Chapter 3 The Scientific Basis for Examination and Classification of Knee Ligament Injuries
CLASSIFICATION SYSTEM FOR KNEE LIGAMENT INJURIES
Many different classification systems for knee ligament injuries have been proposed in the sports medicine literature.20,21,31,32,42 A series of studies conducted by the authors enabled the development of an algorithm for the diagnosis and classification of these injuries based on kinematic and biomechanical data.8,14–17,36–42,55,60 The purpose of this chapter is to summarize these studies and provide the clinician with the proper examination techniques that allow precise diagnosis of abnormal knee motions, subluxations, and ligament injuries.
The classification scheme developed from the authors’ investigations is based on seven concepts:
Critical Points CLASSIFICATION SYSTEM FOR KNEE LIGAMENT INJURIES
Noyes, F. R.; Grood, E. S.: Classification of ligament injuries: why an anterolateral laxity or anteromedial laxity is not a diagnostic entity. Instr Course Lect 36:185–200, 1987.
Purpose of a Classification System
Authors’ Classification System Based on Seven Concepts
In this chapter, the studies presented relate to the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL) and posteromedial structures, the iliotibial band (ITB), and the midlateral capsule. Studies related to the posterolateral structures (fibular collateral ligament [FCL], popliteus muscle-tendon-ligament, and posterolateral capsule) are presented in Chapters 20, Function of the Posterior Cruciate and Posterolateral Ligament Structures, and 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes.
Concept 1: The Final Diagnosis of Knee Ligament Injuries Is Based on the Specific Anatomic Defect Derived from the Abnormal Motion Limit and Joint Subluxation
Concept 2: Ligaments Have Distinct Mechanical Functions to Provide Limits to Tibiofemoral Motions and the Types of Motions That Occur between Opposing Cartilage Surfaces
The ability of ligaments to limit tibiofemoral motion provides the geometric parameters within which the neuromuscular system is able to control the position of the knee during activity. Although focus is placed on the mechanical function of the ligaments and capsular structures, the reader should be cognizant of the potentially important role of ligaments in providing sensory feedback to the neuromuscular system.24,53 Ligaments have three properties that affect their ability to limit joint motion: location of their attachment on the bones, just-taut length, and stiffness.
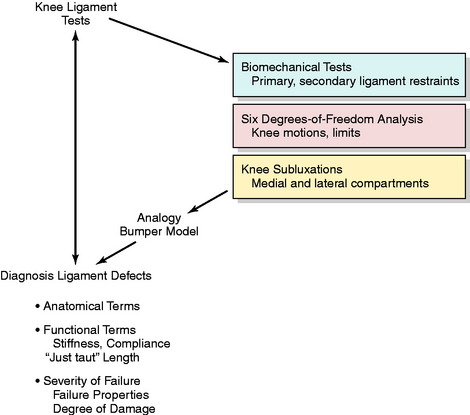
The kinematic and biomechanical concepts required to interpret clinical tests are shown in Figure 3-1. First, the appropriate clinical test must be selected to diagnose a specific ligament structural abnormality. Diagnostic information is obtained based on understanding the primary and secondary ligament restraint system. The results of the tests must be understood and communicated in terms of the six-DOF system that determines the abnormal motion limits. The medial and lateral tibiofemoral compartments are examined separately to determine the different types of subluxation. The final diagnosis of the ligament defect must be made in precise anatomic and functional terms and according to the severity of ligament failure (partial or complete).
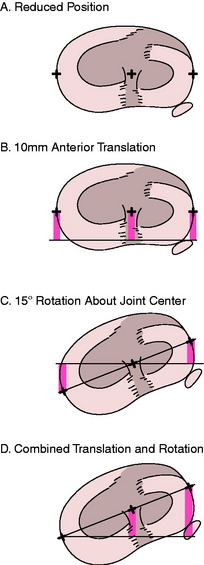
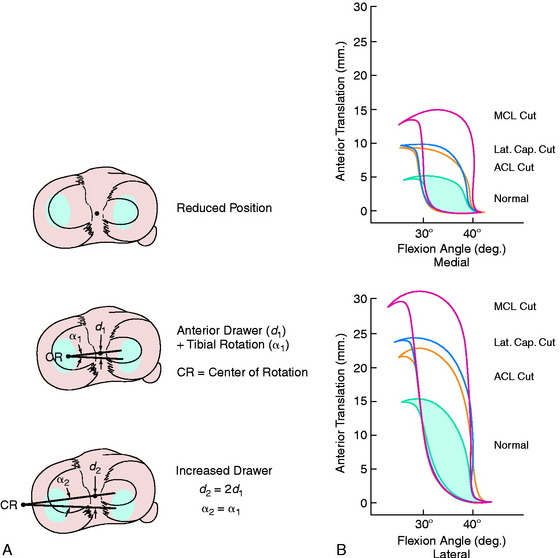
Concept 3: Although There Are Six DOF, the Manual Stress Examinations Are Designed to Test Just One or Two Limits at a Time
Translation of a rigid body (such as the tibia) is described by the motion of an arbitrarily selected point on the body. Typically, the AP translation is described by the motion of a point located midway between the medial and the lateral margins of the tibia. If only translation motions occur, the amount of motion does not depend upon which point is chosen, that is, whether the point is at the center of the knee or at the medial or lateral joint margin. This is because all points will move along parallel paths. However, when rotation and translation motions are combined, the amount of translation does depend upon which point is used. This can be seen by considering the four cases illustrated in Figure 3-2.
Figure 3-2B shows an anterior translation of 10 mm without associated tibial rotation. All points move anteriorly by the same amount. Figure 3-2C shows an internal rotation of 15° about an axis located midway between the spines of the intercondylar eminence. The point on the rotation axis is stationary while the lateral joint margin (edge) moves anteriorly and the medial margin posteriorly (see Fig. 3-2D). The amount of anterior and posterior motion of the points at the joint margin depends upon the amount of rotation and how far away the points are from the rotation axis (center of rotation). This illustrates that when translation is measured in the presence of a concurrent rotation, it is important to know at what point the translation was measured.
Concept 4: Ultimately, the Clinical Examination Must Be Analyzed by a Six-DOF System to Detect Abnormalities
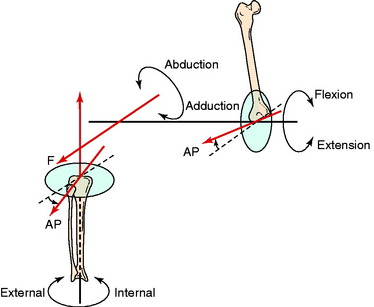
The field of science that describes the motions between objects is known as kinematics. A fundamental aspect of this field is the recognition that six possible motions may occur in three dimensions. Each of the six motions is discrete and separate from the other five motions. The six motions are referred to as degrees of freedom (DOF). The three rotational DOF in the knee joint are shown in Figure 3-3. Each rotation occurs about one axis: flexion-extension, internal-external, and abduction-adduction.
The flexion-extension axis is located in the femur and oriented in a pure medial-lateral direction perpendicular to the femoral sagittal plane. Rotation of the tibia about this axis does not have associated internal-external rotation or abduction-adduction motions.17 Because these motions occur during flexion, the flexion-extension axis shown in Figure 3-3 does not correspond to the functional flexion axis. The functional flexion axis is skewed in the knee and changes its orientation as the knee is flexed. This skewed orientation accounts for the combined motions of flexion, abduction, and tibial rotation.
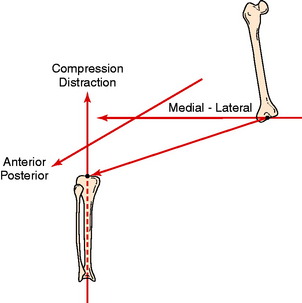
There are three linear DOF in the knee joint referred to as translations. One simple approach to describing translations is to visualize relative sliding between the bones along each of the three rotational axes (Fig. 3-4). The sliding motion along the flexion-extension axis is the medial-lateral translation between the tibia and the femur. The sliding motion along the tibial rotation axis results in joint compression and distraction translation. Sliding motions along the abduction-adduction rotation axis produce AP translations. These are also commonly known as drawer motions.
Therefore, six possible motions can occur in the knee, three rotations and three translations. Three axes are required to explain these six motions, one fixed in each bone, as shown in Figure 3-4. Each axis represents two DOF, one a rotation occurring about the axis and the other a translation.
Concept 5: Together, the Ligaments and Joint Geometry Provide Two Limits (Opposite Directions) for Each DOF
Together, the ligaments and joint geometry provide two limits (opposite directions) for each DOF. All together, there are 12 possible limits of motion of the knee (Table 3-1). Injury to the structures that limit each motion increases joint laxity. The position of the joint at the final limits of motions (reflecting the ligament attachment sites) provides the information required for diagnosis. From a diagnostic standpoint, it would be ideal if each of the 12 limits of motion were controlled by a single ligamentous structure. Differential diagnosis could then be performed by evaluating each of the 12 limits separately. Clearly, this ideal situation does not exist. The ligaments, capsular structures, and joint geometry all work together and each contributes to limiting more than one motion. Thus, the problem of diagnosing knee injuries reduces to determining how to apply individual or combination motions to lengthen primarily a single ligament or capsular structure so that structure can be evaluated independently.
TABLE 3-1 Twelve Limits of Knee Joint Motion
| Motion Limit | Structures Limiting the Motion |
|---|---|
| Flexion | Ligaments, leg and thigh shape, joint compression |
| Extension | Ligaments and joint compression |
| Abduction | Ligaments and lateral joint compression |
| Adduction | Ligaments and medial joint compression |
| Internal rotation | Ligaments and menisci |
| External rotation | Ligaments and menisci |
| Medial translation | Bones (spines interlocking with femoral condyles) and ligaments (to prevent distraction) |
| Lateral translation | Bones (spines interlocking with femoral condyles) and ligaments (to prevent distraction) |
| Anterior translation* | Ligaments |
| Posterior translation* | Ligaments |
| Joint distraction | Ligaments |
| Joint compression | Bone, menisci, and cartilage |
* Menisci, joint compressive effects after injury to primary restraint.
The ability to isolate each structure is the key to differential diagnosis of individual ligament injuries. The isolation of a structure is accomplished by placing the knee at the proper joint position (specifically, knee flexion angle and tibial rotation position) before the clinical stress test is performed. For example, the abduction (valgus) stress test is performed both in full extension and at 20° to 30° of flexion. In the flexed position, the posterior capsule becomes slack, which allows the examiner to primarily load the MCL and midmedial capsule. The evaluation of ACL function is performed at 20° of knee flexion56 as opposed to the 90° position29 commonly used many years ago because the 20° position more often results in increased anterior subluxation because secondary restraints are more slack and less able to block this motion. Diagnosis of an injury to a specific ligament is performed at a joint position at which other structures are the most lax and least able to block the abnormal subluxation from the ligament injury. The lax secondary restraints allow an increase in joint motion before they become taut and resist further joint motion. Thus, isolating a ligament so its integrity may be individually tested requires placing the knee in a position in which other supporting structures are slack.
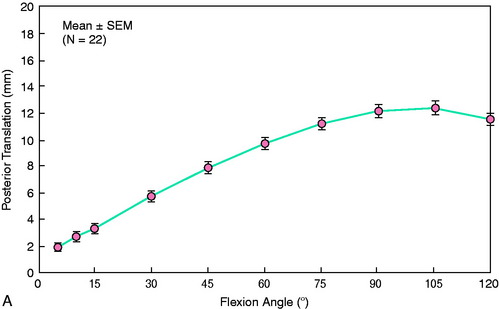
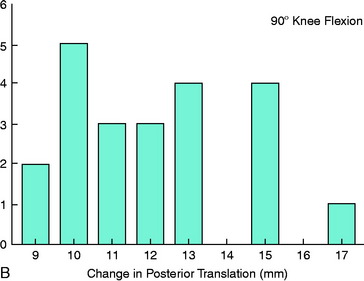
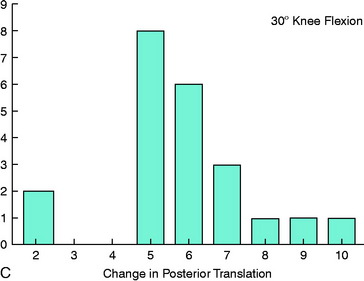
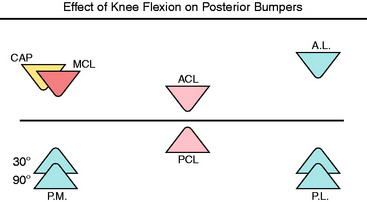
Another example of the importance of selecting the joint position for clinical tests is the diagnosis of PCL injury. Figure 3-5 shows the amount of increased posterior tibial translation that occurs when the PCL is removed.10,16,17 The increase in posterior translation is two to three times greater at 90° of flexion than at 20° of flexion. This phenomenon is easily understood using a bumper model analogy in which the amount of joint motion after a ligament is injured depends on the role and function of the remaining ligaments that must ultimately limit the joint motion (Fig. 3-6). Thus, the increase in joint motion that occurs when a ligament is injured reflects the amount of additional joint motion required before the remaining intact ligaments become stretched and are able to limit further motion.
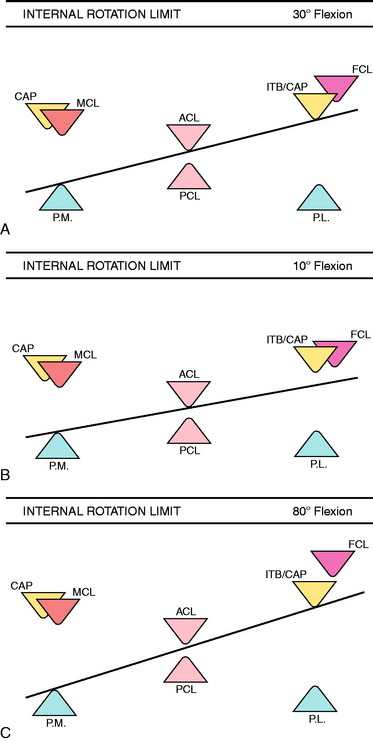
Figure 3-7 illustrates the limits to internal tibial rotation in the knee joint.16 At 30° flexion (see Fig. 3-7A), the limits to internal rotation are provided by posteromedial structures, lateral structures, and the ACL all working together. Sectioning either the ACL or the lateral structures produces a small increase in internal rotation. When both of these structures are cut together, a larger increase in internal rotation occurs. The further limit to internal rotation is the FCL, based upon its anatomy.
The ACL dominates at flexion angles less than 30°, whereas the lateral structures dominate at flexion angles greater than 30°. This can be explained by considering the changes that occur in ligament slackness with flexion and extension. As the knee is extended past 20°, the amount of AP translation decreases owing to reduction in the combined slackness of both cruciate ligaments. This brings these bumpers closer together. The posteromedial capsule (PMC) also tightens, moving its bumper anteriorly. This combination (see Fig. 3-7B) results in a decreased role of the anterolateral structures because the tibia can no longer rotate to the point where they become taut.
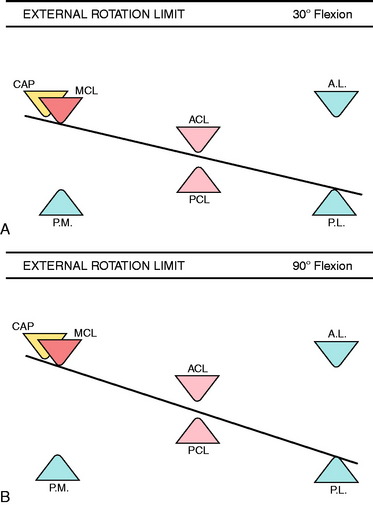
Figure 3-8 illustrates the limits to external rotation. At 30° flexion, external rotation is limited only by the extra-articular restraints. On the lateral side, this includes all of the posterolateral structures, which act as a unit. Large increases in rotation do not occur until all structures are cut. At 90° flexion, the posterior capsule is slack and the PCL blocks significant increases in external rotation when the posterolateral structures are sectioned. In laboratory studies, external rotation increases an average of only 5.3° ± 2.6° when all of the posterolateral structures are sectioned and the PCL is intact. When the PCL is also sectioned, a large additional increase in external rotation occurs, ranging from 15° to 20°.
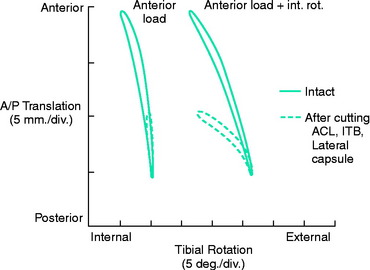
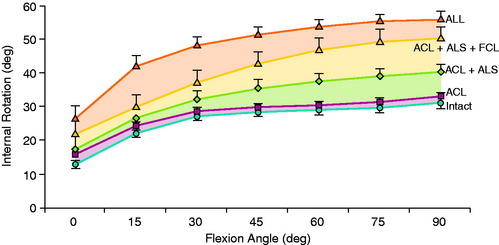
An example of the changes in motion limits in ACL ruptures is shown in Figure 3-9. In cadaver knees, cutting the ACL causes an abnormal increase in both anterior tibial translation and internal tibial rotation.8 The increase in anterior tibial translation is the primary abnormality, because it increases 100% while there is a small increase in internal rotation (approximately 15%). Cutting the ACL alone produced a small but significant increase in internal rotation, greatest at 0° and 15° (Fig. 3-10). Subsequently, sectioning the ITB and lateral capsule produced statistically significant increases at 30° and greater.
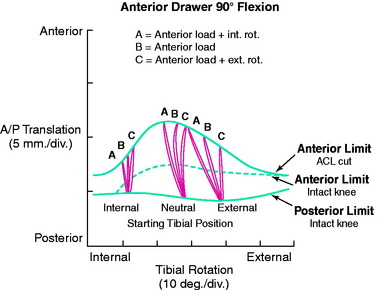
The amount of anterior tibial translation induced during anterior drawer testing is dependent upon the amount of internal or external tibial rotation applied at the beginning of the test (Fig. 3-11). The instrumented knee joint is shown for measuring rotations and translation motions during the clinical examination in Figure 3-12. This is because rotation tightens the extra-articular secondary restraints. The greatest amount of anterior or posterior tibial translation will be produced when the tibial is not forcibly rotated internally or externally, tightening extra-articular structures, during the clinical test. If the tibia is internally or externally rotated prior to the start of testing, the amount of tibial translation elicited will be smaller. Thus, the clinician controls the amount of translation both by the initial rotational position of the tibia and by the amount of rotation imposed during the test. There is considerable variation in examination techniques of clinicians that makes all of the clinical tests highly subjective and qualitative, as is discussed.
The pivot shift12 and flexion-rotation44 drawer (Fig. 3-13) tests involve a complex set of tibial rotations and AP translations. At the beginning of the flexion-rotation drawer test, the lower extremity is simply supported against gravity (Fig. 3-14, position A). After ligament sectioning, both anterior tibial translation and internal rotation increase as the femur drops back and externally rotates into a subluxated position.42 This position is accentuated as the tibia is lifted anteriorly (see Fig. 3-14, position B). At approximately 30° of flexion, the tibia is pushed posteriorly, reducing the tibia into a normal relationship with the femur (see Fig. 3-14, position C). This is the limit of posterior tibial translation resisted primarily by the PCL. From position C to position A, the knee is extended to produce the subluxated position again.
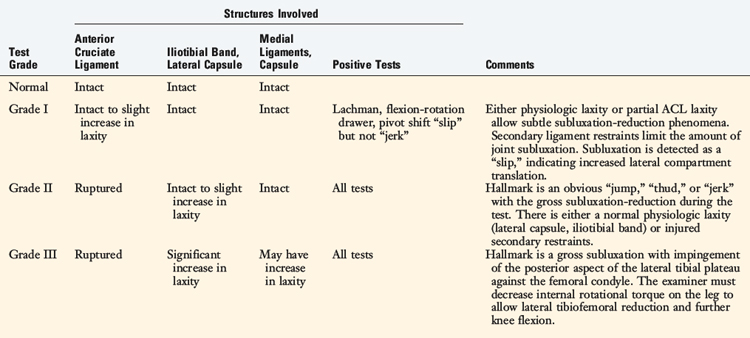
The pivot shift and flexion-rotation drawer tests are graded only in qualitative terms because it is not possible to determine accurately the actual amount of internal tibial rotation or anterior translation elicited. A fully positive pivot shift test (grade III) indicates a gross subluxation of the lateral tibiofemoral articulation along with an increased anterior displacement of the medial tibial plateau (Table 3-2). The amount of anterior subluxation elicited is indicative of rupture to the ACL and laxity to the secondary extra-articular restraints. The lateral tibial plateau demonstrates the greater subluxation in a positive pivot shift test, indicating that the lateral restraints (ITB, lateral capsule) are not functionally tight. This does not mean that these restraints are injured because a physiologic slackness of the ITB tibiofemoral attachments is normal at the knee flexion position used in this test. These attachments are tightest at knee flexion angles of 45° and higher. Therefore, the majority of knees with an isolated ACL tear will have a positive pivot shift phenomenon.
In knees with a grade III pivot shift test, the amount of anterior tibial subluxation is so great that the posterior margin of the lateral tibial plateau impinges against the lateral femoral condyle and blocks further knee flexion during the test. The examiner must add both a maximal anterior force and an internal tibial rotation force to determine whether the maximum subluxation position can be reached. In revision ACL reconstructions, a combined intra-articular graft and extra-articular ITB surgical approach is often considered, as is discussed.34
Concept 6: Rotatory Subluxations Are Characterized by the Separate Compartment Translations That Occur to the Medial and Lateral Tibial Plateaus during the Clinical Test
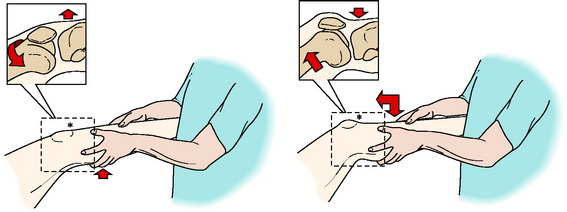
A simple concept may assist in explaining the abnormal motions that occur after ACL rupture: rotatory subluxations can be classified according to the amount of anterior and posterior translation of each tibiofemoral compartment. Figure 3-15A shows a Lachman test performed on a knee in which the combined motions of anterior tibial translation and internal tibial rotation occur about a medially located rotation axis. In this example, only planar motion occurs; the ACL rupture doubles the amount of anterior tibial translation and slightly increases internal tibial rotation. The rotation axis shifts medially. The ratio of tibial translation to degrees of internal tibial rotation determines how far medially the axis of rotation shifts.
The abnormalities in tibial rotation and translation are easily expressed in terms of the different amounts of anterior translation that occur to the medial and lateral compartments (see Fig. 3-15B) in biomechanical tests. During the clinical tests, the clinician may qualitatively palpate and observe the anterior or posterior translation of each tibial plateau. The AP translation of each plateau is characterized instead of defining the individual components of translation, rotation, and rotation axis location that all lead to the anterior subluxation. The combined effect of the rotation and translation determines the translation of the medial and lateral tibiofemoral compartments.
The type of rotatory subluxations that occur depends on both the ligament injury and the knee flexion position. The subluxations of the medial and lateral compartment are usually recorded at two knee flexion positions, such as 20° and 90°. To be described later is the dial test for posterolateral injuries, in which the examiner determines whether increases in external tibial rotation reflect anteromedial or posterolateral tibial subluxations. It should be noted that rotatory subluxations are historically based on increases in tibial internal or external rotation and in only a few studies have the actual medial and lateral tibial subluxations in an AP direction been determined.16,45 There are complex rotatory subluxations involving increases in translation, but in opposite directions of both the medial and the lateral compartments with combined medial and lateral ligament injuries.
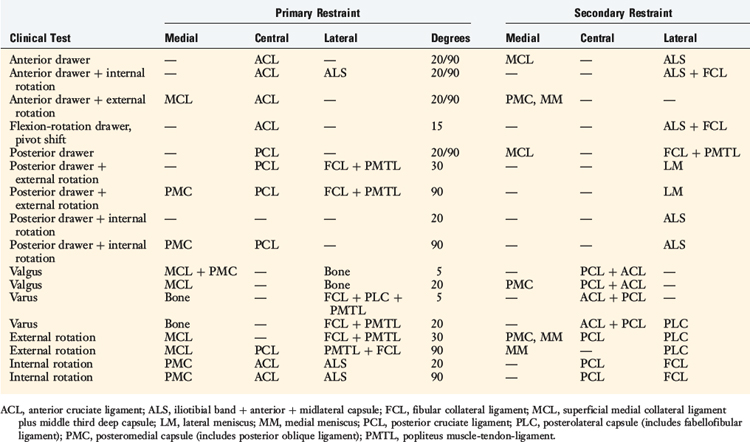
Concept 7: The Damage to Each Ligament and Capsular Structure Is Diagnosed Using Tests in Which the Primary and Secondary Ligament Restraints Have Been Experimentally Determined
Tears to the ACL and injury to the extra-articular ligamentous and capsular structures may be diagnosed using the Lachman, pivot shift, and flexion-rotation drawer tests. These tests provide the basic signs that allow the clinician to determine which structures are injured based on abnormal motion limits and resultant joint subluxations. The tests are performed in knee flexion positions in which the secondary restraints are unable to resist abnormal motions so that maximum displacement (subluxation) of the joint is produced. Table 3-3 provides a general summary of the primary and secondary restraints for the major tests used in the clinical examination. Later in this chapter, the specific restraining function of the ligaments is discussed in detail.
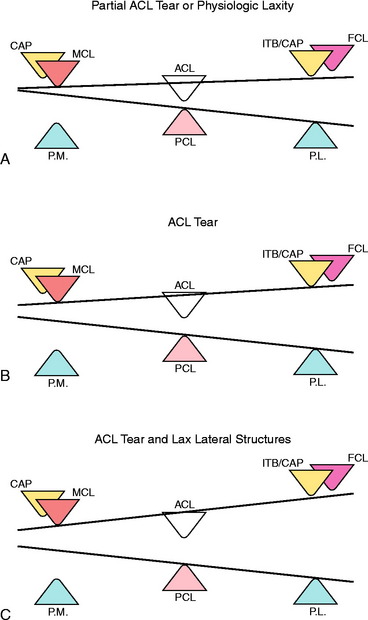
The qualitative grading of the pivot shift phenomenon is illustrated in Figure 3-16 to explain how ligament structures resist combined tibiofemoral motions. The cruciate ligaments are represented by a set of central bumpers that limit the amount of AP translation. There are also medial and lateral sets of bumpers that resist medial and lateral tibiofemoral compartment translations. For the medial and lateral bumpers, different ligament structures commonly work together as systems to provide the resistance. The bumpers represent not the anatomic position of the ligament structures, but rather a visual schematic to show the final restraints to tibial motion, summarizing the effect of the ligaments, menisci, and capsular structures. The tension-retraining effect of the ligaments is replaced by an opposite mechanism, a compressive bumper.
In diagnosing abnormal knee motion limits, the Lachman test involves primarily tibial translation without significant tibial rotation, testing the central bumper represented by the ACL. A bumper model representation of a partial ACL tear or an ACL-deficient knee with tight medial and lateral extra-articular restraints that limit the amount of anterior tibial translation is shown in Figure 3-16A. The amount of central and lateral tibial translation is only slightly increased. The bumper model illustrates how the anterior restraints limit motion during the flexion-rotation drawer test, which allows the maximal anterior excursion of the medial and lateral tibiofemoral compartments. In this knee, the pivot shift test is qualitatively listed as a grade I.
The most common type of anterior subluxation that occurs after an ACL rupture is shown in Figure 3-16B. The center of rotation shifts medially outside the knee joint, with a resultant increase in translation to both the medial and the lateral compartments, with the anterior subluxation of the lateral compartment being the greatest. The anatomic structures include the ACL and the lateral extra-articular restraints. In this knee, the pivot shift test is qualitatively listed as a grade II.
A knee with gross anterior subluxation is represented in Figure 3-16C. There is increased translation and subluxation to both the medial and the lateral compartments and the rotation axis shifts even further medially outside the knee joint. The pivot shift test is listed as a grade III, indicative of gross subluxation with impingement of the posterior aspect of the tibia against the femoral condyle. Partial damage to the medial ligamentous structures may be present.
LIGAMENTOUS RESTRAINTS TO AP TRANSLATION
In a series of biomechanical cadaveric experiments,8 the ranked order of the importance of each knee ligament and capsular structure in resisting the clinical anterior and posterior drawer tests was determined, providing the primary and secondary restraints to specific knee motions. The ranked order was based on the force provided by each ligament in resisting AP translation.
Prior to these experiments, investigators performed studies in which selective sectioning of ligaments was conducted and the increases in anterior or posterior tibial displacement were measured.5,6,11,13,19,28,29,47,50, For example, the displacement test was done by applying a force on an intact knee, cutting a ligament, repeating the test, and measuring the increase in displacement. One problem with this experimental design is that the increase in displacement is dependent on the order in which the ligaments are sectioned. If this order is altered, the measured increase in displacement will change. Therefore, it is not possible to define the function of a single ligament in a precise manner. In addition, the amount of residual joint displacement after ligament sectioning is dependent on the just-taut length of the remaining ligaments, which varies between physiologic “tight” and “loose” knee joints.
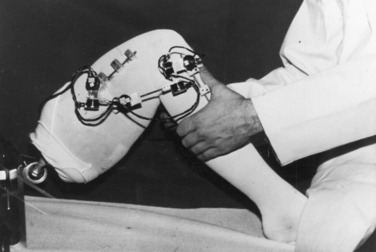
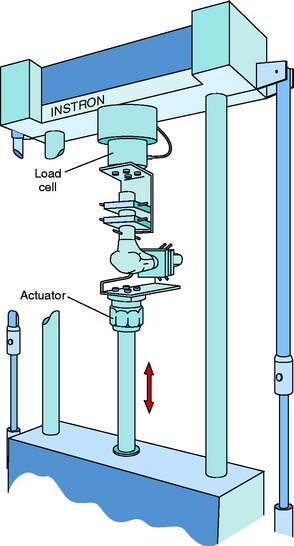
Fourteen cadaver knees were tested from donors aged 18 to 65 years (mean, 42 yr). The knee specimens were mounted in an Instron Model 1321 biaxial servocontrolled electrohydraulic testing system (Fig. 3-17). A pair of grips was used for the femur and tibia that allowed for their precise position to be adjusted. First, the femur was secured with its shaft aligned along the axis of the load cell. The tibia was placed horizontally, with its weight supported by the lower grip. The output of the load cell was adjusted to zero to compensate for the weight of the upper grip and femur. The tibia was placed in a rotated position halfway between its limits of internal and external rotation. The output of the load cell was monitored while the tibia was secured in order to avoid pre-loading the ligaments. Single-plane anterior and posterior drawer tests were conducted by causing the actuator to move up and down without rotation. This is a constrained test in which coupled tibial rotation is purposely blocked. Specific details regarding the tests and data acquisition and statistical analyses are described in detail elsewhere.8
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree