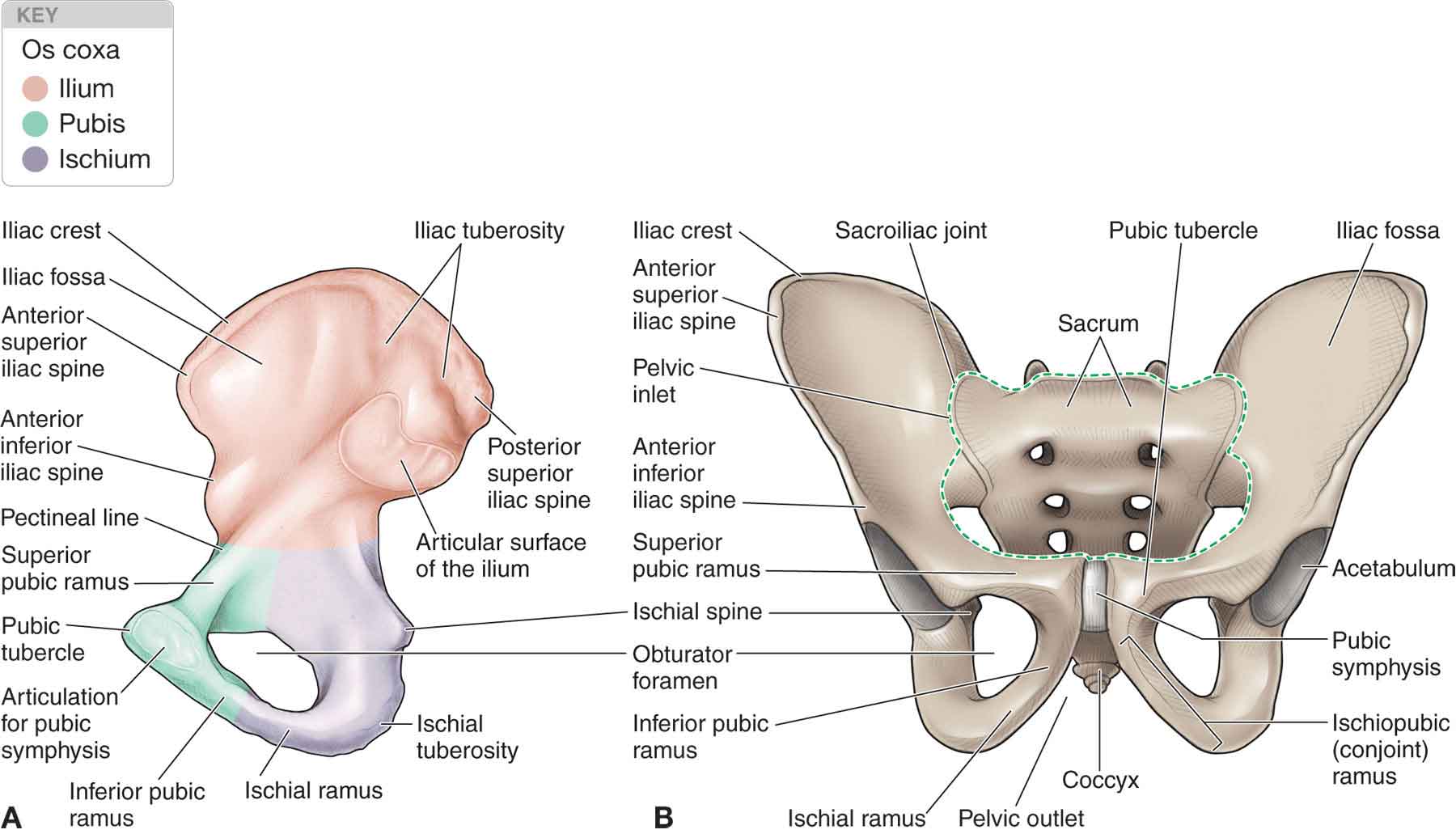
The sacroiliac joint (SIJ) serves as the supporting base of the spine and as the point of intersection between the spinal and the lower extremity joints. The SIJ is the least understood and, therefore, one of the most controversial and interesting areas of the spine. Determining a diagnosis in this region is complicated by the biomechanics of the SIJ and its relationships with the surrounding joints, including the hip, pubic symphysis, and lumbar spine. Grieve1 has proposed that the SIJ, together with the other areas of the spine that serve as transitional areas, is of prime importance in understanding vertebral joint problems. This level of importance is perhaps surprising because isolated pelvic impairments are rare. However, findings for SIJ dysfunction appear to be common, and the literature is replete with intervention techniques aimed at correcting pelvic dysfunctions.2–11 This may be explained by the fact that, in addition to being able to produce pain on its own, the SIJ often can refer pain.12 The level of interest surrounding this joint dates back to the Middle Ages, a time when the burning of witches was commonplace. It was noticed after these burnings that three of the bones were not destroyed: a large triangular bone and two very small bones. It can only be assumed that some degree of significance was given to the large triangular bone as it was deemed a sacred bone and was thus called the sacrum. It is unclear what significance was given to the two smaller bones, the sesamoid bones of the great toe. Despite these illustrious beginnings for the sacrum, it was not until approximately 100 years ago that significant attention was applied to the study of pelvic anatomy and function, and its relationship to low back and pelvic pain. At the start of the 20th century, SIJ strain was thought to be the most common cause of sciatica.13 Then, in 1934, Mixter and Barr14 reported that sciatica could be caused by a prolapsed intervertebral disk, and the interest in the SIJ as a source of sciatica dwindled. Since then, there have been periods when the joint has been blamed for almost all low back and leg pain, and times when it has only been considered a problem during pregnancy. It is now generally accepted that approximately 13% (95% CI: 9–26%) of patients with persistent low back pain have the origin of pain confirmed as the SIJ.15 Anatomically, the SIJ is a large diarthrodial joint that connects the spine with the pelvis (Fig. 29-1) and which serves as a central base through which forces are transmitted both directly and indirectly. The structure of the pelvis and its surrounding tissues has evolved in conjunction with the evolutionary changes in human gait. Three bones comprise the SIJ: two innominates and the sacrum. FIGURE 29-1 The pelvis. (Reproduced, with permission, from Chapter 6. Headache & Facial Pain. In: Greenberg DA, Aminoff MJ, Simon RP. eds. Clinical Neurology, 8e. New York, NY: McGraw-Hill; 2012.)
CHAPTER 29
The Sacroiliac Joint
OVERVIEW
ANATOMY
Sacrum
The sacrum (Fig. 29-1), a strong and triangular bone located between the two innominates, provides stability to this area and transmits the weight of the body from the mobile vertebral column to the pelvic region. Evolutionary changes have resulted in an increased size of the sacrum to accommodate the increased osseous attachment of the gluteus maximus muscle, and to facilitate the increased compression produced in a bipedal stance.11 The sacrum base is above and anterior, and its apex below and posterior (Fig. 29-1). This differs from nonhuman mammals in which the sacral base is horizontal, and the lumbar spine is kyphotic.11 Five centra fuse to form the central part of the sacrum, which contains remnants of the intervertebral disks enclosed by bone. The sacrum has four pairs of pelvic sacral foramina for transmission of the anterior (ventral) primary rami of the sacral nerves and four pairs of posterior (dorsal) sacral foramina for transmission of the posterior (dorsal) primary rami.
The transverse processes of the first sacral vertebra fuse with the costal elements to form the ala and the lateral crests (see Fig. 29-1). The ala of the sacrum forms the superolateral portions of the base. The superior articular processes of the sacrum (Fig. 29-1), which are concave and oriented posteromedially, extend upward from the base to articulate with the inferior articular processes of the fifth lumbar vertebra.
On the posterior (dorsal) surface of the sacrum is a midline ridge of bone called the median sacral crest, which represents the fusion of the sacral spinous processes of S1 to S4. Projecting posteriorly from this crest are four spinous tubercles. The fused laminae of S1 to S5, which are located lateral to the median sacral crest, form the intermediate sacral crest.
The sacral hiatus exhibits bilateral downward projections that are called the sacral cornua. These projections represent the inferior articular processes of the fifth sacral vertebra and are connected to the coccyx via the intercornual ligaments. On the inferolateral borders of the sacrum, approximately 2 cm to either side of the sacral hiatus, are the inferior lateral angles (ILAs). The triangular sacral canal houses the cauda equina. In addition to the more commonly considered bones and joints are those of the coccygeal spine. The coccyx, which is variable in size, consists of three to five vertebral units that are usually fused, with the exception of the first segment, which articulates with the distal end of the sacrum, and is referred to as the sacrococcygeal joint.16 In general, the posterior (dorsal) surface of the coccyx is convex, so that its inferior aspect slopes anteriorly.
Innominates
The ilium, ischium, and pubic bone fuse at the acetabulum to form each innominate (Fig. 29-1). The ilium of each of the two innominates articulate with the sacrum, forming the SIJ, and the pubic bone of each of the innominates articulate with each other at the symphysis pubis. The ilia have undergone significant adaptations in response to bipedalism in such a way that the bone has twisted so that the lateral aspect is now directed anteriorly, and the gluteus medius and minimus muscles have migrated anteriorly with a resultant change in their function.11
Sacroiliac Joint
The articulating surfaces of this joint differ, with the joint surface of the ilium formed from fibrocartilage and the sacral surface formed from hyaline cartilage.17 The SIJ is in part synovial (25% of its surface) and in part syndesmosis, and so between the sacral and iliac auricular surfaces, the SIJ is deemed a synovial articulation or diarthrosis.18,19
The inverted, L-shaped, auricular articular surface of the sacrum (Fig. 29-1) is surrounded entirely by the costal elements of the first three sacral segments. The short (superior) arm of this L-shape lies in a craniocaudal plane, within the first sacral segment, and corresponds to the depth of the sacrum (see Fig. 29-1). It is widest superiorly and anteriorly. The long (inferior) arm of the L-shape lies in an anteroposterior (A-P) plane, within the second and third sacral segments, and represents the length of the sacrum from top to bottom. It is widest inferiorly and posteriorly. There are large irregularities on each articular surface20 that are approximately, though not exactly, reciprocal, with the sacral contours being generally deeper.21,22 In addition to the larger irregularities, there are smaller horizontal crests and hollows that run anteroposteriorly. The sacral articular surface is wedge shaped in its upper portion, formed by the first sacral segment and half of the second. Below this, the joint surfaces run nearly vertically and then diverge somewhat, making a flare which tends to prevent the sacrum from sliding upward between ilia.22
The morphology varies in size, shape, and contour from side to side, and between individuals and changes with aging.23 In fact, variations in the SIJ morphology are so common that they have been classified as type A, being less vertical than type B, and type C as an asymmetric mixture of types A and B.5 Each of these variants can alter the function of the pelvis and its influence on the lumbar lordosis.24
The articulating surfaces of the joint respond differently to the aging process, with early degenerative changes occurring on the iliac surface rather than on both surfaces of the joint simultaneously.27 Other changes associated with aging include the development of intraarticular fibrous connections.28 However, even with severe degenerative changes, the SIJ rarely fuses.18
The SIJ can be the site of manifestation for several disease processes, including SI tuberculosis, spondyloarthropathy (ankylosing spondylitis), and crystal and pyogenic arthropathies.
Joint Capsule
The SIJ capsule, consisting of two layers, is extensive and very strong. It attaches to both articular margins of the joint and is thickened inferiorly.
Ligaments
Like other synovial joints, the SIJ is reinforced by ligaments, but the ligaments of the SIJ are some of the strongest and toughest ligaments of the body.
Anterior Sacroiliac (Articular)
The anterior sacral ligament (Fig. 29-2) is an anteroinferior thickening of the fibrous capsule, which is relatively weak and thin compared to the rest of the SI ligaments. The ligament extends between the anterior and inferior borders of the iliac auricular surface and the anterior border of the sacral auricular surface.18 The anterior sacral ligament is better developed near the arcuate line and the posterior-inferior iliac spine (PIIS), where it connects the third sacral segment to the lateral side of the preauricular sulcus.
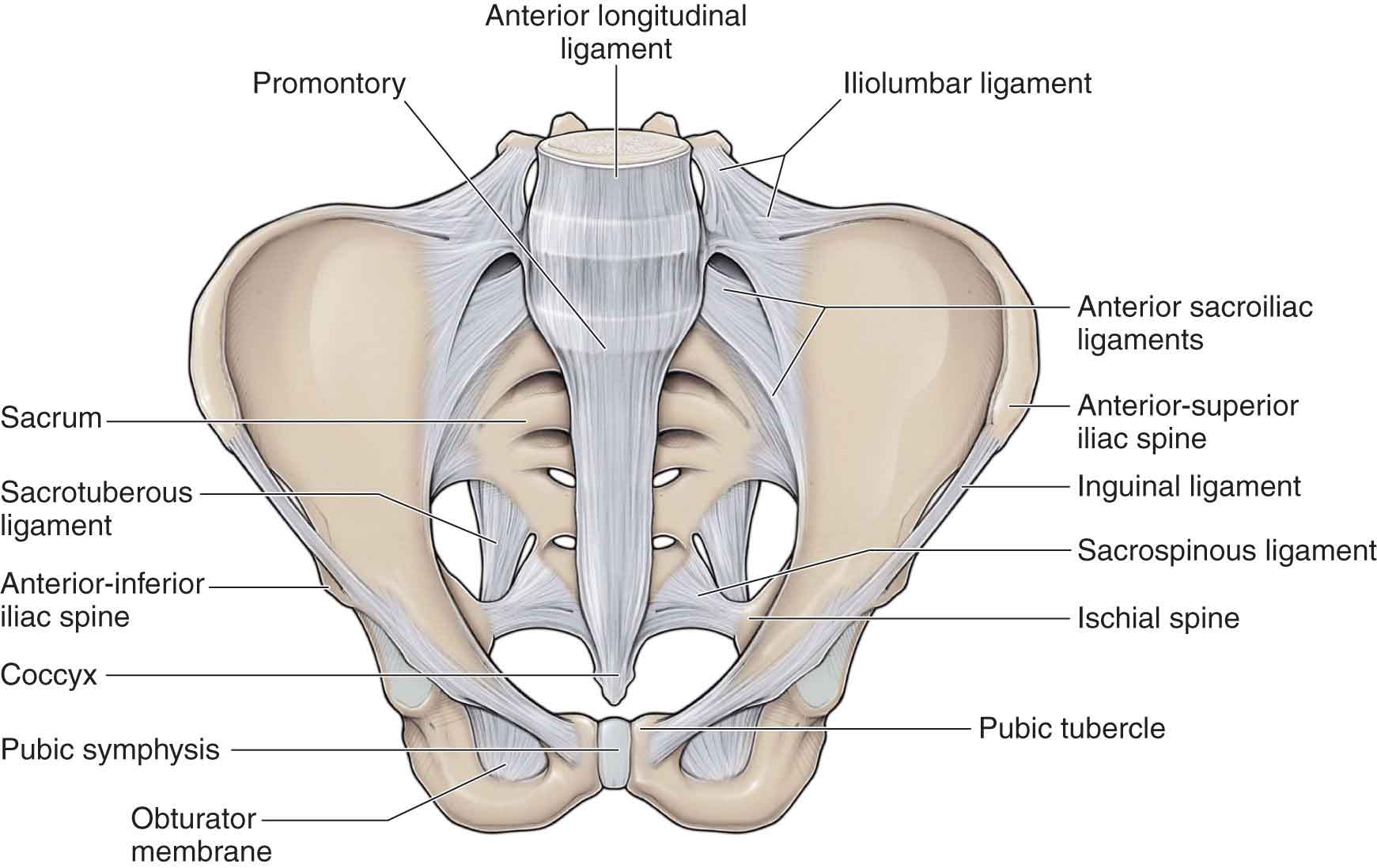
FIGURE 29-2 Anterior ligaments.
Because of its thinness, this ligament is often injured and can be a source of pain. It can be palpated at Baer’s SI point*29 and can be stressed using the anterior distraction and posterior compression pain provocation tests (see later).
*Baer’s SI point has been described as being on a line from the umbilicus to the ASIS, 5 cm from the umbilicus.
Interosseous Sacroiliac (Articular)
This is a strong, short ligament located deep to the posterior (dorsal) SI ligament, and it forms the major connection between the sacrum and the innominate, filling the irregular space posterosuperior to the joint between the lateral sacral crest and the iliac tuberosity (Fig. 29-3).30 The deep portion sends fibers cranially and caudally from behind the auricular depressions. The superficial portion is a fibrous sheet connecting the superior (cranial) and posterior (dorsal) margins of the sacrum to the ilium, forming a layer that limits direct palpation of the SIJ. The interosseous SI ligament functions to resist anterior and inferior movement of the sacrum.
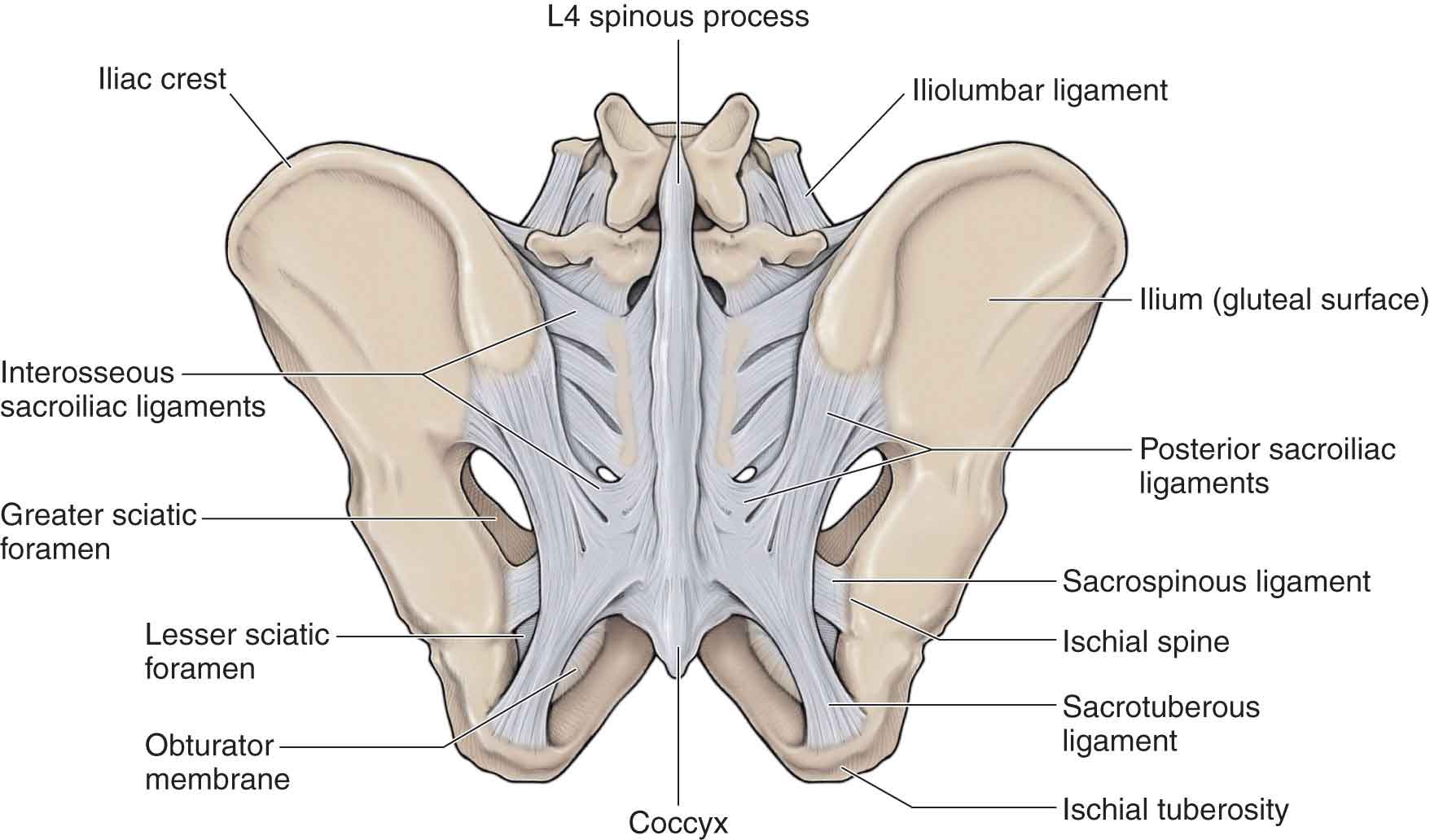
FIGURE 29-3 Posterior ligaments.
Posterior (Dorsal) Sacroiliac (Articular)
The posterior (dorsal) SI ligament or long ligament (see Fig. 29-3), which is easily palpable in the area directly caudal to the posterior-superior iliac spine (PSIS), connects the PSIS (and a small part of the iliac crest) with the lateral crest of the third and fourth segments of the sacrum.31 This is a very tough and strong ligament. The fibers of this ligament are multidirectional and blend laterally with the sacrotuberous ligament. It also has attachments medially to the erector spinae32 and multifidus muscles33 and the thoracodorsal fascia. Thus, contractions of the various muscles that attach to this ligament can result in the tightening of the ligament.
Directly caudal to the PSIS, the ligament is so solid and stout that one can easily think a bony structure is being palpated. What complicates matters is the fact that the area overlying the ligament is a frequent source of pain.34
The lateral expansion of the long ligament in the region directly caudal to the PSIS varies between 15 and 30 mm. The length, measured between the PSIS and the third and fourth sacral segments, varies between 42 and 75 mm. The lateral part of the posterior (dorsal) ligament is continuous with fibers passing between ischial tuberosity and iliac bone.
At the superior (cranial) aspect, the posterior (dorsal) ligament is attached to the PSIS and the adjacent part of the ilium, at the inferior (caudal) side to the lateral crest of the third and fourth, and occasionally to the fifth, sacral segments.32
Nutation (anterior motion) of the sacrum appears to slacken the posterior (dorsal) ligament, whereas counternutation (posterior motion) tautens the ligament.32
Sacrotuberous (Extraarticular)
This ligament (see Fig. 29-3) is composed of three large fibrous bands, broadly attached by its base to the PSIS, the lateral sacrum, and partly blended with the posterior (dorsal) SI ligament. Its oblique, lateral fibers descend and attach to the medial margin of the ischial tuberosity, spanning the piriformis muscle from which it receives some fibers. The medial fibers, running anteroinferior and laterally, have an attachment to the transverse tubercles of S3, S4, and S5, and the lateral margin of the coccyx. To the posterior surface of the sacrotuberous ligament are attached the lowest fibers of the gluteus maximus and the piriformis, the contraction of which produces increased tension in the ligament.35 Superficial fibers on the inferior aspect of the ligament can continue into the tendon of the biceps femoris.
In addition to stabilizing against nutation of the sacrum, the sacrotuberous ligament also counteracts against the posterior (dorsal) and superior (cranial) migration of the sacral apex during weight bearing.36,37
Sacrospinous (Extraarticular)
Thinner than the sacrotuberous ligament, this triangular-shaped ligament extends from the ischial spine to the lateral margins of the sacrum and coccyx, and also laterally to the spine of the ischium (see Fig. 29-3). The ligament runs anterior (deep) to the sacrotuberous ligament to which it blends and then attaches to the capsule of the SIJ.33
The sacrotuberous and sacrospinous ligaments, which convert the greater and lesser sciatic notches into the greater and lesser foramen respectively, oppose forward tilting of the sacrum on the innominates during weight bearing of the vertebral column.
Iliolumbar (Indirect)
The anatomy of the iliolumbar ligament (Fig. 29-2) is described in Chapter 28.
Pubic Symphysis
The pubic symphysis is classified as a symphysis because it has no synovial tissue or fluid, and it contains a fibrocartilaginous lamina or disk (Fig. 29-2). The bone surfaces of the joint are covered with hyaline cartilage but are kept apart by the presence of the disk.
The following are the supporting ligaments of this joint21:
 Superior pubic ligament, a thick fibrous band.
Superior pubic ligament, a thick fibrous band.
 Inferior arcuate pubic ligament, which attaches to the inferior pubic rami bilaterally and blends with the articular disk.
Inferior arcuate pubic ligament, which attaches to the inferior pubic rami bilaterally and blends with the articular disk.
 Posterior pubic ligament, a membranous structure that blends with the adjacent periosteum.
Posterior pubic ligament, a membranous structure that blends with the adjacent periosteum.
 Anterior ligament, a very thick band that contains both transverse and oblique fibers.
Anterior ligament, a very thick band that contains both transverse and oblique fibers.
The pubic symphysis is a common source of groin pain, particularly in athletes (see section “Groin Pain”).
Muscles
Lee11 lists 35 muscles that attach directly to the sacrum or innominate, or both (Table 29-1). A muscle attaching to bone has the potential for moving that bone, although the degree of potential varies. Rather than producing movement at the SIJ, the muscles around the pelvis are more likely involved directly or indirectly in helping to provide stability to the joint.
TABLE 29-1 | Muscles That Attach to the Sacrum, Ilium, or Both |
Latissimus dorsi Erector spinae Semimembranosus Semitendinosus Biceps femoris Sartorius Inferior gamellus Multifidus Obturator internus Obturator externus Piriformis Tensor fascia lata External oblique Internal oblique Transversus abdominis Rectus abdominis Pyramidalis Gluteus minimus Gluteus medius Gluteus maximus Quadratus femoris Superior gemellus Gracilis Iliacus Adductor magnus Rectus femoris Quadratus lumborum Pectineus Psoas minor Adductor brevis Adductor longus Levator ani Sphincter urethrae Superficial transverse perineal ischiocavernosus Coccygeus |
Piriformis
This muscle (see Chapter 19) arises from the anterior aspect of the S2, S3, and S4 segments of the sacrum; the capsule of the SIJ; and the sacrotuberous ligament. It exits from the pelvis via the greater sciatic foramen, before attaching to the upper border of the greater trochanter of the femur.
The piriformis primarily functions to produce external rotation and abduction of the femur, but is also thought to function as an internal rotator and abductor of the hip if the hip joint is flexed beyond 90 degrees. It also helps to stabilize the SIJ, although too much tension from it can restrict the motion of this joint.38 The piriformis has been implicated as the source for a number of conditions in this area, including the following two
Transversus Abdominis
The transversus abdominis (TrA) is the deepest abdominal muscle and arises from the lateral one-third of the inguinal ligament, the anterior two-thirds of the inner lip of the iliac crest, the lateral raphe of the thoracolumbar fascia, and the inner surface of the lower six costal cartilages, interdigitating with the costal fibers of the diaphragm.11 For a detailed description of the anatomy and function of the TrA, refer to Chapter 28. Although the TrA does not cross the SIJ directly, it can affect the stiffness of the pelvis through its direct anterior attachments to the ilium, as well as its attachments to the middle layer and the deep laminae of the posterior layer of the thoracodorsal fascia.46,47
Multifidus
The anatomy of the multifidus muscle is described in Chapter 28. Some of the deepest fibers of the multifidus attach to the capsules of the zygapophyseal joints48 and are located close to the centers of rotation of spinal motion. They connect adjacent vertebrae at appropriate angles, and their geometry remains relatively constant through a range of postures, thereby enhancing spinal stability.49
Erector Spinae
For a detailed description of the anatomy of the erector spinae, refer to Chapter 28. Through its extending effect on the spine and its substantial sacral attachments, the erector spinae might be thought to promote sacral nutation, although this has not been proven.
Gluteus Maximus
This is one of the strongest muscles in the body (see Chapter 19). It arises from the posterior gluteal line of the innominate, the posterior aspect of the lower lateral sacrum and coccyx, the aponeurosis of erector spinae muscle, the superficial laminae of the posterior thoracodorsal fascia, and the fascia covering the gluteus medius muscle, before attaching to the gluteal tuberosity. In the pelvis, the gluteus maximus blends with the ipsilateral multifidus, through the raphe of the thoracodorsal fascia,33 and the contralateral latissimus dorsi, through the superficial laminae of the thoracodorsal fascia.50 Some of its fibers attach to the sacrotuberous ligament. Tension in the sacrotuberous ligament increases when these fibers contract.51
Iliacus
This muscle arises from the iliac fossa (see Chapter 19), the iliac crest, the anterior SI ligament, the inferior fibers of the iliolumbar ligament,52 and the lateral aspect of the sacrum. As it travels distally, its fibers merge with the lateral aspect of the psoas major tendon to form the iliopsoas, which continues onto the lesser trochanter of the femur, sending some fibers to the hip joint capsule as it passes.
Long Head of the Biceps Femoris
The long head of the biceps femoris originates from the ischial tuberosity and sacrotuberous ligament. In addition to functioning as a hip extensor and knee flexor (see Chapter 19, the long head of the biceps femoris, due to its connections to the sacrotuberous ligament, may also have a proprioceptive role during activities such as gait.
Pelvic Floor Musculature
The term “pelvic floor muscles” primarily refers to the levator ani, a muscle group composed of the pubococcygeus, puborectalis, and iliococcygeus. The levator ani muscles join the coccygeus muscles to complete the pelvic floor. The pelvic floor muscles work in a coordinated manner to increase intraabdominal pressure, provide rectal support during defecation, inhibit bladder activity, help support the pelvic organs, and assist in lumbopelvic stability.53
Levator Ani. The levator ani (Fig. 29-4) originates anteriorly from the pelvic surface of the pubis, posteriorly from the inner surface of the ischial spine, and from the obturator fascia. It inserts into the front and sides of the coccyx, to the sides of the rectum, and into the perineal body. The levator ani forms the floor of the pelvic cavity, functions to constrict the lower end of the rectum and vagina, and can also be activated during forced expiration.
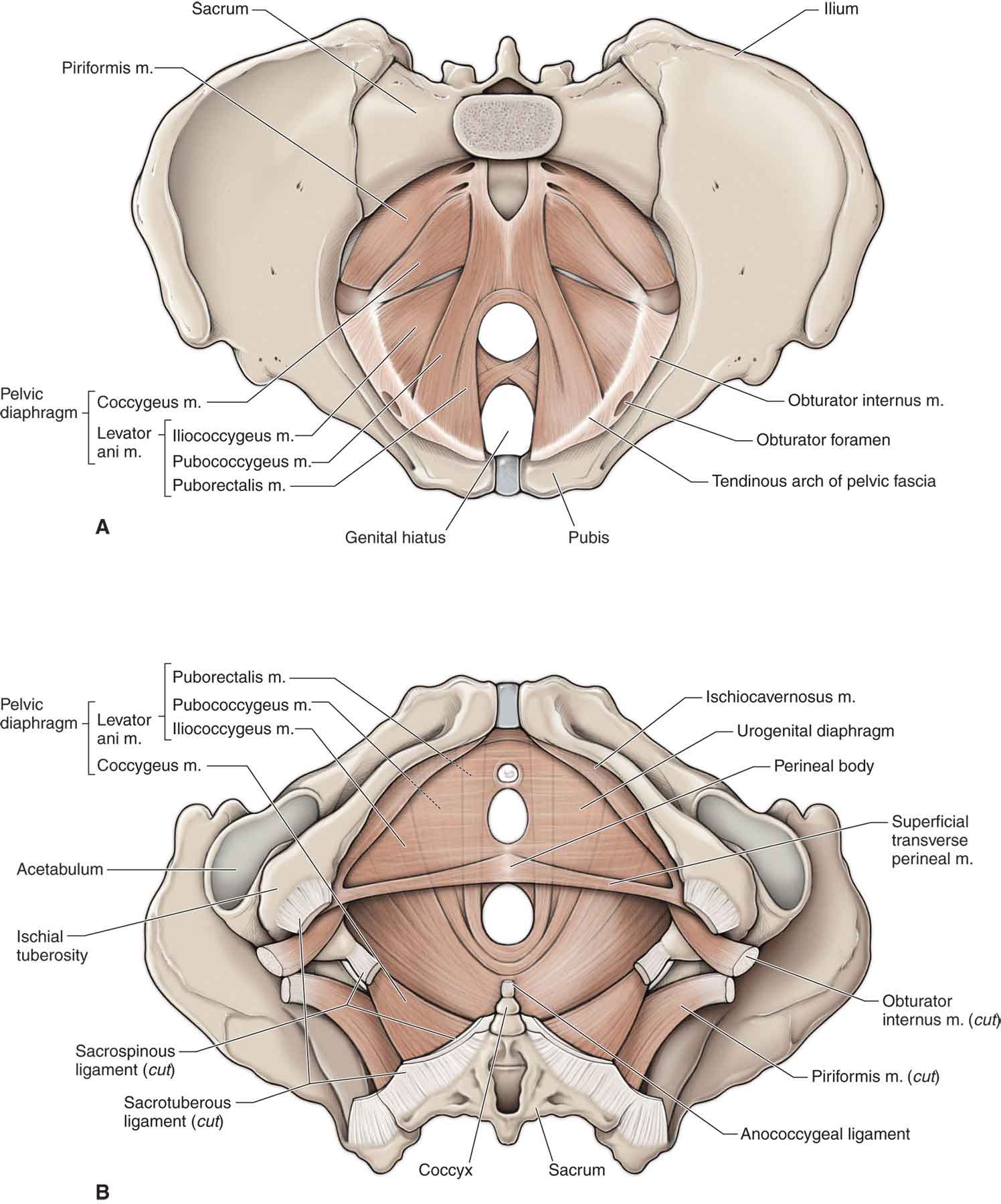
FIGURE 29-4 Pelvic floor muscles. (Reproduced, with permission, from Chapter 12. Pelvis and Perineum. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The muscle, which consists of anterior, intermediate, and posterior fibers, is innervated by the muscular branches of the pudendal plexus.
Anterior Fibers. The anterior fibers insert into the perineal body, comprise the levator prostatae or sphincter vaginae, and form a sling around the prostate or vagina.
Intermediate Fibers
 Puborectalis. The puborectalis (see Fig. 29-4) originates at the pubis and forms a sling around the junction of the rectum and the anal canal. The muscle pulls the anorectal junction anteriorly, assisting the external sphincter in anal closure.
Puborectalis. The puborectalis (see Fig. 29-4) originates at the pubis and forms a sling around the junction of the rectum and the anal canal. The muscle pulls the anorectal junction anteriorly, assisting the external sphincter in anal closure.
 Pubococcygeus. The pubococcygeal muscle (see Fig. 29-4) arises from the pubis and its superior ramus and passes posteriorly to insert into the anococcygeal body between the coccyx and the anal canal. The muscle functions to pull the coccyx forward. It also serves to elevate the pelvic organs and compress the rectum and vagina.
Pubococcygeus. The pubococcygeal muscle (see Fig. 29-4) arises from the pubis and its superior ramus and passes posteriorly to insert into the anococcygeal body between the coccyx and the anal canal. The muscle functions to pull the coccyx forward. It also serves to elevate the pelvic organs and compress the rectum and vagina.
 Posterior Fibers. The iliococcygeal muscle (see Fig. 29-4) arises from the arcus tendineus and ischial spine and inserts onto the last segment of the coccyx and the anococcygeal body. The muscle functions to pull the coccyx from side to side and to elevate the rectum.
Posterior Fibers. The iliococcygeal muscle (see Fig. 29-4) arises from the arcus tendineus and ischial spine and inserts onto the last segment of the coccyx and the anococcygeal body. The muscle functions to pull the coccyx from side to side and to elevate the rectum.
 Levator Plate. The pubococcygeal muscle and the iliococcygeal muscle unite posterior to the anorectal junction to form the levator plate, which inserts into the coccyx.
Levator Plate. The pubococcygeal muscle and the iliococcygeal muscle unite posterior to the anorectal junction to form the levator plate, which inserts into the coccyx.
 Coccygeus. This muscle (Fig. 29-4) arises from the pelvic surface of the ischial spine and sacrospinous ligament and inserts on the coccyx margin and side of the lowest segment of the sacrum. Supplied by the muscular branches of the pudendal plexus, the coccygeus functions to pull forward and support the coccyx. In addition, the coccygeus muscle provides support for the pelvic contents and the SIJ.
Coccygeus. This muscle (Fig. 29-4) arises from the pelvic surface of the ischial spine and sacrospinous ligament and inserts on the coccyx margin and side of the lowest segment of the sacrum. Supplied by the muscular branches of the pudendal plexus, the coccygeus functions to pull forward and support the coccyx. In addition, the coccygeus muscle provides support for the pelvic contents and the SIJ.
Neurology
It remains unclear precisely how the anterior and posterior aspects of the SIJ in humans are innervated, although the anterior portion of the joint likely receives innervation from the posterior rami of the L2 to S2 roots.54 Contribution from these root levels is highly variable and may differ among the joints of given individuals.55 Additional innervation to the anterior joint may arise directly from the obturator nerve, superior gluteal nerve, or lumbosacral trunk.22,56 The posterior portion of the joint is likely innervated by the posterior rami of L3 to S3, with a particular contribution from S1 and S2.57 An additional autonomic component of the joint’s innervation further increases the complexity of its neural supply and likely adds to the variability of pain referral patterns from this area.56,58
The current reference standard for confirming pain stemming from the SIJ is fluoroscopically guided, contrast-enhanced, intraarticular anesthetic blocks.59 Using this method, the SIJ has been identified in 10% to 27% of patients with low back pain as a source of their primary pain.15,60,61 Mechanical pain resulting from SIJ dysfunction may manifest as sacral pain but may also refer pain distally. For example, SIJ problems can refer pain to the iliac fossa, the buttock, the groin, the superior lateral and posterior thigh, and rarely below the knee.62 In general, SIJ pain is characterized by unilateral pain below the level of L5, in the absence of midline pain, whereas irritation of a spinal nerve may cause radicular symptoms below the knee.63 Pubic symphysis dysfunction typically results in localized pain, or groin pain, which is aggravated by activities involving the hip adductor or rectus abdominis muscles.64 However, studies have shown that using evidence of pain referral patterns, or evidence of groin pain is neither sensitive nor specific for SIJ dysfunction.65
Pain also may be referred to the sacrum from a distant structure, including the contralateral sacrospinalis muscle,66 the ipsilateral interspinous ligaments of L3 to S2,67 and the L4 to L5 facet joints.68 In addition, it is well established that dysfunctional pelvic floor muscles can contribute to the symptoms of interstitial cystitis and the so-called urethral syndrome, which is urgency frequency with or without chronic pelvic pain.69–71
BIOMECHANICS
Motions at the neighboring lumbar spine predominantly occur around the sagittal plane and comprise flexion and extension, whereas the motions occurring at the hip occur in three planes and include the one motion that the lumbar spine does not tolerate well, that is, rotation. Thus, the pelvic area must function to transfer the loads generated by body weight and gravity during standing, walking, sitting, and other functional tasks.72 To date, there is very little agreement, either among or even within disciplines, about how the structures of the pelvis achieve this. For many decades, it was thought that the SIJ was immobile due to the close fitting nature of the articular surfaces. Research has now shown that mobility of the SIJ is not only possible,73–76 but also essential for shock absorption during weight-bearing activities.77 However, the range of motion (ROM) in the SIJ is small, less than 4 degrees of rotation and up to 1.6 mm of translation.74,78 Of interest, is the fact that one study79 found no difference in available ROM between the symptomatic and asymptomatic sides.
It is likely that the movement of the pelvis is in the nature of deformations and slight gliding motions around a number of undefined axes, with the joints of the pelvic ring deforming in response to body weight and ground reaction forces. The amplitude of this motion likely varies among individuals. Motion at the SIJ is facilitated by several features, including the following:
 The fibrocartilaginous surfaces of the innominate facets, which are deformable, especially during weight bearing, when the surfaces are forced together.
The fibrocartilaginous surfaces of the innominate facets, which are deformable, especially during weight bearing, when the surfaces are forced together.
 The pubic symphysis—if the innominates are moving at the SIJ, then they must also be moving at their anterior junction, which would allow for an immediate, and almost perfect, reciprocal motion.
The pubic symphysis—if the innominates are moving at the SIJ, then they must also be moving at their anterior junction, which would allow for an immediate, and almost perfect, reciprocal motion.
No manual diagnostic tests have shown reliability for determining how much an individual’s SIJ is moving in either symptomatic or asymptomatic subjects. In contrast to Sturesson’s study,78 when Doppler imaging testing has been used to measure stiffness (or laxity) of the SIJ in subjects with and without pelvic pain, it has been shown that asymmetry of stiffness between sides correlated with the symptomatic individual.80–82 These studies have shown that within the same subject, asymptomatic individuals have similar values for the left and right SIJs, whereas individuals with unilateral posterior pelvic girdle pain had different stiffness values for the left and right sides. Theoretically, when assessing SIJ mobility, a dysfunction at the SIJ can manifest as one of the two types of asymmetries
 If one of the SIJs is hypermobile, the amplitude of motion is increased asymmetrically, and the resistance to motion is decreased on the dysfunctional side.
If one of the SIJs is hypermobile, the amplitude of motion is increased asymmetrically, and the resistance to motion is decreased on the dysfunctional side.
 If one of the SIJs is hypomobile, the amplitude of motion is asymmetrically reduced, and the resistance to motion is increased on the dysfunctional side.
If one of the SIJs is hypomobile, the amplitude of motion is asymmetrically reduced, and the resistance to motion is increased on the dysfunctional side.
Thus, the current trend is to focus more on the symmetry, or asymmetry, of the motions palpated or observed.
Anatomical research,83–85 initiated to determine the source of low back pain, has demonstrated that alterations in the pattern of muscular contraction and the timing of specific muscle activation differ between healthy subjects and those demonstrating symptoms. Furthermore, studies86 have shown that the strength and endurance of the trunk muscles are important in determining the muscle capacity of individuals. This research has led to theories about the force- and form-closure mechanisms of joints and how stability is necessary at joints for effective load transfer. Based on this knowledge, functional tests of load transfer through the pelvic girdle have been developed87–89 together with a number of treatment protocols.90–92 This approach has three physical components (form closure, force closure, and motor control) and one psychological component (emotions).
In upright positions, the SIJ is subjected to considerable shear force as the mass of the upper body must be transferred to the lower limbs via the ilia.93,94 The body has two mechanisms to overcome this shear force: one dependent on the shape and structure of the joint surfaces of the SIJs (form closure), which is wedge shaped with a high coefficient of friction, and the other mechanism involving generation of compressive forces across the SIJ via muscle contraction (force closure).94
Form Closure
Form closure refers to a state of stability within the pelvic mechanism, with the degree of stability dependent on its anatomy, with no need for extra forces to maintain the stable state of the system.85 The following anatomic structures are proposed to assist with form closure:
 The congruity of the articular surfaces and the friction coefficient of the articular cartilage. Both the coarseness of the cartilage and the complementary grooves and ridges increase the friction coefficient and thus contribute to form closure by resisting against horizontal and vertical translations.22 In infants, the joint surfaces are very planar, but between the ages of 11 and 15 years, the characteristic ridges and humps that make up the mature sacrum begin to form. By the third decade, the superficial layers of the fibrocartilage are fibrillated, and crevice formation and erosion has begun. By the fourth and fifth decades, the articular surfaces increase irregularity and coarseness and the wedging is complete.18
The congruity of the articular surfaces and the friction coefficient of the articular cartilage. Both the coarseness of the cartilage and the complementary grooves and ridges increase the friction coefficient and thus contribute to form closure by resisting against horizontal and vertical translations.22 In infants, the joint surfaces are very planar, but between the ages of 11 and 15 years, the characteristic ridges and humps that make up the mature sacrum begin to form. By the third decade, the superficial layers of the fibrocartilage are fibrillated, and crevice formation and erosion has begun. By the fourth and fifth decades, the articular surfaces increase irregularity and coarseness and the wedging is complete.18
 The integrity of the ligaments.
The integrity of the ligaments.
 The shape of the closely fitting joint surfaces.
The shape of the closely fitting joint surfaces.
According to current research, when the sacrum nutates, or flexes, relative to the innominate (Fig. 29-5), or when the innominate posteriorly rotates relative to the sacrum, the greatest number of ligaments, particularly the interosseous and posterior (dorsal) ligaments, are tightened at the SIJ.85,95,96 These latter ligaments lie posterior to the joint and approximate the posterior iliac bones when placed under tension.95 Thus, nutation of the sacrum can be described as the close packed position, or self-locking mechanism, for the SIJ and is, therefore, the most effective position for transferring high loads. This position somewhat conveniently produces a position of lumbar lordosis, which is advocated in many interventions for the lumbar spine.
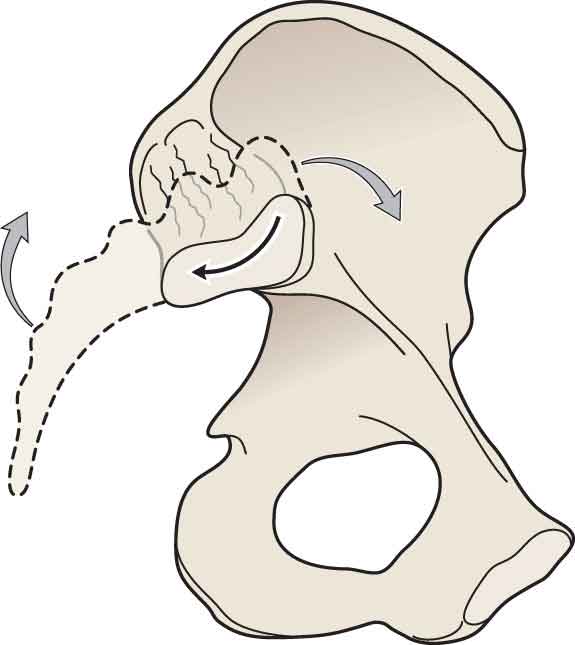
FIGURE 29-5 Sacral nutation.
Just as nutation of the sacrum enhances the self-locking mechanism, counternutation of the sacrum (Fig. 29-6), which occurs during activities, such as the end range of forward bending, sacral sitting, long sitting, and hip hyperextension, reduces the self-locking mechanism.95. This position results in a loss of the lumbar lordosis and an increase in intervertebral disk pressure (see Chapter 28).
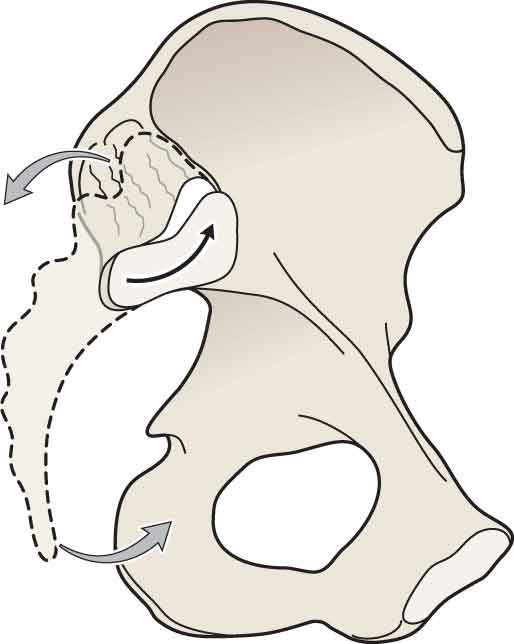
FIGURE 29-6 Sacral counternutation.
Using forward bending at the waist as an example, a combination of anterior and outward rotation of both innominates results in the approximation and superior motion of both PSISs, while the sacrum nutates (Table 29-2). After approximately 60 degrees of forward bending, the innominates continue to rotate anteriorly, but the sacrum no longer nutates.84 If the sacrum remains nutated throughout the forward bending, the SIJ remains compressed and stable. However, if the sacrum is forced to counternutate earlier in the range, as in individuals with tight hamstrings, less compression occurs, thereby increasing the reliance on dynamic stabilization provided by muscles and thus making the SIJ more vulnerable to injury.84
TABLE 29-2 | Lumbar Motions and Sacroiliac Motions |
Lumbar Motion | Innominate Motion | Sacrum Motion |
Flexion | Anterior rotation | Nutation, then counternutation |
Extension | Slight posterior rotation | Nutation |
Rotation | Ipsilateral: Posterior rotation Contralateral: Anterior rotation | Nutates ipsilaterally |
Side bending | Ipsilateral: Anterior rotation Contralateral: Posterior rotation | Ipsilateral: Side bends ipsilaterally Contralateral: Side bends contralaterally |
Force Closure
Force closure requires intrinsic and extrinsic forces to keep the SIJ stable.85 These dynamic forces involve the neurological and myofascial systems and gravity. Together, these components produce a self-locking mechanism for the SIJ. Optimum force closure requires the application of just the right amount of force at just the right time, which in turn requires a motor control system that can predict the timing of the load and prepare the system appropriately. The degree of force closure depends on the capability of an individual’s form closure and the various loading conditions (e.g., speed, duration, magnitude, and predictability).97
In a kinetic analysis of the pelvic girdle, Vleeming et al.50,95 identified a number of muscles that resist translational forces and which are specifically important to the force-closure mechanism: the erector spinae, gluteus maximus, latissimus dorsi, and biceps femoris (see Chapter 28). Two other muscle groups, an “inner muscle unit” and an “outer muscle unit” also play an important role.84,86,92 The inner muscle unit consists of the following:
 Transversus abdominis (TrA). A study by Richardson et al.98 found that contraction of the TrA significantly decreases the laxity of the SIJ, and that this decrease in laxity is larger than that caused by a bracing action using all the lateral abdominal muscles. Theoretically, contraction of the TrA produces a force that approximates the ilia anteriorly.98
Transversus abdominis (TrA). A study by Richardson et al.98 found that contraction of the TrA significantly decreases the laxity of the SIJ, and that this decrease in laxity is larger than that caused by a bracing action using all the lateral abdominal muscles. Theoretically, contraction of the TrA produces a force that approximates the ilia anteriorly.98
 The muscles of the pelvic floor. Hemborg et al.99 have demonstrated that the pelvic floor muscles coactivate with the TrA during lifting tasks.
The muscles of the pelvic floor. Hemborg et al.99 have demonstrated that the pelvic floor muscles coactivate with the TrA during lifting tasks.
 Multifidus. Studies100–102 have reported that the deep fibers of the multifidus become inhibited and reduced in size in individuals with low back and pelvic girdle pain.
Multifidus. Studies100–102 have reported that the deep fibers of the multifidus become inhibited and reduced in size in individuals with low back and pelvic girdle pain.
The outer muscle unit consists of four systems: the posterior oblique system (latissimus dorsi, gluteus maximus, and thoracolumbar fascia), the deep longitudinal system (erector spinae, deep lamina of the thoracolumbar fascia, sacrotuberous ligament, and biceps femoris), the anterior oblique system (external and internal oblique, contralateral adductors of the thigh, and the intervening anterior abdominal fascia), and the lateral system (gluteus medius–minimus and contralateral adductors of the thigh). The outer muscle unit is proposed to contribute to the force-closure mechanism in the following manner84:
 Posterior oblique system. The gluteus maximus (see Chapter 19), which blends with the thoracodorsal fascia, and the contralateral latissimus dorsi contribute to force closure of the SIJ posteriorly by approximating the posterior aspects of the innominates. This oblique system is a significant contributor to load transference through the pelvic girdle during the rotational activities of gait.
Posterior oblique system. The gluteus maximus (see Chapter 19), which blends with the thoracodorsal fascia, and the contralateral latissimus dorsi contribute to force closure of the SIJ posteriorly by approximating the posterior aspects of the innominates. This oblique system is a significant contributor to load transference through the pelvic girdle during the rotational activities of gait.
 Deep longitudinal system. This system serves to counteract any anterior shear or sacral nutation forces as well as to facilitate compression through the SIJs. As mentioned in the anatomy section, the long head of the biceps femoris muscle controls the degree of nutation via its connections to the sacrotuberous ligaments.36
Deep longitudinal system. This system serves to counteract any anterior shear or sacral nutation forces as well as to facilitate compression through the SIJs. As mentioned in the anatomy section, the long head of the biceps femoris muscle controls the degree of nutation via its connections to the sacrotuberous ligaments.36
 Anterior oblique system. The oblique abdominals, acting as phasic muscles, initiate movements.92and are involved in all movements of the trunk and upper and lower extremities, except when the legs are crossed.103
Anterior oblique system. The oblique abdominals, acting as phasic muscles, initiate movements.92and are involved in all movements of the trunk and upper and lower extremities, except when the legs are crossed.103
 Lateral system. The lateral system functions to stabilize the pelvic girdle on the femoral head during gait through a coordinated action.
Lateral system. The lateral system functions to stabilize the pelvic girdle on the femoral head during gait through a coordinated action.
The sacrococcygeal joint has a limited amount of movement in flexion and extension, ranging from approximately 5–15 degrees in either direction.105 A posterior rotation (flexion) motion occurs when moving from a standing to a sitting position, which is thought to enable optimal force absorption in the seated position.16 The reverse occurs when moving from a seated to a standing position.
As alluded to earlier, the sacral positions that correspond to poor sacral biomechanics are very similar to those lumbar spine positions that are unfavorable to spinal stability. Conversely, the positions that enhance sacral stability also enhance lumbar spine stability. As a result, there has been much confusion amongst disciplines when determining whether the SIJ or lumbar spine is the cause of the patient’s symptoms. For example, consider the prone on elbows position (see Chapter 28), which nutates the sacrum and increases the lordosis of the lumbar spine. If a patient with either a sacral dysfunction or an intervertebral disk herniation is asked to adopt this position, the symptoms would likely decrease.
EXAMINATION
Most investigators agree that no single test can be used to confirm the diagnosis of SIJ dysfunction because of the complexity of the anatomy and biomechanics and its proximity to other symptom-provoking structures.
Diagnostic physical examination tests that are commonly used to determine a diagnosis include55
 direct tenderness;
direct tenderness;
 soft-tissue examination for zones of hyperirritability and tissue texture changes;
soft-tissue examination for zones of hyperirritability and tissue texture changes;
 evaluation of referral zones;
evaluation of referral zones;
 associated fascial or musculotendinous restrictions;
associated fascial or musculotendinous restrictions;
 abnormal regional length–strength muscle relationships;
abnormal regional length–strength muscle relationships;
 postural analysis;
postural analysis;
 true leg length and functional leg-length determination;
true leg length and functional leg-length determination;
 static and dynamic osseous landmark examinations; and
static and dynamic osseous landmark examinations; and
 provocative testing including traditional orthopaedic tests, motion demand tests, and ligament tension tests.
provocative testing including traditional orthopaedic tests, motion demand tests, and ligament tension tests.
Although traditionally assumed to be reliable and diagnostically useful, none of these tests has ever been validated against an independent criterion standard.55 As a consequence, controversy exists about which group of tests is the best.
Under the premise that a relationship exists between pelvic asymmetry and low back pain, orthopaedic, osteopathic, and physical therapy tests promote the use of pain provocation (symptom based) tests and static (positional) or dynamic (motion or functional) tests.1,10,38,84,106–109
The use of static tests has been questioned,110–114 as, although Cibulka et al.115 found the results from these tests reliable, Levangie114 found a weak association between standing PSIS asymmetry and low back pain, at least in selected groups. The problems with static testing are
 the high degree of anatomical variability in this area;
the high degree of anatomical variability in this area;
 determining whether the asymmetry noted is normal or abnormal;
determining whether the asymmetry noted is normal or abnormal;
 determining which side is abnormal; and
determining which side is abnormal; and
 determining whether the asymmetry is too asymmetric or not asymmetric enough. For example, if the right innominate is anteriorly rotated, compared with the left, is it rotated too much, too little, or just the right amount compared with its starting position? Because the starting position is not known, the degree of rotation cannot be assessed.
determining whether the asymmetry is too asymmetric or not asymmetric enough. For example, if the right innominate is anteriorly rotated, compared with the left, is it rotated too much, too little, or just the right amount compared with its starting position? Because the starting position is not known, the degree of rotation cannot be assessed.
The dynamic tests do not fare much better. Dreyfuss et al.55 reported 20% positive findings in one or more of the dynamic (motion or functional) tests in a group of asymptomatic people. The major problem with the dynamic tests is that SIJ motion is small, so it is highly implausible to be able to detect it. An example of a dynamic test is the standing flexion test, which has frequently been used to analyze SIJ mobility and to determine the side of the impairment. The test is performed as follows: Each PSIS is palpated with the thumb placed under it caudally. The patient then bends forward at the waist. Provided there is no impairment in the SIJ or the lower lumbar spine, as the patient bends forward, both thumbs should move superiorly (cranially). If one SIJ joint is “blocked,” it moves upward further in relation to the other side.113 Thus far, reliability studies of the standing flexion test show that it lacks sufficient diagnostic power.113,116,117 This shortfall may be because the compression of the joints caused by the sacral nutation in the early to midranges of forward flexion likely limits movement of the SIJ.118
Some studies have reported that pain provocation tests have a good interexaminer reliability,113,119 but they have not been found reliable by others.15,116 This is likely because the pain provocation tests have only been found reliable in identifying SIJ dysfunction in certain populations, such as patients with posterior pelvic pain during or following pregnancy.120 Laslett et al.121 reported that adequate sensitivity (0.88) and specificity (0.78) can be achieved using a clinical prediction rule involving two positive tests of distraction, thigh thrust, compression, and sacral thrust (see Pain Provocation Tests in Special Tests section). The diagnostic process begins with the two tests that have the highest positive predictive value and specificity (distraction test) and negative predictive value and sensitivity (thigh thrust) for identifying SIJ pathology. If these two tests both recreate the patient’s SIJ pain (positive), further tests are not indicated. If one or neither of the two tests are positive, the clinician follows the algorithm in Figure 29-7.

FIGURE 29-7 Decision-making algorithm for the SIJ.
As several recent studies have found improved interrater reliability in the diagnosis of low back pain when using a combination of physical examination procedures as opposed to a single model approach,15,55,113,122,123 it would be logical to assume that a similar approach would work with the SIJ.
Ideally, the diagnosis needs to be based on the results of a thorough biomechanical examination that includes an assessment of load transfer, and pain provocation. Patients with failed load transfer through the pelvic girdle often present with inappropriate force closure, in that certain muscles become overactive while others remain inactive, delayed, or asymmetrical in their recruitment.124 When approaching SIJ dysfunction it is likely more important to determine why there are symptoms, rather than attempting to identify the specific symptom generating structures.
In most cases, an examination of the pelvic joints is of little use if the lumbar spine and the hip joints have not been previously cleared by examination or intervention, because both of these joints can refer pain to this area and may also profoundly affect the function of the SIJ.
History
A history of low back pain or leg pain, or both, warrants an examination of the lumbopelvic–hip complex. The most common presenting symptoms in patients with SIJ dysfunction are complaints of pain or tenderness over the region of the PSIS.125–127 The clinician must also determine whether the current problem is a consequence of pregnancy and/or delivery. If so, it is important to ascertain when the symptoms began, what was the nature of the delivery, and how much trauma occurred to the pelvic floor and the abdominal wall.128
The following findings are likely to be present with an SIJ dysfunction:12,55,129,130
 A history of sharp pain that occurred with a particular activity and that awakens the patient from sleep upon turning in bed. The clinician must ask what kind of bed the patient sleeps in, and what position is most frequently adopted.
A history of sharp pain that occurred with a particular activity and that awakens the patient from sleep upon turning in bed. The clinician must ask what kind of bed the patient sleeps in, and what position is most frequently adopted.
 Pain with running, walking, ascending or descending stairs, or hopping or standing on the involved leg.
Pain with running, walking, ascending or descending stairs, or hopping or standing on the involved leg.
 Pain with forward bending of the trunk and pain with standing hip flexion.
Pain with forward bending of the trunk and pain with standing hip flexion.
 Pain with transitional movements such as rising to stand from a sitting position or getting in and out of the car.
Pain with transitional movements such as rising to stand from a sitting position or getting in and out of the car.
 Pain with a straight-leg raise at, or near, the end of the range (occasionally early in the range when hyperacute).
Pain with a straight-leg raise at, or near, the end of the range (occasionally early in the range when hyperacute).
 Pain and sometimes limitation on extension and ipsilateral side bending of the trunk.
Pain and sometimes limitation on extension and ipsilateral side bending of the trunk.
 Pain that is worsened with long periods of sitting or standing if the lumbar lordosis is not maintained.
Pain that is worsened with long periods of sitting or standing if the lumbar lordosis is not maintained.
The clinician must determine the exact location of the pain/dysesthesia and whether it is localized or diffuse, and its quality (see Chapter 4). If the symptoms do radiate, the clinician must determine how far down the limb or limbs the symptoms are felt, or whether the symptoms radiate into the abdomen or thorax.128
Finally, the clinician should ask the patient if there have been any adjunctive diagnostic tests (i.e., x-ray, computed tomography, or magnetic resonance imaging), or any laboratory tests.
Systems Review
Given the number of visceral organs in the vicinity of the SIJ, the clinician must complete a thorough systems review to rule out a visceral source for the symptoms. A Cyriax scanning examination (see Chapter 4) should be performed on any patient who presents with an insidious onset of pelvic pain. The scanning examination, which includes the primary stress tests (anterior and posterior distraction), can be used to help detect sacroiliitis resulting from microtraumatic arthritis, macrotraumatic arthritis, or systemic arthritis (e.g., ankylosing spondylitis, Reiter’s syndrome), or the more serious pathologies grouped under the sign of the buttock (see Chapter 19). Primary breast, lung, and prostate cancers are among the most common cancers to metastasize to the axial skeleton, including the pelvic ring.131 A further source of sacral pain can be a stress fracture of the sacrum, which can be associated with a wide range of extrinsic and intrinsic risk factors (see “Intervention Strategies”), and an equally wide range of symptoms and signs.132
Tests and Measures
As previously mentioned, in order to rule in or rule out SIJ dysfunction, a thorough musculoskeletal examination of the low back, the pelvis, the hips, and the remainder of the lower extremities, including a full neurologic evaluation must be performed.
Observation
The observation should begin as the patient enters the treatment area to assess the impact the patient’s condition has on gait. As described in chapter 6, there should be minimal deviation of the head in either plane and no deviation of the pelvis in the coronal plane relative to the lumbar spine and hip (Trendelenburg sign). Asymmetry in stride length and time spent in each phase of the gait cycle can be indicative of impairments within the lumbopelvic hip complex.128 In addition, an avoidance of the normal heel impact at initial contact may indicate an attempt by the patient to reduce the ground reaction forces and resultant joint loading.
Observation should also include an overall assessment of posture to check for the presence of asymmetry (see Chapter 6). The primary spinal curves should be maintained (i.e., gentle even lumbar lordosis, thoracic kyphosis, and cervical lordosis), and there should be no kinks, shifts, hinges, or transverse plane rotations in the entire spinal curve.128 The clinician should observe the degree of tilt at the pelvis. The question of cause and effect should be raised. An anterior pelvic tilt, which occurs when the anterior-superior iliac spine (ASIS) moves anteriorly and inferiorly, causes hip flexion and an increase in the lumbar lordosis (extension) and thoracic kyphosis. The anterior pelvic tilt results in a stretching of the abdominals and the sacrotuberous, SI, and sacrospinous ligaments, and an adaptive shortening of the hip flexors, the hamstrings, and the erector spinae. In contrast, a posterior pelvic tilt, which occurs when the PSIS moves posteriorly and inferiorly, results in lengthening of the hip flexors, the hamstrings, and the erector spinae, and adaptive shortening of the abdominals and the gluteals.
A lateral pelvic tilt results in opposite motions at each side of the pelvis. The pelvic motion is defined by what is occurring at the iliac crest of the pelvis that is opposite the weight-bearing extremity/side of the pelvis that is moving. A lateral pelvic tilt may be caused by scoliosis with ipsilateral lumbar convexity, a leg-length discrepancy, or shortening of the contralateral quadratus lumborum. This position results in adaptive shortening of the ipsilateral hip abductors and contralateral hip adductors, and weakness of the contralateral hip abductors. A lateral pelvic tilt is not the same as a pelvic shift. A pelvic shift results in extension of the hip and extension of the lower lumbar spinal segments and is often seen with slouched or relaxed postures.
There appears to be a strong correlation between the position of the pelvis and the forward head.133 If the pelvic landmarks are asymmetric, and the patient has a forward head, the clinician should attempt to correct the forward head. If the attempted correction of the forward head worsens the pelvic asymmetry and increases the symptoms, the intervention should be aimed at correcting the asymmetry. If the attempted correction of the forward head improves the pelvic asymmetry and the symptoms, the subsequent intervention should be aimed at correcting the forward head.134
Hip Range of Motion
The ROM of the hip, including internal and external rotation, is performed to help rule out pain referred from the hip joint. Although a unilateral limitation of hip motion, in which one of the motions is unequal between the left and right sides, has been observed in patients with disorders of the SIJ,76,135–137 the evidence to demonstrate whether hip motion is limited in patients with signs of SIJ dysfunction is inconclusive. LaBan et al.64 noted asymmetry in hip abduction and external rotation in patients with inflammation of the SIJs. Dunn et al.138 reported limited hip mobility in patients with infection of the SIJ; however, no mention was made as to which movements were limited.
Others have described cases in which patients with low back pain had unilateral, limited internal hip rotation and excessive external hip rotation, and also exhibited signs of SIJ dysfunction. A recent study by Cibulka et al.135 attempted to determine whether a characteristic pattern of hip ROM existed in patients with low back pain, and whether those classified as having SIJ dysfunction have a different pattern of hip ROM compared with those with unspecified low back pain. The study found that patients with low back pain, who had signs suggesting SIJ regional pain, had significantly more hip external than internal rotation ROM on one side. The authors concluded that identifying unilateral hip ROM asymmetry in patients with low back pain might help in diagnosing SIJ regional pain.135 Hip ROM and its relation to lumbar and pelvic motion can be assessed using the one-leg stand test, also known as the stork test or Gillet test.
One-Leg Stand Test. The patient is positioned in standing and is then asked to stand on one leg, and to flex the contralateral hip and knee towards the waist. The clinician observes the effort required and the ability to perform the task. The pelvis should not anteriorly/posteriorly/laterally tilt, nor rotate in the transverse plane as the weight is shifted to the supporting limb.128 The test is then repeated on the opposite side. Once the patient has performed this maneuver several times, the clinician kneels behind the patient and, using the thumb of one hand, palpates the PSIS, and the thumb of the other hand to palpate the sacrum at either S2 or the ipsilateral ILA. The patient is asked to repeat the test while the clinician palpates. A small amount of posterior rotation of the innominate during this maneuver should be felt, and the quality and amplitude should be symmetrical between left and right sides.128
Lumbopelvic Range of Motion
Forward Bending. The patient is positioned in standing and is asked to bend forward at the waist while the clinician observes and palpates. Forward bending at the waist results in a posterior displacement of the pelvic girdle which, in turn, shifts the center of gravity (COG) behind the pedal base such that slight plantar flexion of the talocrural joint occurs.139 When the leg lengths are equal, the sacrum should nutate bilaterally and symmetrically relative to the innominates and remain nutated throughout the forward bending motion as the pelvic girdle flexes at the hip joints.118 The innominate should remain posteriorly rotated relative to the sacrum throughout the forward bend. When the pelvis unlocks, the innominate can be felt to rotate anteriorly relative to the ipsilateral sacrum.87,140 There should be a symmetry of the paravertebral fullness between the thorax and the pelvic girdle so that it is equal on both sides of the spinal column. As the patient returns to the standing position, the sacrum should remain symmetrically nutated until the erect posture is reached. There is no relative anterior or posterior rotation between the innominates during forward bending, but both should travel an equal distance as the pelvic girdle anteriorly tilts.139 The forward bending should be repeated several times to note the consistency/inconsistency of any positive findings and the ease with which the patient is able to bend forward repeatedly.128 A positive test for inadequate load transfer is if there is a lack of anterior pelvic tilt, excessive flexion of the thoracolumbar spine, and any twisting that occurs in the pelvic girdle.97 Although asymmetry of motion of the innominate during forward bending is a positive finding, it is not indicative of any specific dysfunction of the SIJ.
Backward Bending. The patient is positioned in standing and is asked to bend backward at the waist while the clinician observes and palpates. Backward bending at the waist results in an anterior displacement of the pelvic girdle which, in turn, shifts the COG in front of the pedal base such that slight dorsiflexion of the talocrural joint occurs.139 When the leg lengths are equal, the sacrum should counternutate bilaterally and symmetrically relative to the innominates and remain counternutated throughout the backward bending motion as the pelvic girdle extends symmetrically at the hip joints.118 The lumbar spinal segments should extend symmetrically without shifting or hinging, and the innominate should remain posteriorly rotated relative to the sacrum as the pelvic girdle tilts posteriorly throughout the backward bend. As the pelvis unlocks, the innominate can be felt to rotate anteriorly relative to the ipsilateral sacrum. Even though the pelvic girdle is tilting posteriorly, it is the relative motion between the innominate and the sacrum that is important to assess.128 As the patient returns to the standing position, the sacrum should remain symmetrically counternutated until the erect posture is reached. There is no relative anterior or posterior rotation between the innominates during forward bending, but both should travel an equal distance as the pelvic girdle posteriorly tilts.139 The backward bending should be repeated several times to note the consistency/inconsistency of any positive findings and the ease with which the patient is able to bend backwards repeatedly.128 A positive test for inadequate load transfer is if there is a lack of posterior pelvic tilt, excessive extension of the thoracolumbar spine, and any twisting that occurs in the pelvic girdle.97
Side Bending. The patient is positioned in standing and is asked to side bend to the right and then to sidebend to the left while the clinician observes and palpates. Right side bending of the body is initiated by displacing the upper legs/pelvis to the left so that the right femur abducts and the left femur adducts, thus maintaining the COG within the pedal base.139 The apex of this lateral bending curve should be at the level of the greater trochanter, and the body should remain in the coronal plane. The lumbar spinal segments should sidebend symmetrically without shifting or kinking. At the pelvis, during side bending, the left innominate posteriorly rotates relative to the right innominate, and the sacrum rotates to the left while the lumbar spine side bends to the right.139 The reader should be able to extrapolate what happens during left side bending.
Landmark Palpation
The palpation of landmarks can be used to locate areas of tenderness rather than for detecting pelvic asymmetry, because as asymmetry of pelvic landmarks is the norm, “positive” findings are likely to be misleading.114 The various landmarks of the pelvis are palpated with the patient positioned standing, sitting, and lying (see Figs. 29-8 and 29-9).
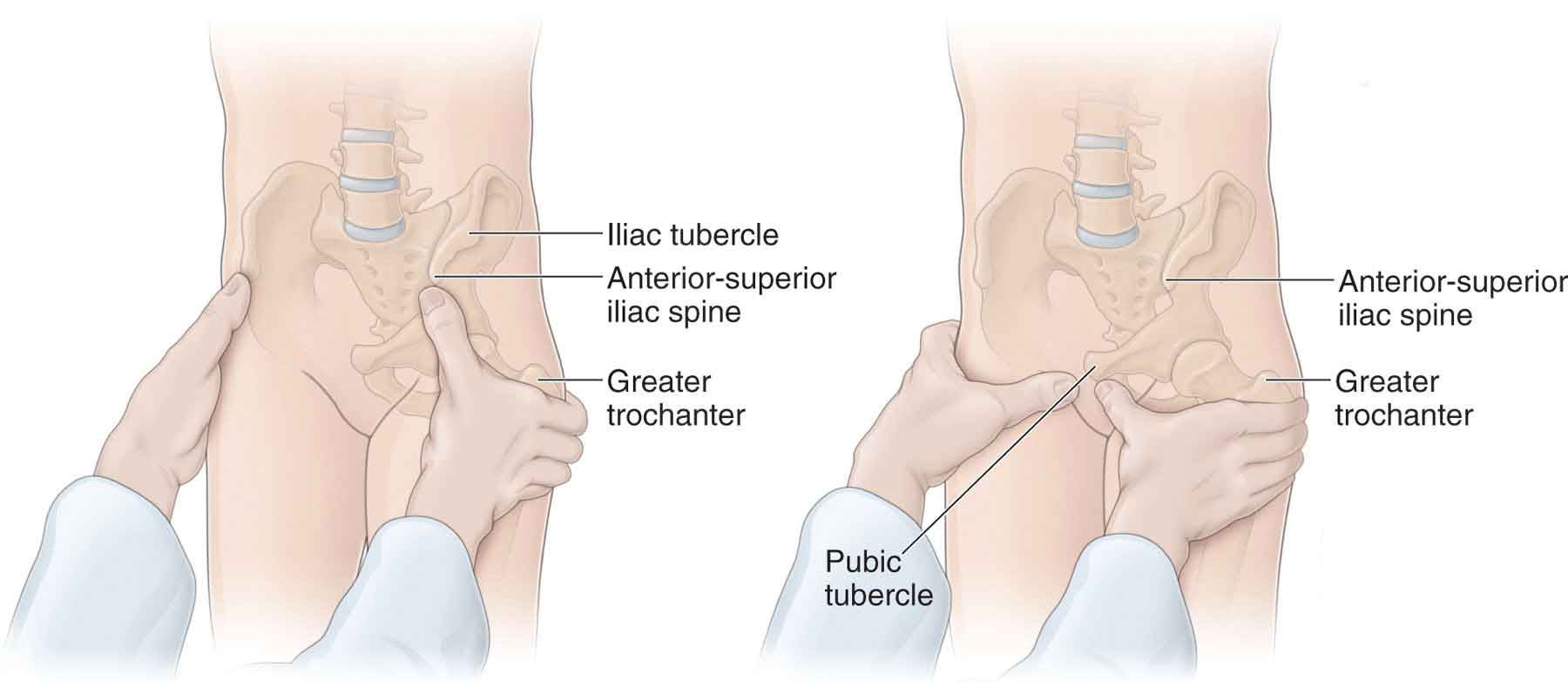
FIGURE 29-8 Palpation of the hip and pelvis.
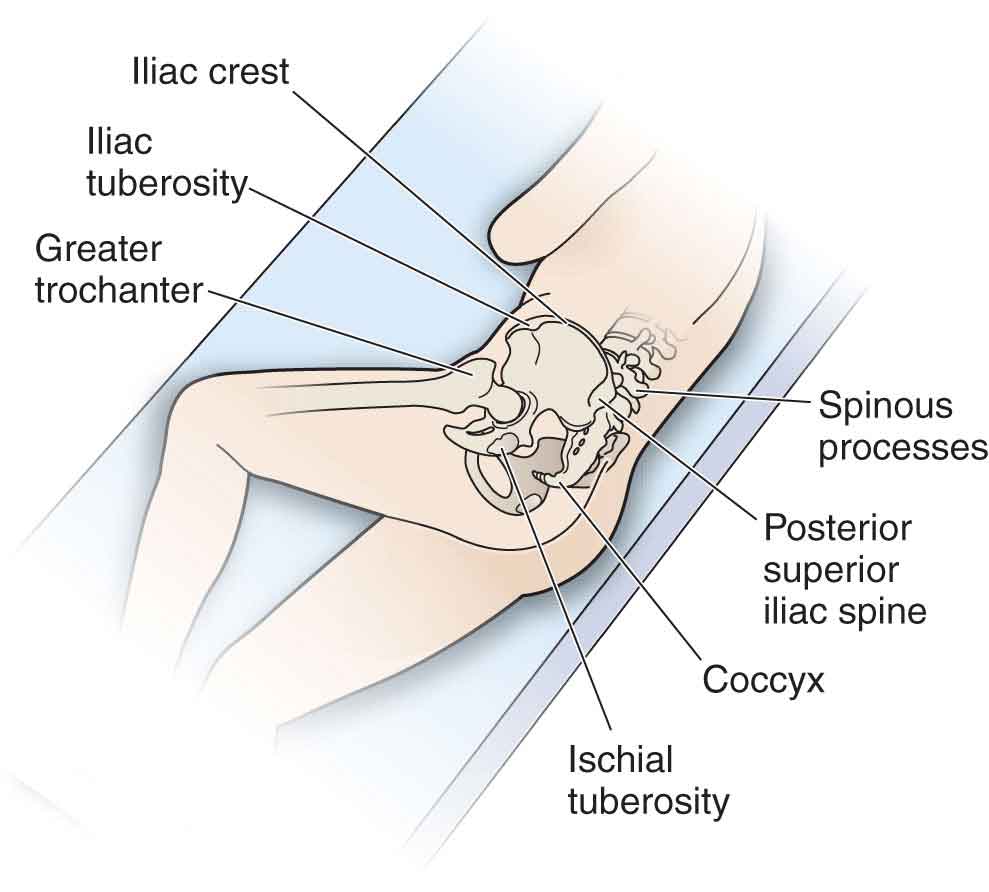
FIGURE 29-9 Bony landmarks.


