The Stiff Elbow: Degenerative Joint Disease and Arthrofibrosis
Steven A. Giuseffi
Scott P. Steinmann
The operative treatment of the stiff and/or arthritic elbow has traditionally included open joint debridement or joint replacement. These open procedures were met with reasonable success, but results were tempered by relatively long recovery periods and high complication rates. As arthroscopic techniques have evolved, orthopedic surgeons have grown more interested in a more minimally invasive approach to elbow stiffness. Arthroscopic debridement of the stiff elbow offers the potential advantages of improved intraoperative articular visualization, decreased postoperative pain, and more rapid patient recovery in comparison with open procedures. Furthermore, several recent series have documented equivalent outcomes between open and arthroscopic techniques for elbow arthritis.
The articular anatomy of the elbow is complex, and the relatively small elbow capsule is surrounded by important neurovascular structures. The combination of a small working space and proximity to vital nerves and arteries initially deterred many surgeons from pursuing complex arthroscopic elbow procedures. Elbow arthroscopy was initially performed primarily for joint evaluation and loose body removal. However, an increased understanding of local neurovascular anatomy as well as increased experience with elbow arthroscopy has led to an expansion of potential surgical indications.
Elbow arthroscopy can be used for resection of symptomatic plicae, synovectomy for inflammatory arthritis, lateral epicondylitis debridement, treatment of osteochondritis dissecans, and fixation of simple elbow fractures. In addition to these indications, elbow arthroscopy may be especially useful in the setting of arthrofibrosis and/or elbow arthritis. The results of arthroscopic capsular release as well as joint debridement and osteophyte resection have been promising. The focus of this chapter will be the application of arthroscopic techniques for patients with stiff and/or arthritic elbows.
CLINICAL EVALUATION
History
Osteoarthritis, rheumatoid arthritis, and posttraumatic contractures may all lead to a stiff elbow joint. Osteoarthritis patients often have pain and stiffness, especially at the extremes of elbow motion. These patients often have relatively pain-free elbow motion in the midmotion arc. Loss of terminal extension is classically observed (1). Patients may also note weakness, cosmetic deformity, and instability. The patient should be questioned about mechanical symptoms such as locking or catching. Inflammatory arthritis often presents with elbow effusion and synovitis, polyarthropathy, morning stiffness, and systemic symptoms. Patients with this presentation warrant rheumatologic workup.
It is important to get an adequate history regarding the timeline of elbow pain and stiffness as well as any inciting events or exacerbating factors. In particular, it is crucial to ask the patient regarding any past traumatic episodes. Distal humerus fractures with resultant articular deformity can cause posttraumatic arthritis. Stiffness may also develop in the absence of bony deformity, with hemarthrosis leading to capsular contraction and fibrosis.
Any treatment received by the patient prior to presentation should also be noted. In particular, patients should be questioned regarding any physical therapy and/or splinting that they have undergone. If they have received physical therapy or undergone splinting, it is pertinent to know what type of therapy exercises were performed, the duration of therapy and/or splinting, and the patient’s results from these interventions.
The patient’s handedness as well as vocational and avocational activities are also pertinent. Osteoarthritis of the elbow is most frequently seen in the dominant arms of men with a history of heavy labor. Patients who are avid weight lifters or who are throwing athletes are also predisposed to elbow arthritis.
Physical Examination
The physical examination begins with inspection of the extremities for effusion or synovitis that may suggest inflammatory arthropathy. The elbow joint is evaluated for visual deformity as well as effusions. The elbow carrying angle is noted. The skin is inspected for rashes and prior surgical or traumatic scars. A complete neurovascular exam is essential prior to elbow arthroscopy to document preoperative function and sensation.
Examination of elbow range of motion is particularly valuable, and it is important to note both the passive and the active elbow motion arc and compare it with the contralateral side. Range of motion testing will help determine severity of functional impairment as well as provide a baseline for subsequent evaluation. Flexion contractures are commonly observed in the setting of osteoarthritis as well as arthrofibrosis. The experienced clinician may be able to distinguish between a “soft” and a “hard” endpoint that will suggest extrinsic versus intrinsic articular pathology.
Patients with osteoarthritis often have pain at the endpoints of the elbow motion arc. Crepitus may be noted. The examiner may note that the elbow locks or catches in certain positions. Testing of elbow stability is also critical and completes the physical examination.
Imaging
Imaging studies are obtained and correlated with the history and physical examination. Standard radiographic views of the elbow should include anteroposterior, lateral, and oblique projections. These are closely inspected for signs of posttraumatic deformity as well as loose bodies, which are indicative of underlying osteoarthritis. The clinician should particularly pay close attention to the olecranon and coronoid processes as well as the olecranon and coronoid fossae of the humerus, as these areas are prone to osteophytic degeneration.
CT is a valuable preoperative examination that helps characterize the size and location of osteophytes. These images are very useful for preoperative planning, particularly if three-dimensional reconstructions are obtained. CT is also indicated in the setting of malunion and posttraumatic deformity.
OPERATIVE PLANNING AND TECHNIQUE
Indications
Elbow arthroscopy is a reasonable option in the patient with symptomatic osteoarthritis and/or arthrofibrosis with loss of functional range of motion. A trial of nonoperative measures such as activity modification, nonsteroidal anti-inflammatory medications, and physical therapy and splinting are warranted prior to surgical intervention. The patient should be appropriately informed regarding the potential risks to neurovascular structures inherent in elbow arthroscopy. The patient must be willing and able to participate in any anticipated postoperative therapy or splinting regimen. Open procedures are preferred over arthroscopy in patients who have undergone significant prior elbow surgery (particularly on the lateral aspect of the elbow as this may lead to scarring near radial nerve) or who have severe bony deformity or capsular retraction.
Anesthesia and Patient Positioning
The first decision in performing elbow arthroscopy is to determine the type of anesthesia to be used. The authors recommend general anesthesia for various reasons, though axillary blocks may also be used. Elbow arthroscopy requires that the patient assume a prone or lateral decubitus position, which can be uncomfortable and awkward for the patient. In a complex arthroscopic case with duration exceeding 1 hour, the patient may experience significant discomfort that can be difficult to control and may jeopardize the success of the procedure. In addition, the use of a nerve block precludes an accurate postoperative neurologic examination. As there is a very real risk of neurovascular injury during elbow arthroscopy, an accurate postoperative examination is critical. In the setting of an axillary nerve block, it may be several days before a postoperative neurologic complication is discovered. Therefore, general anesthesia is recommended as long as the patient’s overall medical health does not preclude it.
Patient positioning for elbow arthroscopy is dependent on surgeon preference. Poehling and colleagues (2) first described prone positioning, and many orthopedic surgeons have modified this to a lateral decubitus position. The lateral decubitus position allows the elbow to be positioned, so that it is highest in the operative field, which improves access to the joint and allows the surgeon to maneuver arthroscopic equipment around the elbow without impinging against the side of the patient’s body (3).
It is best to obtain an elbow arm support made specifically for elbow arthroscopy (3). The use of a knee holder impedes access to the elbow. The patient can be tilted 10° to 20° toward the operating surgeon to prevent rollback of the patient and to maintain proper positioning within the arm holder. This helps avoid compression on the antecubital fossa.
A pillow is placed between the patient’s legs and the proximal fibulae are well padded. A back support brace is applied to maintain torso positioning, and a strap is placed over the patient’s waist. A nonsterile tourniquet is applied as proximally as possible on the operative arm at the level of the arm holder (Figs. 34.1, 34.2, 34.3 and 34.4).
Starting Portal Placement
The potential for neurovascular injury with elbow arthroscopy is relatively high as compared with arthroscopy of the knee and shoulder, and much attention has been given to safe portal placement. It is essential to understand the local anatomy and know the safe zones for portal placement.
The order of portal placement is not as critical as a solid understanding of relevant elbow anatomy.
The order of portal placement is not as critical as a solid understanding of relevant elbow anatomy.
 FIGURE 34.1. Patient positioned for elbow arthroscopy. Lateral decubitus position with the unaffected elbow on an arm board. (From Steinmann SP. Elbow arthroscopy. J Am Soc Surg Hand. 2003;3:199-207; Figure 1, with permission.) |
 FIGURE 34.2. Elbow arthroscopy arm holder attaches to the side of the operating table. (From Steinmann SP. Elbow arthroscopy. J Am Soc Surg Hand. 2003;3:199-207; Figure 2, with permission.) |
All portal sites should be marked prior to surgery. This allows the surgeon to determine bony landmarks before the joint is distended or the soft tissues edematous. The lateral epicondyle, medial epicondyle, radial head, capitellum, and olecranon should all be marked out. The elbow is then distended with 20 to 30 cc of saline, using a syringe and 18G needle. The needle is usually placed through the “soft spot” that lies in the middle of the triangle bordered by the olecranon, radial head, and lateral epicondyle. Alternatively, the joint can be distended with an injection directly posterior just proximal to the olecranon tip. Distending the elbow prior to establishing the
starting portal is an important step, as distending the joint positions the major neurovascular structures further from the starting portal and facilitates initial portal insertion. In a nondistended elbow, inserting the trocar for the starting portal is considerably more difficult and more dangerous.
starting portal is an important step, as distending the joint positions the major neurovascular structures further from the starting portal and facilitates initial portal insertion. In a nondistended elbow, inserting the trocar for the starting portal is considerably more difficult and more dangerous.
 FIGURE 34.3. Patient positioned for elbow arthroscopy. The elbow is elevated to allow 360° of access. (From Steinmann SP. Elbow arthroscopy. J Am Soc Surg Hand. 2003;3:199-207; Figure 3, with permission.) |
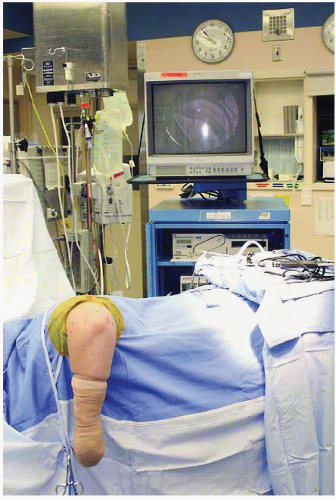 FIGURE 34.4. The surgeon’s view during elbow arthroscopy. Monitor positioned on opposite side of the table. (From Steinmann SP. Elbow arthroscopy. J Am Soc Surg Hand. 2003;3:199-207; Figure 4, with permission.) |
After the joint is distended, it is time to establish a starting portal. The choice of starting portal is a matter of surgeon preference. The surgeon’s experience and anatomic knowledge is more important in preventing neurovascular injury than the order of portal placement. Portal sites should be made with a no. 11 blade. The knife scalpel should be drawn across the skin only without penetration into the deeper soft tissues. Once the skin is divided, a small hemostat can be used to spread down to the joint capsule and enter the joint. Joint entry is confirmed by release of the previously injected saline from the capsule. The blunt trocar is then used to enter the joint. Using a sharp trocar is avoided during elbow arthroscopy as this can damage neurovascular structures.
The trocar is then exchanged for the arthroscope, and evaluation of the joint commences. A 4-mm, 30° arthroscope is the workhorse for elbow arthroscopy. Some advocate the use of a 70° scope, but as this is seldom used in general arthroscopic practice, it may be disorienting. A 2.7-mm arthroscope can be used in a contracted joint but is not needed in most patients. However, in certain spots such as the direct lateral (soft spot) portal, the smaller scope may be easier to manipulate.
Once the arthroscope has entered the joint, the surgeon must then obtain visualization and create a space in which to work. This can be performed through pressure distention or mechanical retraction. Both methods function well, but pressure distention will eventually cause fluid to extravasate into the tissues during the course of the procedure. Kelly and colleagues (4) recommended using retractors as a means of mechanical retraction to avoid this complication. Simple lever retractors such a Howarth or large, blunt Steinmann pins are effective. Retractors are typically placed into the elbow joint through an accessory portal that is 2 to 3 cm proximal to the viewing portal (Fig. 34.5).
Again, the choice of starting portal is a matter of surgeon preference as safe entry into the joint can occur from either the medial or the lateral approach. The radial nerve is the structure at greatest risk during portal placement. There are two methods of minimizing risk of radial nerve injury. The first technique is to establish the anterolateral portal first when bony landmarks are clearly palpable. The anteromedial portal can then be established from a direct inside-out approach.
Alternatively, the surgeon can choose to establish the anteromedial portal first and then create an anterolateral portal under direct arthroscopic visualization. The anteromedial portal is relatively distant from the medial and ulnar nerves, and it is fairly safe to start with this portal. Arthroscopic observation of the lateral capsule during anterolateral portal placement, however, is not fail proof. A misdirected needle or trocar could damage the radial nerve despite intra-articular visualization.
 FIGURE 34.5. Elbow arthroscopy retractors. Three Howarth retractors and one blunt Steinmann pin. (From Steinmann SP. Elbow arthroscopy. J Am Soc Surg Hand. 2003;3:199-207; Figure 8, with permission.) |
SPECIFIC PORTALS
Anterolateral
The anterolateral portal was originally described by Andrews and Carson (5). Anatomic studies have shown that the posterior antebrachial nerve and radial nerve are quite close to the anterolateral portal (6). A safe approach is to place the portal in the sulcus between the radial head and the capitellum. This area is fairly easy to locate prior to the onset of fluid extravasation and soft tissue edema. The skin is incised, a hemostat is used to spread to the joint and aimed toward the joint center. To minimize risk of radial nerve injury, it is advisable to place a cannula in the anterolateral portal and then pass all instruments through the cannula. This eliminates blind passes into the joint.
Once in the joint, the surgeon should be able to visualize the medial radial head, coronoid process, trochlea, and coronoid fossa from the anterolateral portal. The anteromedial portal can then be started through an inside-out technique. The arthroscope is removed from the sheath, and a blunt trocar is passed through the sheath straight across the joint until it tents the medial elbow skin. The skin is then incised over this trocar, and the sheath is
pushed out of the skin. A cannula is then placed over the tip of the sheath, and the arthroscope is inserted into this cannula while gently retracting the trocar. In this manner, the cannula and trocar are pulled back into the joint together, with the arthroscope inside the cannula and following the trocar down into the elbow joint. Because the interval between the median and the ulnar nerves is relatively wide on the medial elbow, this inside-out technique of establishing the anteromedial portal is quite safe (Figs. 34.6, 34.7 and 34.8).
pushed out of the skin. A cannula is then placed over the tip of the sheath, and the arthroscope is inserted into this cannula while gently retracting the trocar. In this manner, the cannula and trocar are pulled back into the joint together, with the arthroscope inside the cannula and following the trocar down into the elbow joint. Because the interval between the median and the ulnar nerves is relatively wide on the medial elbow, this inside-out technique of establishing the anteromedial portal is quite safe (Figs. 34.6, 34.7 and 34.8).
 FIGURE 34.6. Anterolateral portal located anterior to the radiocapitellar joint. (From Steinmann SP. Elbow arthroscopy. J Am Soc Surg Hand. 2003;3:199-207; Figure 5, with permission.) |
 FIGURE 34.7. Direct posterior portal. (From Steinmann SP. Elbow arthroscopy. J Am Soc Surg Hand. 2003;3:199-207; Figure 6, with permission.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





