Primary Adhesive Capsulitis
Primary adhesive capsulitis is the progressive loss of motion in the shoulder associated with inflammation and subsequent fibrosis. The pathogenesis of adhesive capsulitis has long been debated and is still not fully understood. In addition to the clinical symptoms, histopathologic changes in the synovium and subsynovium are observed (
7). The histology suggests both an inflammatory and fibrosing etiology, evident to varying degrees during the separate stages of the disease. There is significant evidence to support the hypothesis that adhesive capsulitis is caused by a synovial inflammation, with subsequent reactive capsular fibrosis, leading to loss of motion.
Adhesive capsulitis is described as a condition of shoulder stiffness that progresses through four stages originally described by Neviaser and Neviaser (
7).
Table 23.1 summarizes each stage. It is critical to recognize that accurate identification of the stage will guide treatment and that the presentation of the disease represents a continuum rather than a discrete stage. Each stage can be identified by duration of symptoms, arthroscopic features, range of motion limitations both clinically and under anesthesia, and histopathology. Neviaser described the arthroscopic changes of adhesive capsulitis (
1).
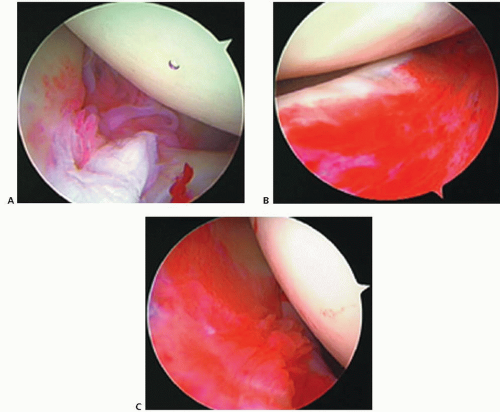
Stage I is described as the painful phase, with limited active motion secondary to painful inflammation. Passive motion is preserved when the patient is examined under anesthesia, either with a local anesthetic block or with a general anesthesia. This finding confirms the early stage of disease, as the motion loss is secondary to pain caused by inflammation rather than fibrosis. Loss of active motion occurs in forward flexion, abduction, and internal rotation, with minimal external rotation deficit. Symptoms last up to 3 months. Arthroscopic examination of the glenohumeral joint reveals diffuse synovitis, most pronounced in the anterosuperior capsule and rotator
interval (
Fig. 23.1). The histology of biopsy specimens in the painful phase reveals hypertrophic, hypervascular synovitis, with inflammatory infiltrates, but normal-appearing capsular tissue.
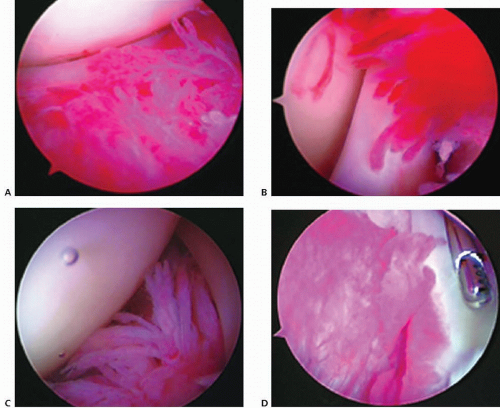
Stage II, the freezing phase, is associated with more chronic shoulder pain and significant loss of motion in all planes. The duration of symptoms is typically from months 3 to 9. An exact definition of this stage is debated based on actual degree of motion loss; however, examination under anesthesia will demonstrate only a partial loss of motion. This reflects a loss of capsular volume secondary to the onset of fibrosis. Arthroscopy reveals diffuse, dense, proliferative and hypervascular synovium (
Fig. 23.2). Cellular changes identified in biopsy specimens include new collagen deposition with disorganized collagen fibrils and no inflammatory infiltrates.
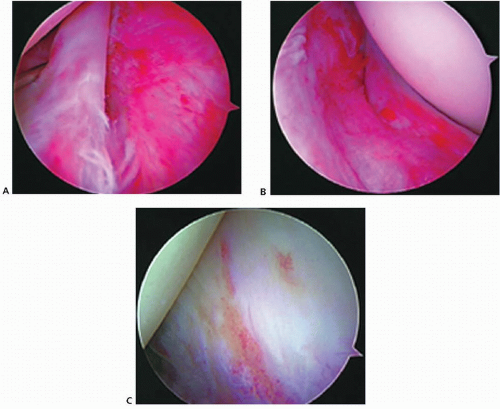
Stage III, the frozen phase, occurs between months 9 and 15. Patients in this phase report a history of improvement in their shoulder pain over time, yet continue to demonstrate stiffness. When the shoulder is examined under anesthesia, there is no improvement in passive range of motion when compared with the active motion while awake. Arthroscopic inspection reveals resolution of the hypervascular synovitis, persistent loss of capsular volume, and a residual synovial layer with patches of thickened, injected, waxy tissue (
Fig. 23.3). Biopsy of stage III capsule shows dense hypercellular, organized collagenous tissue.
Stage IV, the resolution phase, is characterized by a gradual return of motion, with no associated pain. The histologic characteristics of this phase have not been characterized, as the need for arthroscopy and biopsy is obviated.
Post-traumatic or Postsurgical Shoulder Stiffness
The layers of tissue surrounding the shoulder joint each permit a fixed amount of motion as they glide over each other. The ligaments, tendons, and muscles all have variable lengths depending on tissue elasticity and the
distances between skeletal structures. Acromion morphology has not been associated with adhesive capsulitis (
8). When any of these layers or parts is injured, inflamed, or deformed, it can result in loss of motion.
The glenoid and humeral head articulation can have altered anatomy from trauma, surgery, or arthritis (
9). This can have various effects on joint capsule volume. The effect on the capsule can be global, affecting all planes of motion. Alternatively, joint capsule tightness can involve specific locations of the capsule, with resultant effects on the individual ligaments, producing recognizable patterns of deficiency.
Contracture of the rotator interval, which is comprised in part by the coracohumeral ligament and superior glenohumeral ligament, typically limits forward flexion, extension, and external rotation when the shoulder is in the adducted position. The anteroinferior ligament complex is a restraint to external rotation in abduction. The postero-inferior complex limits internal rotation and forward flexion. Isolated contracture of these ligaments will produce limits in motion in a predictable fashion. The restraint to motion results in an increase in the translation of the humeral head opposite the side the lesion.
Capsulorrhaphy arthropathy is an example of a condition in which the humeral head is translated posteriorly by a tight anterior capsule. This results in increased joint reactive forces on the posterior glenoid and subsequent arthropathy. When both limbs of the inferior glenohumeral ligament complex are affected, the result is a superior migration producing what some have termed “non outlet impingement.”
Rotator cuff injuries and repairs have the potential to cause stiffness. In the setting of rotator cuff tear or tendinopathy, patients lose the action of dynamic stabilization. A voluntarily decreased glenohumeral motion in an effort to reduce the pain of impingement may lead to a compensatory increase in scapulothoracic motion. After surgical repair, or in the setting of a chronic, contracted tear, the rotator cuff muscle-tendon units may actually be shorter. This can result in restricted motion. It is critical to fully mobilize the
tendons from adhesions during the procedure, as well as perform appropriate releases. During the postsurgical rehabilitation, it is also important to perform early passive mobilization of the joint to prevent adhesion formation.
Intra-articular deformity is less well tolerated than extrinsic contracture in shoulder stiffness. This deformity can be caused by erosion of bone secondary to osteoarthritis or from fractures. Fractures alter the anatomy directly and potentially indirectly in the setting of post-traumatic arthritis.
In arthritis, the joint incongruity leads to global capsular thickening and scarring, secondary to an inflammatory component of the disease. Fractures of the proximal humerus can also lead to stiffness either by intra-articular incongruity or by malpositioning of the tuberosities and subsequent poor function of dynamic stabilization. Even after arthroplasty, nonanatomic reconstruction such as oversizing and poor orientation of components can lead to stiffness. Procedures to treat instability such as arthroscopic capsular plication, Bristow, Latarjet, or Trillat can successfully treat instability; however, this can be at the expense of limited motion.