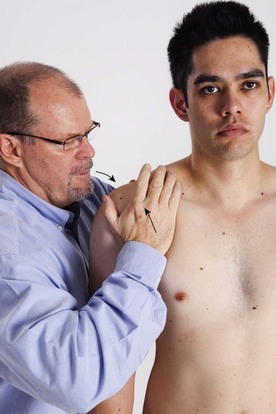
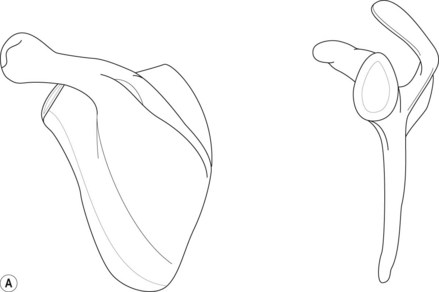
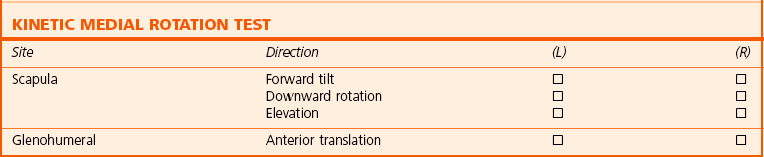
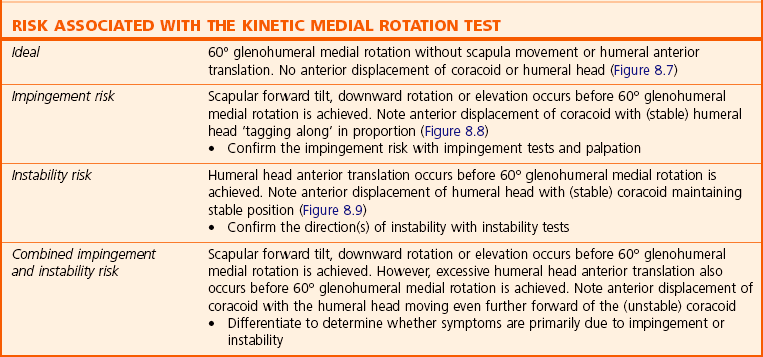
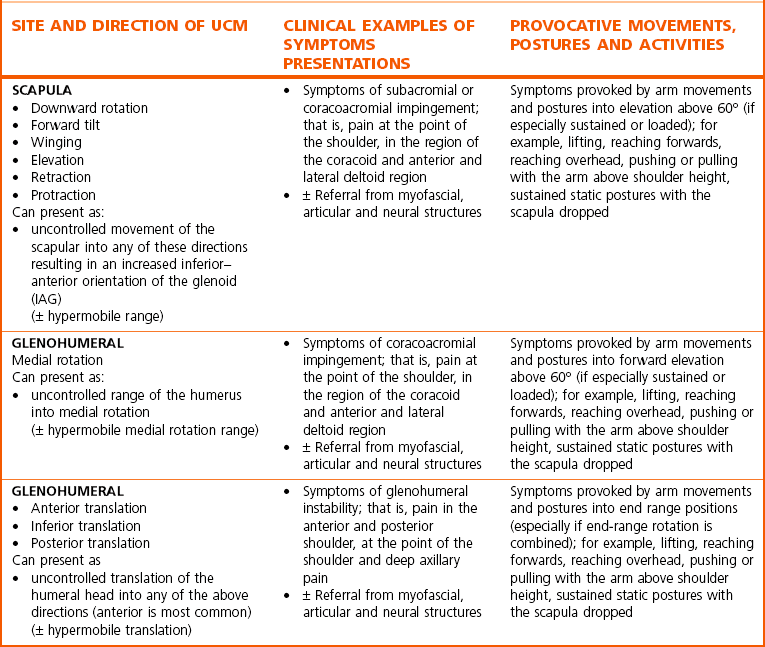
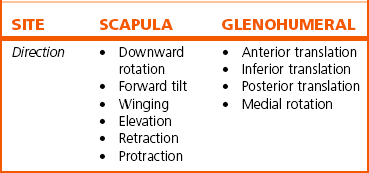
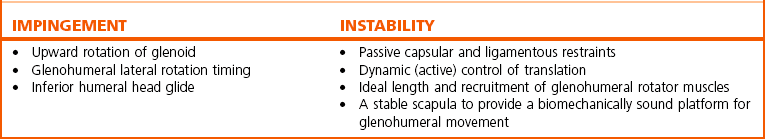
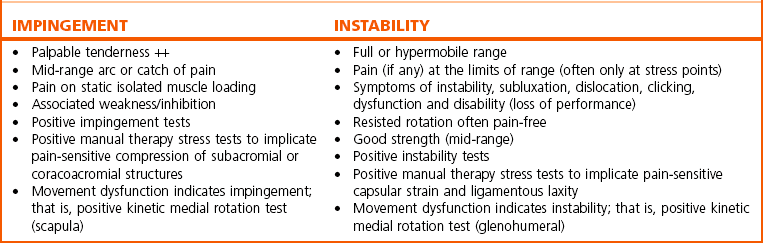
Chapter 8 The complexity of shoulder girdle dysfunction makes diagnosis difficult, with definitions for common diagnoses, such as impingement and frozen shoulder, being unclear, inconsistent and unreliable (Schellingerhout et al 2008). An epidemiological study examining 1960 people successfully identified current and past shoulder problems, but was unable to discriminate between discrete shoulder pathologies (Walker-Bone et al 2004). Therapy for shoulder girdle pain and disability is predominantly concerned with restoration of optimal movement and function rather than applying diagnostic labels, with traditional approaches to clinical diagnosis at the shoulder girdle frequently neglecting to assess dynamic movement faults, a significant factor associated with shoulder dysfunction (Lukasiewicz et al 1999; Ludewig & Cook 2000; Lin et al 2006; Tate et al 2008). Classification of movement control faults at the shoulder girdle is gaining recognition, with Kibler & McMullen (2003) describing a clinical classification of scapular dyskinesis (scapular movement control faults). A classification of dysfunction in terms of site and direction of uncontrolled movement (UCM) has been proposed (Mottram 2003; Mottram et al 2009a; Comerford & Mottram 2011), and diagnosis based on movement impairment (Sahrmann 2002; Caldwell et al 2007) encouraged. The consensus statement at a recent scapular summit (Kibler et al 2009) agreed that the observation of scapular dyskinesis and clinical tests that alter symptoms (UCM in this text) should form the basis for the scapular evaluation. The ability to control the orientation and movement of the scapula is essential for optimal arm function. The bony, capsular and ligamentous restraints are minimal at the scapulothoracic ‘joint’ so stability is dependent on active muscular control. Movement faults and changes in muscle function of the scapula are associated with shoulder symptoms (Lukasiewicz et al 1999; Ludewig & Cook 2000; Lin et al 2006; Roy et al 2008; Tate et al 2008). The glenohumeral joint has the greatest range of motion of any human joint. This mobility is necessary for upper limb functions, which range from weight bearing to high-speed acceleration and deceleration at the extremes of its range. Stability is sacrificed to a significant degree to achieve this mobility function. The scapula provides the base for attachment of muscles that move the glenohumeral joint. The scapula should be orientated to optimise the length–tension relationship of these muscles (van der Helm 1994) and provides the proximal articular surface of the glenohumeral joint (glenoid) and orientates the glenoid, to increase the range available to the upper limb. The scapula facilitates optimal contact with the humeral head – increasing joint congruency and stability (Saha 1971). Abnormal scapular kinematics have been identified in people with multidirectional instability (Ogston & Ludewig 2007). Full upward rotation of the glenoid enhances mechanical stability of the joint by bringing the glenoid fossa directly under the head of the humerus (Lucas 1973) and prevents impingement under the subacromial and coracoacromial arch. Glenohumeral function is influenced to a large extent by the position and orientation of the glenoid and hence scapula stability; however, the glenohumeral joint exhibits a number of mechanisms to retain joint congruency during functional movement which include passive stability mechanisms and active stability mechanisms. Passive stability mechanisms include the capsular and ligamentous restraints, labrum and mechanisms such as the creation on negative intra-articular pressure to resist translation. Muscle stiffness is required at the scapula-thoracic and glenohumeral to enhance stability. It has been shown that moderate levels of muscle contraction can significantly increase glenohumeral joint stiffness and stability (Huxel et al 2008). A non-specific pre-setting action of the rotator cuff and biceps is seen prior to rotation of the shoulder joint, and this recruitment is aimed mainly at enhancing the joint ‘stiffness’ and hence its stability (David et al 2000). A similar action is seen in upper trapezius (Wadsworth & Bullock-Saxton 1997), suggesting it has a pre-setting role at the scapula. Evidence suggests that muscle function around the shoulder girdle can be impaired by pain and pathology. Altered timing (latency) of electromyographic (EMG) activity has been identified in muscles of the scapula (Wadsworth & Bullock-Saxton 1997; Cools et al 2003; Lin et al 2005; Falla et al 2007; Moraes et al 2008) and the glenohumeral joint (Hess et al 2005). Interestingly, muscle function (or dysfunction) has been associated with movement faults; for example, decreased serratus anterior activity has been associated with an increase in forward tilt of the scapula (Ludewig & Cook 2000; Lin et al 2005). This literature supports the need for specific assessment of movement faults so individual rehabilitation strategies can be implemented. Further research is needed to explore the relationship between movement abnormalities and symptoms and muscle function. Motion analysis studies have identified abnormal movements of the scapula which include scapula internal rotation (Ludewig & Cook 2000; Nawoczenski et al 2003; Tsai et al 2003; Borstad & Ludewig 2005; Borstad 2006); scapular downward rotation (Ludewig & Cook 2000; Tsai et al 2003; Lin et al 2006); scapula anterior tilt (Lukasiewicz et al 1999; Ludewig & Cook 2000; Nawoczenski et al 2003; Borstad & Ludewig 2005; Lin et al 2005; Morrissey 2005); and elevation (Lukasiewicz et al 1999; Tsai et al 2003; Lin et al 2005). UCM of the glenohumeral joint has been identified and includes translation (Baeyens et al 2001; Ruediger et al 2002; von Eisenhart-Rothe et al 2002, Ludewig and Cook 2002) and external rotation (Baeyens et al 2001). In the current literature it is clear that alterations in dynamic control of the glenohumeral and scapula-thoracic joints are important factors in shoulder pathology (Ludewig and Cook 2000; Morrissey 2005; Alexander 2007; Ogston & Ludewig 2007). Although these studies demonstrated clear differences in movement patterns for symptomatic shoulders, they do not describe test manoeuvres that could be used specifically to detect the abnormalities in the clinical environment, therefore neglecting a significant component of assessment. This chapter details the assessment of UCM at the shoulder region and describes retraining strategies. The diagnosis of site and direction of UCM at the shoulder girdle can be observed at the scapula in terms of downward rotation, forward tilt, winging (internal rotation), elevation, retraction and protraction (abduction) and the glenohumeral joint in terms of anterior, inferior, posterior translation and medial rotation (Table 8.1). The site and direction of UCM at the scapula and the glenohumeral joint can be linked to different clinical presentations and postures and activities that provoke or produce symptoms (Table 8.2). Table 8.2 The link between the site and direction of UCM at the shoulder and different clinical presentations In a shoulder with signs and symptoms of impingement and instability, control of movement needs to be effective to manage symptoms and dysfunction. These mechanisms are highlighted in Table 8.3 and the assessment of these mechanisms is an important aspect of a comprehensive shoulder girdle assessment. The site and direction of uncontrolled movement at the shoulder girdle can be linked to different clinical presentations of shoulder impingement syndrome and glenohumeral instability. Table 8.4 illustrates the clinical guidelines for impingement and instability. The key principles for assessment and classification of UCM are described in Chapter 3. All dissociation tests are performed with the scapula and glenohumeral in the neutral training region. This can be passively positioned by the therapist prior to each test. The subject needs to clearly understand the test and appropriate facilitation strategies employed, including cognitive awareness, tactile, visual and technological feedback, and proprioceptive input. As a useful guide to repositioning the scapula in the neutral training region, the therapist stands to the side of the patient’s shoulder and places the pisiform and ulnar border of one hand on the medial side of the patient’s inferior scapular angle. The therapist then places the ulnar border of the other hand on the patient’s coracoid with the hollow of the palm over the humeral head (Figure 8.1). With the fingers of both hands pointing to the ceiling, the therapist lifts both their elbows so that both forearms are in line. The therapist then gently ‘squeezes’ both hands together so that the acromion rises up, the humeral head moves backwards and the inferior scapular angle moves laterally around the chest wall (Figure 8.2). While the therapist passively supports the shoulder here, the person is asked to relax the shoulder and then is asked to use ‘minimal’ effort to actively maintain this position (Figure 8.3). With the scapula being actively maintained in this position, the therapist should palpate a series of landmarks (Box 8.1) and make any minor adjustments required. A common dysfunction pattern seen with loss of scapula neutral is the orientation of the glenoid in an inferior anterior direction, termed the inferior anterior glenoid (IAG) (Figure 8.4). This can be corrected by rotation of the scapula in the coronal plane – observed by the acromion moving superiorly while the inferior angle moves laterally (upward rotation of the scapula in the sagittal plane). The scapula also moves upward and backward (posterior or backward tilt) (Mottram et al 2009b) away from the IAG position. The therapist passively stabilises the scapula and glenohumeral joint and assesses the passive range of glenohumeral rotation without compensation (Figure 8.5). • Restrictions – reduced glenohumeral medial rotation with the arm abducted. When the scapula and humeral head are passively supported to control scapula-thoracic movement or glenohumeral anterior translation, a significant loss of glenohumeral medial rotation is often observed. Ideal passive range of medial rotation is 60°. Loss of medial rotation range may be due to several reasons: • UCM – compensatory strategies associated with restriction of glenohumeral joint medial rotation. A variety of compensation strategies for restrictions can be employed to maintain functional range of motion. If glenohumeral medial rotation is restricted, compensatory movement can be made at both the scapula and the humeral head (Sahrmann 2002; Morrissey 2005). 1. hypermobile medial rotation range 2. discrepancies of shoulder medial rotation range in different positions of arm elevation 3. excessive initiation of scapular compensation during shoulder medial rotation 4. excessive glenohumeral translation during medial rotation 5. symptoms (pain, discomfort, strain) associated with shoulder medial rotation movements. Start supine and with the humerus in 90° abduction (hand to the ceiling), and the humerus supported in the plane of the scapula. The therapist palpates the coracoid and humeral head during the procedure (Figure 8.6). The accuracy of this palpation has been measured (Morrissey et al 2008). Medial rotation of the humerus should occur without compensation at the scapula or glenohumeral joint. The scapula should not move into forward tilt, downward rotation or elevation and the humeral head should not translate anteriorly (Morrissey 2005). There should be 60° of active medial rotation (Figure 8.7). An alternative test position is in standing with or without wall support of the scapula. T60.1 Assessment and rating of low threshold recruitment efficiency of the Kinetic Medial Rotation Test These UCMs have been linked to pathology. The scapula may forward tilt, downwardly rotate or elevate to compensate for the loss of medial rotation. A positive test (scapula UCM) has been linked with risk of impingement and symptoms (Morrissey 2005). The test is useful for diagnosis, especially for impingement, particularly when used with other impingement tests (Morrissey 2005). Uncontrolled anterior translation of the humeral head compensates for a lack of glenohumeral medial rotation. A positive test (glenohumeral UCM) has been linked with instability symptoms and risk (Morrissey 2005) (T60.3). With visual, auditory and kinaesthetic cues the person becomes familiar with the task of medially rotating the glenohumeral joint to 60° without scapula movement or glenohumeral translation. Some useful clinical cues are illustrated in Box 8.2. Lean against a wall with the wall supporting the shoulder blade position. The upper body has to turn 15–30° off the wall so that the shoulder blade and upper arm can be supported flat on the wall. Only rotate the shoulder forwards as far as the neutral scapula can be controlled (Figure 8.10). When rotation control on the wall is efficient progress to the same movement unsupported away from the wall (Figure 8.11). The therapist assesses the passive range of glenohumeral lateral rotation. There should be 45° of independent passive lateral rotation. It should be relatively easy to independently dissociate the 45° glenohumeral lateral rotation from the scapular movement (Figure 8.12). • Reduced glenohumeral lateral rotation with the elbow by side. Functional restrictions of glenohumeral lateral rotation are identified with the scapula stabilised and the arm by the side. A significant loss of glenohumeral lateral rotation with the arm by the side is frequently identified. This restriction of functional lateral rotation range may be due to several reasons: • UCM – compensatory strategies associated with restriction of glenohumeral joint lateral rotation. If lateral rotation is restricted, different compensation strategies can be seen:
The shoulder girdle
Introduction
Scapula function and glenohumeral joint stability
Changes in shoulder muscle function
Identifying UCM at the shoulder girdle
Diagnosis of the site and direction of UCM at the shoulder girdle
Linking the site of UCM to symptom presentation
Identifying site and direction of UCM at the scapulothoracic and glenohumeral joints
Scapula and glenohumeral joint neutral training region
Inferior anterior glenoid (IAG)
Observation and analysis of shoulder medial rotation
Description of ideal pattern
Movement faults associated with glenohumeral medial rotation
Relative stiffness (restrictions)
 Capsular restriction. Capsular shortening may contribute to a loss of medial rotation, though this is not the most common cause. If capsular shortening is present then there is usually a significant loss of lateral rotation first observed as less than 90° lateral rotation in abduction.
Capsular restriction. Capsular shortening may contribute to a loss of medial rotation, though this is not the most common cause. If capsular shortening is present then there is usually a significant loss of lateral rotation first observed as less than 90° lateral rotation in abduction.
 Myofascial restriction. Over-activity, dominance and relative stiffness of the glenohumeral lateral rotator muscles: a common presentation-related to the loss of medial rotation is over-activity and shortening of the lateral rotator muscles (infraspinatus and teres minor). Assessment of both the contractile and connective tissue shortening needs to be made and appropriate soft tissue work applied.
Myofascial restriction. Over-activity, dominance and relative stiffness of the glenohumeral lateral rotator muscles: a common presentation-related to the loss of medial rotation is over-activity and shortening of the lateral rotator muscles (infraspinatus and teres minor). Assessment of both the contractile and connective tissue shortening needs to be made and appropriate soft tissue work applied.
 Co-contraction rigidity. Occasionally, active medial rotation range at the glenohumeral joint may be limited by co-contraction rigidity. In the attempt to medially rotate, all glenohumeral muscles co-contract excessively and seem to ‘splint’ the shoulder from achieving full rotation. This is often a guarding response associated with instability or acute pathology or a protective ‘spasm’ in an acute inflammatory episode.
Co-contraction rigidity. Occasionally, active medial rotation range at the glenohumeral joint may be limited by co-contraction rigidity. In the attempt to medially rotate, all glenohumeral muscles co-contract excessively and seem to ‘splint’ the shoulder from achieving full rotation. This is often a guarding response associated with instability or acute pathology or a protective ‘spasm’ in an acute inflammatory episode.
Relative flexibility (potential UCM)
 Uncontrolled scapula forward tilt, downward rotation or elevation. The scapula may forward tilt, downwardly rotate or elevate to compensate for the loss of medial rotation. The accuracy of this palpation has been validated with three-dimensional ultrasound and motion analysis measures (Morrissey et al 2008). A positive test (scapula movement) has been linked with risk of impingement and symptoms (Morrissey 2005). The test is useful for diagnosis, especially for impingement, particularly when used with other impingement tests (Morrissey 2005).
Uncontrolled scapula forward tilt, downward rotation or elevation. The scapula may forward tilt, downwardly rotate or elevate to compensate for the loss of medial rotation. The accuracy of this palpation has been validated with three-dimensional ultrasound and motion analysis measures (Morrissey et al 2008). A positive test (scapula movement) has been linked with risk of impingement and symptoms (Morrissey 2005). The test is useful for diagnosis, especially for impingement, particularly when used with other impingement tests (Morrissey 2005).
 Uncontrolled glenohumeral translation control. Excessive anterior translation of the humeral head compensates for a lack of glenohumeral medial rotation. A positive test (glenohumeral movement) has been linked with instability symptoms and risk (Morrissey 2005).
Uncontrolled glenohumeral translation control. Excessive anterior translation of the humeral head compensates for a lack of glenohumeral medial rotation. A positive test (glenohumeral movement) has been linked with instability symptoms and risk (Morrissey 2005).
Indications to test for shoulder medial rotation UCM
Test of shoulder medial rotation control
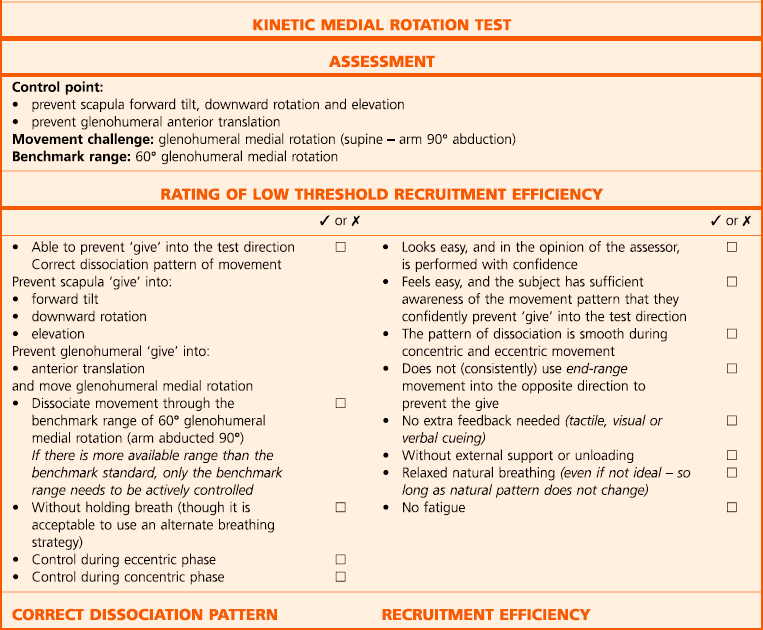
t60 Kinetic medial rotation test (KMRT) (tests for scapula and glenohumeral UCM)
Test procedure
Rating and diagnosis of shoulder girdle UCM
Correction
An alternative position for retraining the KMRT
Shoulder lateral rotation control
Observation and analysis of shoulder lateral rotation
Description of ideal pattern
Movement faults associated with glenohumeral lateral rotation
Relative stiffness (restriction)
 Capsular restriction. A capsular restriction may cause a loss of lateral rotation with the arm by the side but there will be significant (if not greater) loss of lateral rotation with the arm elevated to 90°. Examination of the shoulder ‘quadrant’ test (Maitland et al 2005) would be positive for a capsular restriction. If at 90° of arm abduction the lateral rotation range is normal then the capsule is a very unlikely source of restriction.
Capsular restriction. A capsular restriction may cause a loss of lateral rotation with the arm by the side but there will be significant (if not greater) loss of lateral rotation with the arm elevated to 90°. Examination of the shoulder ‘quadrant’ test (Maitland et al 2005) would be positive for a capsular restriction. If at 90° of arm abduction the lateral rotation range is normal then the capsule is a very unlikely source of restriction.
 Loss of posterior translation of the humerus at limit of lateral rotation. At the limit of active or passive glenohumeral lateral rotation the capsule tensions anteriorly and the humeral head is forced to translate posteriorly in order to achieve full range (Moseley et al 1992; Wilk et al 1997). A loss of this posterior translation of the humeral head at the limit of lateral rotation can significantly reduce the ability to achieve full active or passive lateral rotation at the shoulder when the arm is by the side. This is identified by a decreased range of joint play and a restricted end feel on posterior translation of the humeral head at end range lateral rotation. Appropriate mobilisation of this articular restriction (e.g. with glenohumeral accessory anteroposterior glides at the limit of physiological lateral rotations) is often appropriate here.
Loss of posterior translation of the humerus at limit of lateral rotation. At the limit of active or passive glenohumeral lateral rotation the capsule tensions anteriorly and the humeral head is forced to translate posteriorly in order to achieve full range (Moseley et al 1992; Wilk et al 1997). A loss of this posterior translation of the humeral head at the limit of lateral rotation can significantly reduce the ability to achieve full active or passive lateral rotation at the shoulder when the arm is by the side. This is identified by a decreased range of joint play and a restricted end feel on posterior translation of the humeral head at end range lateral rotation. Appropriate mobilisation of this articular restriction (e.g. with glenohumeral accessory anteroposterior glides at the limit of physiological lateral rotations) is often appropriate here.
 Loss of extensibility of myofascial structures. It may be possible that excessive shortening of myofascial structures may limit lateral rotation range. Pectoralis major and latissimus dorsi may limit lateral rotation with the arm high overhead but for lateral rotation to be limited when the arm is by the side, subscapularis and teres major are likely to be very short. Clinically, this is uncommon but may be associated with a prolonged period of immobilisation, surgery and capsular shortening.
Loss of extensibility of myofascial structures. It may be possible that excessive shortening of myofascial structures may limit lateral rotation range. Pectoralis major and latissimus dorsi may limit lateral rotation with the arm high overhead but for lateral rotation to be limited when the arm is by the side, subscapularis and teres major are likely to be very short. Clinically, this is uncommon but may be associated with a prolonged period of immobilisation, surgery and capsular shortening.
 Co-contraction rigidity. Occasionally, active lateral rotation range at the glenohumeral joint may be limited by co-contraction rigidity. This is often a guarding response associated with instability or acute pathology or protective ‘spasm’ in an acute inflammatory episode.
Co-contraction rigidity. Occasionally, active lateral rotation range at the glenohumeral joint may be limited by co-contraction rigidity. This is often a guarding response associated with instability or acute pathology or protective ‘spasm’ in an acute inflammatory episode.
 Uncontrolled scapula retraction (scapular retraction initiating or dominating glenohumeral lateral rotation). This can be assessed in standing with the arm by the side. This is most frequently associated with a functional loss of glenohumeral lateral rotation range and the development of greater relative flexibility at the scapulothoracic joint. Instead of scapular retraction providing extra movement after the glenohumeral joint has completed lateral rotation, scapular retraction increases to compensate for the inefficient glenohumeral movement. In extreme cases the recruitment of scapular retraction even precedes the recruitment of glenohumeral lateral rotation.
Uncontrolled scapula retraction (scapular retraction initiating or dominating glenohumeral lateral rotation). This can be assessed in standing with the arm by the side. This is most frequently associated with a functional loss of glenohumeral lateral rotation range and the development of greater relative flexibility at the scapulothoracic joint. Instead of scapular retraction providing extra movement after the glenohumeral joint has completed lateral rotation, scapular retraction increases to compensate for the inefficient glenohumeral movement. In extreme cases the recruitment of scapular retraction even precedes the recruitment of glenohumeral lateral rotation.
 Uncontrolled scapula downward rotation. The apparent loss of lateral rotation is very commonly due to a lack of ability to position the glenoid in neutral alignment. If the glenoid is downwardly rotated then lateral rotation can be limited. This is confirmed by passively positioning the scapula in correct alignment. When the scapula (and glenoid) is in neutral alignment the active lateral rotation movement returns to normal.
Uncontrolled scapula downward rotation. The apparent loss of lateral rotation is very commonly due to a lack of ability to position the glenoid in neutral alignment. If the glenoid is downwardly rotated then lateral rotation can be limited. This is confirmed by passively positioning the scapula in correct alignment. When the scapula (and glenoid) is in neutral alignment the active lateral rotation movement returns to normal.
 Uncontrolled scapula forward tilt. This is similar to the above. If the glenoid is orientated antero-inferiorly, lateral rotation can be limited. This is confirmed by passively positioning the scapula in correct alignment. When the scapula (and glenoid) is in neutral alignment the active lateral rotation movement returns to normal.
Uncontrolled scapula forward tilt. This is similar to the above. If the glenoid is orientated antero-inferiorly, lateral rotation can be limited. This is confirmed by passively positioning the scapula in correct alignment. When the scapula (and glenoid) is in neutral alignment the active lateral rotation movement returns to normal.
 Uncontrolled glenohumeral anterior translation. The apparent loss of lateral rotation may be related to an unstable glenohumeral joint. If the glenohumeral joint has excessive anterior translation (due to anterior capsular laxity or instability) then the axis of rotation is displaced and normal lateral rotation cannot be achieved. If the humeral head is palpated with the shoulder resting at end range lateral rotation it is observed to be prominent anteriorly. Upon assessment of a posterior translational glide in this position, a significantly increased range of joint play and a lax soft end feel is identified. This cause of dysfunction is confirmed if full lateral rotation range returns when the humeral head is passively glided posteriorly and maintained in its neutral position.
Uncontrolled glenohumeral anterior translation. The apparent loss of lateral rotation may be related to an unstable glenohumeral joint. If the glenohumeral joint has excessive anterior translation (due to anterior capsular laxity or instability) then the axis of rotation is displaced and normal lateral rotation cannot be achieved. If the humeral head is palpated with the shoulder resting at end range lateral rotation it is observed to be prominent anteriorly. Upon assessment of a posterior translational glide in this position, a significantly increased range of joint play and a lax soft end feel is identified. This cause of dysfunction is confirmed if full lateral rotation range returns when the humeral head is passively glided posteriorly and maintained in its neutral position.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 of the humeral head should protrude forward of the acromion.
of the humeral head should protrude forward of the acromion.