CHAPTER 42 The patient with hyperlaxity and shoulder instability—ehlers-danlos and other disorders
 Heritable disorders of connective tissue comprise (1) Ehlers-Danlos syndrome, Marfan syndrome, and osteogenesis imperfecta, which are rare; and (2) benign joint hypermobility syndrome, which is common, but rarely diagnosed.
Heritable disorders of connective tissue comprise (1) Ehlers-Danlos syndrome, Marfan syndrome, and osteogenesis imperfecta, which are rare; and (2) benign joint hypermobility syndrome, which is common, but rarely diagnosed.Introduction
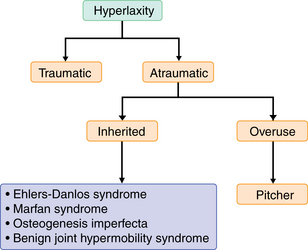
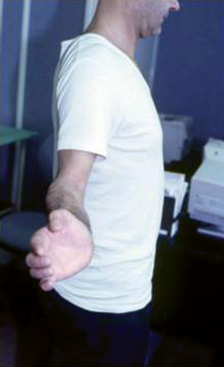
Hyperlaxity can be due to a congenital disease, to overuse in athletes such as pitchers, and to a traumatic shoulder instability event (Fig. 42-1).
Shoulder instability classification differentiates1 the involuntary instability that can occur in one (anterior or posterior) or more than one direction (multidirectional instability [MDI]; anterior, posterior, inferior) from voluntary instability. Instability can be due to either a traumatic or nontraumatic event in a patient with or without preexisting hyperlaxity.
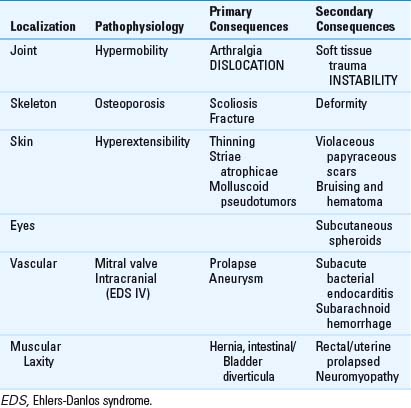
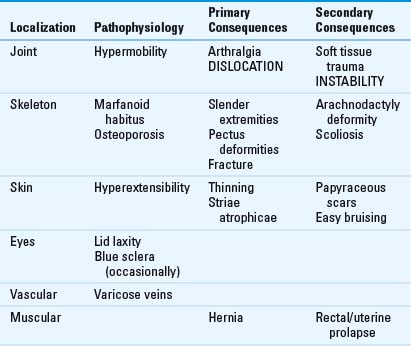
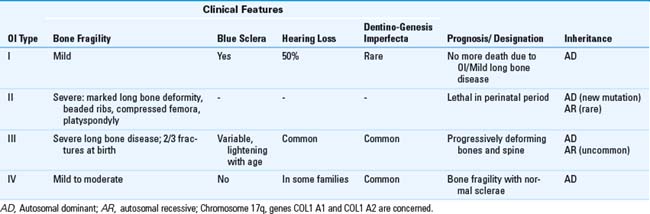
Heritable disorders of connective tissue (HDCT)2 are still studied by geneticists to define their precise biochemical and genetic etiology. They comprise a group of genetic disorders concerning connective tissue matrix protein. The proteins concerned include collagens, elastins, fibrillins, and almost certainly others that have yet to be discovered. The fragility of the tissue is due to modification of collagen component (Fig. 42-2). Because proteins are spread in all the body, symptoms can vary greatly and can affect joints, skeleton (ligaments, tendon, muscle, skin break, and healing) (Table 42-1), eyes, and vasculature.

FIGURE 42-2 Molecular representation of the type 1 collagen in triple helix organization.
(Courtesy of Drs. Baujat and Finidori, Necker Hospital, Genetics Department and Pediatric Orthopaedic Surgery Department, Paris, France.)
The heritable disorders of connective tissue concern four main disorders and all can present with shoulder hyperlaxity and instability3:
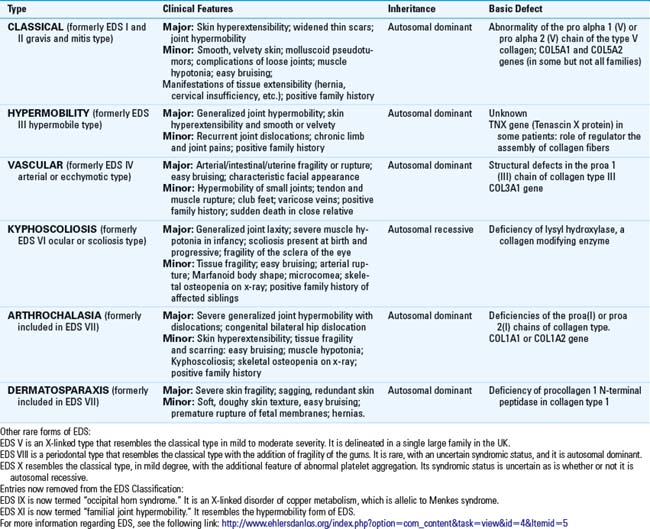
Ehlers-Danlos syndrome has been regrouped into nine types.5 Its cardinal feature is skin hyperextensibility (Table 42-2). The former type III is the hypermobile one that is autosomal dominant6; the former type VII, the arthrochalasia type is also autosomal dominant but occurs more rarely (Table 42-3).
Benign joint hypermobility syndrome (BJHS) is clinically close to the Ehlers-Danlos articular hypermobility syndrome (Table 42-4). The diagnosis of BJHS was revised by Brighton in 19987 (Table 42-5). The joint laxity is due to a laxity of joint ligaments and predisposition to ligamentous injury. It confers an excessive range of movement compared with other people of the same age, gender, and origin.
Table 42-5 Revised Diagnostic Criteria for Benign Joint Hypermobility Syndrome3
| Major criteria | |
| Minor criteria | Marfanoid habitus (tall, slim, span > height, upper/lesser segment ratio less than 0.89 and arachnodactyly) |
| Diagnosis |
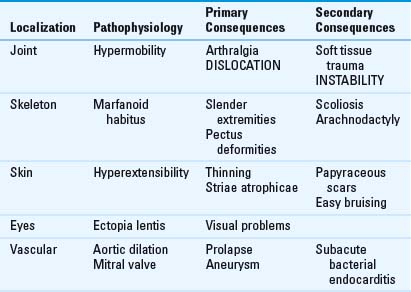
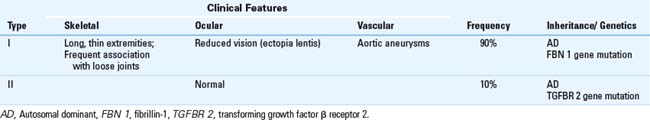
Marfan syndrome is an autosomal dominant disorder. The main feature is the marfanoid body shape with long, slender extremities, and arachnodactyly (Table 42-6). Ectopia lentis, aortic dissection and dilation, mitral valve prolapse, and dural ectasia can occur in the phenotype. The causative gene was found in 1990 on chromosome 15q21, encoding for the microfibrillar protein fibrillin-1 (FBN 1) and FBN 28 (Table 42-7).
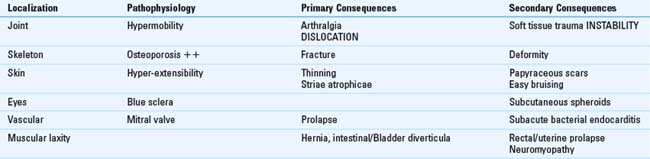
Patients presenting osteogenesis imperfecta have brittle bones and blue sclera for principal features (Table 42-8). Sillence classified this autosomal dominant pathology into four types (Table 42-9).9 Molecular research has revealed that osteogenesis imperfecta results from mutation of 1 of the 2 genes encoding for type 1 collagen (COL1A1 and COL1A2). Wordsworth described joint mobility in these patients.10
Indications/contraindications
Preoperative history, examination, and radiographic findings
Examination findings
Patient shoulder examinations can look for:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree