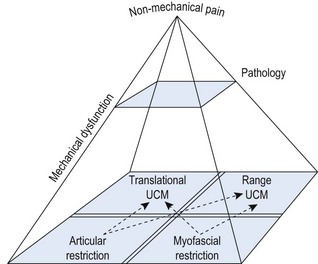
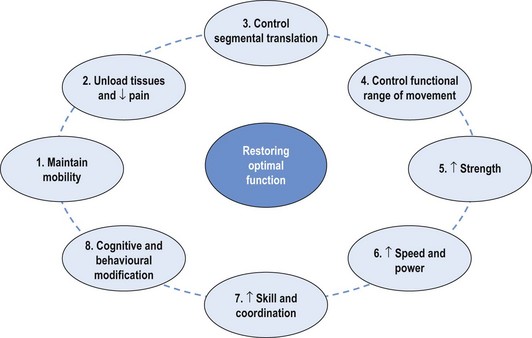
Chapter 4 The retraining of efficient control of uncontrolled movement (UCM) will depend on the pattern of the dysfunction and the site and direction of the UCM. From the assessment (as outlined in Chapter 3) the translation and range of UCM and restriction will have been identified. Correcting aberrant motor control and recruitment patterns is the priority in the rehabilitation of the local stability system. Correcting length and recruitment dysfunction is the priority of the global system. Addressing the UCM and restriction is the key to rehabilitation and this principle is covered throughout this text. As well as dealing with mechanical components of movement dysfunction the pathology must be addressed and non-mechanical issues identified and managed. Dependent upon reported signs and symptoms, local tissues should be assessed to identify the pain-producing or most damaged structure(s). Intervention may include treatment of the pain mechanisms, inflammation and pathology with techniques such as large amplitude manual mobilisations, cryotherapy, heat, active exercise, electrophysiological modalities, neurodynamic techniques, acupuncture, trigger point release, positional release and appropriate medication. These interventions should be supplemented with fitness and exercise programs which are effective approaches for the management of chronic low back pain (Frost et al 1998; Torstensen et al 1998). Consideration and management of psychosocial factors is also essential in the management of chronic low back pain and other chronic musculoskeletal conditions. Cognitive behavioural approaches have a significant role to play for optimal outcomes in chronic low back pain (Waddell 2004). The more multifactorial the patient’s pain presentation is, the more likely a multidisciplinary approach will be required. The clinical reasoning framework to encompass these factors has previously been described in Chapter 1. In the integrated management of musculoskeletal pain there are several factors that require consideration (Figure 4.1). It is important to relate the site and direction of UCM to symptoms and pathology and to the mechanisms of provocation of symptoms. Management of the dysfunction that relates to the symptoms and pathology becomes the clinical priority. UCM that may be evident, but does not relate to symptoms, is not a priority of pathology management. However, it may indicate a potential risk for the future (Mottram & Comerford 2008; Roussel et al 2009). The movement control dysfunction can be labelled and classified by the site and direction of UCM and is described in following chapters. Therapeutic exercise within clinical practice is beneficial (Taylor et al 2007). There is evidence that different types of therapeutic exercise are beneficial to many different groups of patients, including those with osteoarthritis of the knee (Brosseau et al 2003; Pelland et al 2004), chronic low back pain (Hayden et al 2005), shoulder pain (Green et al 2003) and chronic neck pain (Kay et al 2005). Different patients appear to need different therapeutic exercises to manage different therapeutic goals. There are indications that specifically targeted and individualised exercise programs are more beneficial than standardised programs (Stuge et al 2004; Taylor et al 2007). The development of rehabilitation strategies directed at correcting the movement faults, identified by evidence-based assessment, rather than developing rehabilitation strategies based on diagnosis of pathology alone, is gaining recognition and acceptance because patients may present with a similar diagnosis of pathology but differing kinematic mechanisms. However, there remain many examples of exercise programs being developed with the ‘one size fits all’ ideology. Most of these programs become ‘protocols’ for ‘core stability’ training or a particular injury such as patellar malalignment, shoulder instability or a post-surgical protocol. Therapeutic exercise can be used to: 1. maintain mobility/flexibility and mobilise restrictions (especially after manual therapy mobilisation or myofascial stretching) 2. manage pain and symptoms (unload or support pain sensitive tissues) 3. control segmental translatatory motion (local muscle system motor control) 4. control aberrant motion – uncontrolled direction or range (global muscle system motor control) 5. recondition and recover from atrophy and tolerate load (increase strength and endurance) 6. cope with speed (produce acceleration and control momentum) 7. train and re-enforce sport-specific skills (skill and coordination) 8. influence mood and sense of wellbeing to assist in the management of behavioural/affective issues. Figure 4.2 incorporates these goals into a non-linear therapeutic exercise paradigm. It is more appropriate and more functional to prescribe therapeutic exercise in parallel combinations based on a clinical assessment and then decide what rehabilitative changes are required and how and when those changes can be implemented. Therapeutic exercise uses movement as a tool to decrease pain, increase joint range and muscle extensibility, to enhance movement performance and to improve wellbeing. The best way to approach therapeutic exercise is to use a clinical reasoning approach. The steps involved in this approach are outlined in Box 4.1. Box 4.2 highlights some key questions that the therapist should be able to answer and justify. These factors should be understood by the therapist prescribing therapeutic exercise and can be explained and supported with the therapeutic exercise plan. Therapeutic exercise needs to address real everyday functional limitations; for example, the inability to bend over when tying shoelaces (due to low back pain or the fear of provoking low back pain), or the inability (due to shoulder pain) to reach up to a cupboard. If a patient with low back pain is unable to actively control movements of the low back, especially flexion control while performing a ‘waiter’s bow’ (Luomajoki 2008), then clinicians should aim an intervention at the neuromuscular impairment underpinning this. Likewise, if a patient with shoulder pain is unable to actively control the scapula during functional movements of reaching with the arm (von Eisenhart-Rothe et al 2005; Tate et al 2008), then clinicians should aim an intervention strategy at regaining this control. There is evidence to support the use of movement retraining to gain an improvement in function (Jull et al 2009; Roussel et al 2009b). Altering movement patterns via exercise can influence clinical signs (Tate et al 2008). However, it is important to establish a clear diagnosis of the movement faults and from this diagnosis develop an appropriate rehabilitation strategy. The therapist requires a sound knowledge of exercise concepts so a patient-specific retraining program can be developed. This is dependent on expertise in the assessment of movement disorders as described in Chapters 1 and 3, and effective clinical reasoning. Chapter 3 has detailed the assessment of the site and direction of UCM. The next stage is regaining control of the UCM and integrating this new movement pattern into normal movement and function. The key goal to effective retraining is to re-establish control of the UCM and regain normal mobility of motion restrictions. The dissociation tests, as described in Chapter 3, are tests of motor control and these establish the site and direction of UCM. If this UCM is related to symptoms, disability, recurrence, risk of injury and performance, a key focus of rehabilitation is regaining the control of movement and changing motor control patterns. The aim is to change the recruitment pattern and actively control movement at the site and in the direction of stability dysfunction. This is a process of sensory-motor reprogramming. • Firstly, position the site of UCM within its neutral training region (as described in Chapter 3) and teach the person how to recruit the appropriate muscles to control a specific direction of movement at this site, while concurrently moving an adjacent joint (above or below) in the same direction (or moving the same segment in a different direction). For example, if the site of the UCM is the lumbar spine, position it in a long shallow mid-range lordosis. If the direction of the UCM is uncontrolled flexion, the therapist instructs the person to control or prevent lumbar flexion while the person flexes forwards independently at the hips, or flexes the thoracic spine independently of any lumbar movement. The person is taught to use whatever feedback helps to monitor and ensure that the lumbar spine does not increase flexion during the retraining exercise. • The motor control retraining emphasis is focused at the joint and in the direction that movement is isometrically controlled (not where the movement is actively performed). That is, for the lumbar flexion UCM control exercise described above, the lumbar extensor stabiliser muscles are actively recruited to isometrically control lumbar flexion during repetitions of the retraining exercise. The flexion movement at the hip or the thoracic spine creates a flexion loading challenge that the lumbar extensor stabiliser muscles have to work against. Throughout the dissociation retraining movements, local and global stability muscles are continually active to control the UCM. • The person is taught to move an adjacent joint above or below in the same direction as the UCM, or same joint (in a different direction of the UCM) only as far as: • A variety of feedback tools can be employed to teach and facilitate the required retraining movement. These can involve visual feedback (watch the movement), visualisation (including imagery), palpation feedback (with the person’s own hands), kinaesthetic feedback (with adhesive tape and skin tension), verbal instruction and verbal correction, and motion monitoring equipment (e.g. pressure biofeedback). Effective cueing is essential for effective retraining. • Repetitions are required to change motor control patterns. Slow, low effort repetitions are encouraged and movement takes place through the range that the UCM can be actively controlled. A general guide is to perform 20–30 slow repetitions or up to 2 minutes of slow repetitions. Occasionally, the body or limb weight has to be unloaded (supported) so that the stability muscles can control the UCM. As unloaded control gets easier, the training is progressed to controlling the normal functional load of the unsupported limbs or trunk. For example, if lumbar flexion is the UCM and it is difficult to retrain, an early retraining option could be to stand with both hands on a chair or bench top and take partial body weight through the hands. Then, with the weight of the trunk partially supported through the hands, the person is instructed to push the hips away from the bench or chair and try to keep the lumbar spine straight and control lumbar flexion (Figure 4.3). When the ability to perform this retraining exercise is well established, it can be progressed to performing the same strategy without any partial support of the trunk through the hands (Figure 4.4) • The focus is on the quality of control. Substitution strategies or UCM must be avoided. Again, patient awareness is paramount. Retraining is focused on training motor control of inefficient muscle groups and establishing efficiency of a corrective movement pattern, not on strengthening the dominant muscles. • The efficiency of control at the UCM is more important initially than the range of motion at the adjacent joint. This movement is practised until it feels familiar and natural. Initially, when these low load exercises ‘feel’ difficult or a high sensation of effort is perceived, then it is likely that slow motor unit or tonic recruitment is inefficient (see Chapter 2). However, when the same low load exercise starts to feel easy and less unnatural, then it is likely that there is better facilitation of slow motor unit recruitment and improved proprioceptive feedback is becoming established. This is a good clinical indicator of improving stability function and motor control efficiency. • The aim of this dissociation retraining is to facilitate the active and eventually automatic recruitment of the local and global stability muscle systems to control movement and by restoring the appropriate use of muscle stiffness to control movement. • With retraining the person should regain awareness of: • This is also linked to improving proprioceptive responses and low threshold recruitment efficiency. • Encourage normal breathing patterns. People with chronic non-specific low back pain may exhibit altered breathing patterns during tests for UCM (Roussel et al 2009c). • The therapist needs to educate the person about the concept of movement retraining and emphasise the importance of cognitive input into the retraining process. This promotes a concept of ‘mindful’ movement. Awareness and concentration is essential. The focus is on retraining the coordination of movement patterns and not the range of movement or the strength of muscle activation. Dissociation exercise is one of many strategies that can be employed in the retraining of movement. The goal is to be mindful of movements during pain-provoking activities. • None of the corrective exercises to improve dynamic stability should produce or provoke any symptoms at all. • The speed of progression and prognosis will depend on many factors, including changes in proprioceptive input, chronic pain patterns with sensitisation and behavioural issues and pathology. • Patients with proprioceptive deficits often:
Retraining strategies for uncontrolled movement
Rehabilitation management and retraining
Management overview
Therapeutic exercise
The site and direction of UCM
Retraining in control of the site and direction of UCM
 need more supervision and correction to ensure retraining exercises are performed properly
need more supervision and correction to ensure retraining exercises are performed properly
 experience a high sensation of effort with low load skills
experience a high sensation of effort with low load skills
 are less aware of substitution strategies (‘cheating’) – they need to rely heavily on ‘external’ feedback
are less aware of substitution strategies (‘cheating’) – they need to rely heavily on ‘external’ feedback
 progress through movement control training more slowly
progress through movement control training more slowly
 do not integrate into automatic unconscious function as easily
do not integrate into automatic unconscious function as easily
 have a higher incidence of recurrence
have a higher incidence of recurrence
 are more likely to require a long-term maintenance program to stay symptom free.
are more likely to require a long-term maintenance program to stay symptom free.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Retraining strategies for uncontrolled movement