment, by antituberculous drugs, is the same as that for other tuberculous joints (p. 102). Local treatment is at first by rest in a splint or plaster, generally for two to three months in the first instance, depending on severity and progress. Subsequent management depends upon the response to treatment and the state of the joint at the end of this period of immobilisation. If the articular cartilage and bone are still intact, if the general health is good and the local signs have subsided, and if the erythrocyte sedimentation rate has steadily improved, it is likely that the disease has been aborted. In that event active joint movements are encouraged and walking is gradually resumed.
RHEUMATOID ARTHRITIS OF THE KNEE (General description of rheumatoid arthritis, p. 134)
The knees are among the joints most frequently affected by rheumatoid arthritis, and they often suffer severe permanent disability. Both knees are often affected simultaneously with several other joints.
Imaging. Radiographs do not show any abnormality at first. Later there is diffuse rarefaction of the bone in the area of the joint. In long-established cases destruction of articular cartilage leads to narrowing of the joint space (Fig. 18.8), and there may be clear-cut erosions of bone, characteristically at the articular margins. Radioisotope bone scanning shows increased uptake of isotope in the region of the joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree