Abstract
Objective
To study the applicability and responsiveness of the motor function measure (total score and sub-scores D1, D2 and D3) in patients with Charcot-Marie-Tooth disease.
Patients and methods
Two hundred and thirty-three patients aged 4–86 years were included in the descriptive study. Scores and sub-scores were analyzed by age and by disease subtypes. Sensitivity to change (responsiveness) was estimated in patients having had at least two evaluations with at least six months between the first and the second.
Results
Motor function measure scores decrease with age, especially sub-scores D1 and D3. There were no significant differences between the scores according to type of Charcot-Marie-Tooth disease. The scores were significantly higher for ambulatory than for non-ambulatory patients. Significant responsiveness was demonstrated only in type 2 Charcot-Marie-Tooth disease.
Discussion/conclusions
Our results suggest that, especially for D1 and D3 sub-scores, the motor function measure is a reliable and valid outcome measure that can be usefully applied in longitudinal follow-up. Studies of longer duration could demonstrate its responsiveness in other Charcot-Marie-Tooth disease subtypes.
Résumé
Objectif
Étudier l’applicabilité et la sensibilité au changement du score total et des trois sous-scores, D1, D2 et D3 de la mesure de fonction motrice chez des patients atteints de maladie de Charcot-Marie-Tooth.
Patients et méthodes
Étude descriptive sur 233 patients âgés de 4 à 86 ans. Les scores ont été analysés en fonction de l’âge et du type de la maladie. Les sensibilités au changement ont été étudiées chez les patients ayant eu au moins deux évaluations espacées d’au moins six mois.
Résultats
Les scores de la Mesure de Fonction Motrice diminuent avec l’âge, surtout les sous-scores D1 et D3. Il n’existe pas de différence significative en fonction du type de la maladie. Les scores des patients non ambulants sont significativement plus faibles que ceux des patients ambulants. La sensibilité au changement est significative chez les Charcot-Marie-Tooth type 2.
Conclusion
La mesure de fonction motrice est une échelle applicable, surtout D1 et D3, au suivi des patients atteints de la maladie de Charcot-Marie-Tooth de façon longitudinale. Sa sensibilité au changement nécessite d’être confirmée en utilisant des durées d’étude plus longues compte tenu de l’évolutivité de la maladie.
1
English version
1.1
Introduction
Charcot-Marie-Tooth disease (CMT) is one of the most frequent hereditary neuromuscular diseases (NMD), with a prevalence in France of 1 out of 2500 persons . In fact, CMT is a group of diseases characterized by damage to the nerves of the arms and the legs (peripheral nerves) and presenting considerable genetic heterogeneity, with more than 30 potentially responsible genes . Patients suffering from CMT are categorized in sub-groups according to nerve damage and mode of transmission (CMT1: demyelinating form, autosomal dominant; CMT2: axonal form, autosomal dominant or recessive; CMT4: demyelinating form; autosomal recessive; CMTX: form related to chromosome X and IAD: intermediate autosomal dominant) and present highly variable clinical pictures (peroneal muscle atrophy, damaged intrinsic hand muscles, areflexia, deformation of the feet…). Disease development is often slowly progressive and age at symptom onset greatly varies from one individual to the next .
Even though no medical CMT treatment is currently available, studies carried out on animal models have yielded promising results and trials have been or will soon be conducted in humans. Moreover, the effects in humans of ascorbic acid, progesterone and its derivatives, neurotrophine 3 and curcumin have been studied. That much said, precise study of the effects in humans of therapeutic products necessitates valid, sensitive and reproducible assessment tools. From a clinical standpoint, functional assessment both improves long-term patient follow-up and enhances knowledge of the natural development of the disease. More specifically, functional assessment can help to anticipate and forestall some consequences of the disease through appropriate management and adequate technical support.
In 2010, the 168th ENMC international workshop provided an occasion for a review of the available CMT assessment tools . Among these tools, the most widely used are the CMT neuropathy score (CMTNS) , which is the only CMT-specific measurement, and the neuropathy impairment score (NIS) . Both of them have been validated on patients of at least 10 years of age. While the CMTNS takes into account the findings of the neurological exam, the results of electromyogram testing, sensitivity and muscle strength , the NIS scale is a standard scale that evaluates 24 muscle groups, five osteo-tendinous reflexes and disturbed sensation, which is assessed on the dorsal side of the last phalanx of the index finger and the great toe. Only in cases of CMT1A and CMTX has the course of CMT development been studied using the CMTNS and the NIS. The two scales have been shown to effectively detect CMTA change and progression, and the authors recommend study of the development of the other types of CMT using this tool .
As CMT onset generally occurs during the first decade of life, a scale known as the CMT Pediatric Scale (CMTPedS) has been developed ; it is well-tolerated, reliable and reproducible. However, since it is usable only for children, it does not allow for longitudinal follow-up after transition in the adult.
The motor function measure (MFM) is a precise scale that has been validated for most cases of NMD. It objectifies the repercussions of muscle weakness on motor functioning and is appropriate with regard to most neuromuscular diseases, whatever their level of severity. The scale exists in two versions, one of which consists in 32 items and has been validated for NMD patients aged from six to 60 years (MFM-32), while the other comprises 20 items (MFM-20) and has been validated for children of two to six years of age . Validation studies of MFM-32 and MFM-20 have led to the categorization of three motor functions:
- •
D1: standing position and transfers (13 items for MFM-32 et 8 for MFM-20);
- •
D2: axial and proximal motor function (12 items for MFM-32 et 8 for MFM-20);
- •
D3: distal motor function (seven items for MFM-32 et 4 for MFM-20).
The proof-of-concept MFM-32 study, which was conducted in a population of 303 NMD patients of whom 35 were suffering from peripheral neuropathy, successfully demonstrated the robust metrological properties of the tool , and later studies conclusively demonstrated its validity and responsiveness in the different groups of NMD patients .
One advantage of the MFM-32 is that contrarily to the CMTNS, NIS and CMTPedS scales, it is applicable to patients aged from six to 60 years; moreover, it does not take into account the data provided by an electromyogram (EMG), which remains an invasive test that is difficult to carry out systematically, during each consultation.
The objective of this work is to study the applicability and, more particularly, the responsiveness or sensitivity to change (for the total score and the three sub-scores, D1, D2 and D3) of the MFM scale in patients with CMT.
1.2
Patients et methods
1.2.1
Study design
This is a multicenter observational cohort study.
1.2.2
Study population
The patients included were at least four years old, had CMT disease (suspected or confirmed by genetic analysis) and had agreed to have their medical data used for the purposes of clinical research.
The patients were classified in the following diagnostic groups: CMT1, CMT2, other CMTs (CMT4, CMTX and IAD) and ns CMT (non-specified).
1.2.3
Data collection
The data collected in our study originated in the MFM database, which has been available on Internet since 2007 and allows the participating departments to securely enter MFM data pertaining to their patients (for further information, consult www.mfm-nmd.org ).
The collected data included the different MFM items, date of exam, patient birth date, sex, previous surgery, presence (or non-presence) of ventilation, ambulatory (or non-ambulatory) status (a patient is considered as ambulatory if he is able to take 10 steps in an indoor setting without human assistance and with or without technical assistance or devices), age of patient when the first symptoms appeared.
1.2.4
Participating centers
From January 2007 to April 2013, 15 French departments and one Swiss department of physical medicine and rehabilitation, neurology and/or consultations in a reference center for neuromuscular diseases included at least one CMT patient in the MFM database.
1.2.5
The MFM scale
MFM is a generic scale designed to assess motor function in children and adults with neuromuscular disease. The MFM-32 has been validated in patients aged from six to 60 years and comprises 32 terms divided into 3 sub-scores :
- •
D1 (standing position and transfers);
- •
D2 (axial and proximal motor function);
- •
D3 (distal motor function).
The initial MFM validation study did not take into account the psychomotor development of the young child; test-taking duration and the complexity of some of the items were not suitable for young patients. A short version of the MFM-32 has been developed; known as the MFM-20, it consists in 20 items drawn from the MFM-32, and is specifically addressed to children ranging in age from two to seven years.
MFM ratings are based in a 4-Point Likert scale assessing the maximum capacities of a subject not aided by another person: 0 = does not initiate movement or starting position cannot be maintained; 1 = partially completes the exercise; 2 = completes the exercise with compensations or slowness; 3 = completes the exercise “normally”. The total score is established by adding up the scores given for the different items, and it ranges from 0 to 100%.
1.2.6
Statistics
The quantitative variables were described using means, standard deviations and intervals. The qualitative variables were described using numbers and percentages.
Floor and ceiling effects were analyzed by calculating the percentage of the population with a MFM score of 0% and the percentage of the population with a score of 100% respectively. Percentages lower than 20% were considered as acceptable.
The relationships between MFM scores and patient age were analyzed using a linear regression model.
Mean MFM scores were analyzed by diagnostic categories and according to the patients’ ambulatory status. Analysis of variance (Anova) was used to underscore significant differences between groups.
Sensitivity to change (responsiveness) was studied in patients having been evaluated at least two times by the MFM, with a time interval of at least six months between the first and the following MFM. For each patient, repeated measures of the MFM D1, D2, D3 scores and of the total score (TS) were summarized by the trend line slope expressed in terms of annual rate using the « unweighted least-square estimate » . The slopes were subsequently expressed as « standardized response mean » (SRM) by calculating the relationship between mean slope divided by standard deviation of the mean. SRM values were considered as high when > 0.80, moderate from 0.50 to 0.79 and weak when < 0.50 .
1.3
Results
1.3.1
Population characteristics
All in all, 25 MFM-20 and 407 MFM-32 scores from 233 CMT patients (111 men and 122 women) ranging in age from 4 to 86 years were recorded in the MFM database. Characteristics of the patients on the day of their first MFM testing are described on Table 1 .
| Variables | Population | CMT1 | CMT2 | Other CMTs | ns CMTs |
|---|---|---|---|---|---|
| Number of patients | 233 | 86 | 34 | 13 | 100 |
| Confirmed diagnosis | 54.1% (126) | 80.2% (69) | 44.1% (15) | 53.8% (7) | 35% (35) |
| Male | 47.6% (111) | 47.7% (41) | 41.2% (14) | 46.2% (6) | 50% (50) |
| Mean age at 1st MFM (years) | 33.7 ± 21.6 (3.6–86) | 33 ± 20.5 (6.2–70) | 35.8 ± 21.2(4.2–71.9) | 34.6 ± 23.9 (3.7–60.3) | 33.5 ± 23.4(3.6–85.9) |
| Age at first symptoms (years) | 21.34 ± 20.6 (1–77) | 18.82 ± 18 (1–56) | 24.4 ± 21.8 (2–58) | 24.7 ± 24.1 (2–54) | 22.89 ± 23.0 (1–77) |
| Loss of ambulation | 3% (7) | 3.5% (3) | 5.9% (2) | 0% (0) | 2% (2) |
| Use of wheelchair | 6.9% (16) | 3.5% (3) | 5.9% (2) | 7.7% (1) | 10% (10) |
| History of foot surgery | 22.7% (53) | 27.9% (24) | 23.5% (8) | 23.1% (3) | 18% (18) |
| Respiratory assistance | 4.3% (10) | 5.8% (5) | 2.9% (1) | 7.7% (1) | 3% (3) |
| MFM-32 score (%) | 223 | 82 | 33 | 11 | 97 |
| D1 | 67.4 ± 24.3 (0–100) | 70.67 ± 22 (18–100) | 64.41 ± 27.9 (0–100) | 70.7 ± 21.9 (28.2–89.7) | 65.7 ± 25.1 (10.3–100) |
| D2 | 96.0 ± 6.6 (41.7–100) | 97.6 ± 4.2 (83.3–100) | 95.79 ± 10.7 (41.7–100) | 98.8 ± 3.4 (88.9–100) | 96.5 ± 6.7 (63.9–100) |
| D3 | 87.9 ± 13 (9.5–100) | 89.3 ± 9.7 (57.1–100) | 84.99 ± 19.5 (9.5–100) | 83.3 ± 16.8 (42.9–100) | 88.4 ± 12.1 (47.6–100) |
| TS | 83 ± 13.4 (17.7–100) | 97.5 ± 11.3 (56.3–100) | 80.68 ± 17.8 (17.7–100) | 84 ± 12 (58.3–94.8) | 82.2 ± 13.3 (47.6–100) |
| MFM-20 score (%) | 10 | 4 | 1 | 2 | 3 |
| D1 | 94.2 ± 6.86 (79.2–100) | 96.9 ± 4 (91.7–100) | 100 ± / | 93.6 ± 2.9 (95.7–95.83) | 88.9 ± 10.5 (79.2–100) |
| D2 | 98.8 ± 2.81 (91.7–100) | 99 ± 2.1 (95.8–100) | 100 ± / | 100 ± 0 | 97.22 ± 4.8 (91.7–100) |
| D3 | 95.8 ± 6 (83.3–100) | 95.8 ± 4.8 (91.7–100) | 91.7 ± / | 100 ± 0 | 94.44 ± 9.6 (83.3–100) |
| TS | 96.3 ± 3.8 (88.3–100) | 97.5 ± 2.2 (95–100) | 98.3 ± / | 97.5 ± 1.2 (96.7–98.3) | 93.33 ± 6 (88.3–100) |
Mean patient age on the day of the first MFM was 33.7 years ± 21.6 (4–86). Due to their age, 10 patients who were not yet seven years old were given the MFM-20. All the other patients, of whom 33 were seven to 10 years old, were given the MFM-32. Only 3% of the patients could no longer walk, and 6.9% used a manual or electric wheelchair during all or part of the day.
Previous foot surgery had been undergone by a substantial proportion of the patients (22.7%). Finally, 4.3% of the patients, half of whom (5 out of 10) belonged to the CMT1 group, required non-invasive intermittent respiratory assistance using a mask.
Mean MFM test duration (MFM-32: 99 patients, MFM-20: 11 patients) was 35.36 minutes ± 13.1 (minimum: 15 min, maximum: 70 min) for the MFM-32 and 18.18 minutes ± 3.25 (minimum: 15 min, maximum: 25 min) for the MFM-20.
1.3.2
The Motor Function Measure scores
1.3.2.1
Changes of the MFM scores according to age and type of CMT
In order to facilitate comparison, patients were assigned to the following diagnostic-related groups: CMT1, CMT2, ns CMT (non-specified diagnoses) and other CMT (consisting in 6 CMTX, 2 CMT IAD and 5 CMT4).
On an overall basis, DI (standing position and transfers) D3 (distal motor function) diminished pronouncedly with age, whatever the type of CMT ( Fig. 1 ).
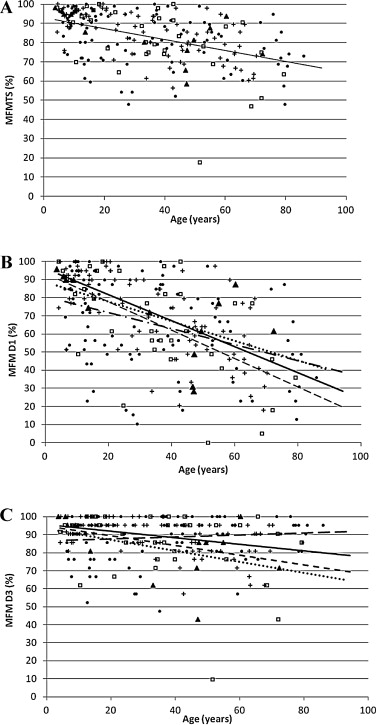
 : other CMTs;
: other CMTs;  : ns CMTs. A. Regression line for all CMT patients: y = −0.2878 x + 93.146. B. Regression lines for each type of CMT:
: ns CMTs. A. Regression line for all CMT patients: y = −0.2878 x + 93.146. B. Regression lines for each type of CMT:  CMT1: y = −0.72 x + 96.167;
CMT1: y = −0.72 x + 96.167;  CMT 2: y = −0.7827 x + 93.5;
CMT 2: y = −0.7827 x + 93.5;  other CMTs: y = −0.5407 x + 88.557;
other CMTs: y = −0.5407 x + 88.557;  ns CMTs: y = −0.4413 x + 80.595. C. Regression lines for each type of CMT:
ns CMTs: y = −0.4413 x + 80.595. C. Regression lines for each type of CMT:  CMT1: y = −0.1822 x + 95.706;
CMT1: y = −0.1822 x + 95.706;  CMT 2: y = −0.2716 x + 94.918;
CMT 2: y = −0.2716 x + 94.918;  other CMTs: y = −0.3075 x + 93.425;
other CMTs: y = −0.3075 x + 93.425;  ns CMTs: y = 0.0555 x + 86.492.
ns CMTs: y = 0.0555 x + 86.492. D1 was the earliest and most pronouncedly lowered sub-score in our CMT population. The D1 decrease was greater for the CMT2 ( y = –0.7827 x + 93.5) and the CMT1 ( y = –0.72 x + 96.167) patients than for other CMT ( y = –0.5407 x + 88.557) and for ns CMT (y = –0.4413x + 80.595) patients ( Fig. 1 B).
D3 sub-scores diminished more slowly over time than D1 sub-scores. “Other CMT” evidenced a significantly greater D3 diminution over time ( y = –0.3075 x + 93.425) than was the case with CMT1 ( y = –0.1822 x + 95.706) ( Fig. 1 C).
D2 (axial and proximal motor function) sub-scores varied very little according to age and remained close to 100%, whatever the age and type of CMT ( y = –0.0781 x + 99.627) (not shown).
1.3.2.2
Differences of MFM scores according to CMT subtype
Fig. 2 A shows that CMT2 patients underwent greater motor function alteration than CMT1 patients, whatever the total score and the MFM sub-score, but the difference did not reach significance for D1 (65.5 ± 28.1 vs. 71.9 ± 22.2, P = 0.35), for D2 (95.9 ± 10.6 vs. 97.7 ± 4.2, P = 0.40), for D3 (85.2 ± 19.2 vs. 89.6 ± 9.6, P = 0.30), and for total score (81.2 ± 17.8 vs. 85.4 ± 11.4, P = 0.16) respectively.
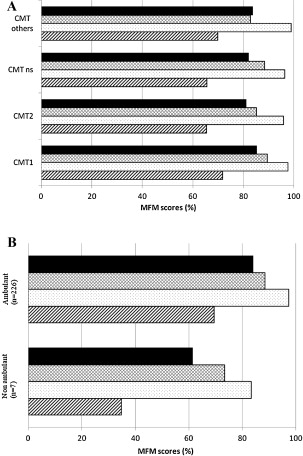
 total score for the MFM (MFM TS);
total score for the MFM (MFM TS);  sub-score D3 for the MFM (MFM D3);
sub-score D3 for the MFM (MFM D3);  sub-score D2 for the MFM (MFM D2);
sub-score D2 for the MFM (MFM D2);  sub-score D1 for the MFM (MFM D1).
sub-score D1 for the MFM (MFM D1). 1.3.2.3
Differences of MFM scores according to the patients’ ambulatory status
Ambulatory patients had significantly more elevated D1, D2, D3 and total MFM scores than did non-ambulatory patients ( Fig. 2 B): D1: 69.5 ± 23.5 vs. 34.8 ± 33.4, P < 0.001; D2: 97.4 ±4.9 vs. 83.3 ± 22.6, P < 0.001; D3: 88.6 ± 11.8 vs. 73.5 ± 30.7, P < 0.001 and total score: 84.1 ±12.3 vs. 61.5 ± 26, P < 0.001, respectively.
1.3.3
Floor effect and ceiling effect
As regards the floor effect, no patient had 0% as a D2, D3 or total score. One patient, representing 0.4% of the total population, had 0% as a D1 score.
As regards the ceiling effect, the maximum score (100%) was reached by 6.4% of the patients for D1 score, 62.7% for D2 score, 19.7% for D3 score and 3% for total score.
1.3.4
Sensitivity to change
All in all, 102 patients (4 to 80 years of age) out of the 233 patients having had at least 2 MFMs recorded in the MFM study database were included in the study of responsiveness or sensitivity to change. Their characteristics are described in Table 2 .
| CMT1 | CMT2 | Other CMTs | ns CMTs | |
|---|---|---|---|---|
| Number of patients | 42 | 12 | 8 | 40 |
| Confirmed diagnosis | 85.7% (36) | 33.3% (4) | 37.5% (3) | 37.5% (15) |
| Mean age at 1st MFM (years) | 30.4 ± 19.7 (4.3–67.8) | 33 ± 25.4 (6.4–79.3) | 25.9 ± 21.8 (4.3–54.9) | 27.8 ± 23.3 (6.25–79.3) |
| Time between MFM 1 and MFM 2 (months) | 17.6 ± 8 (7–30.5) | 27.3 ± 17 (14–74) | 18.6 ± 5.5 (11.5–29.5) | 20.8 ± 13.7 (6.5–62) |
| MFM D1 score | ||||
| Mean annual score change | −3.00 ± 9.05 | −2.15 ± 3.17 | −0.49 ± 3.80 | 0.44 ± 7.58 |
| SRM | 0.32 | 0.68 a | 0.13 | −0.06 |
| MFM D2 score | ||||
| Mean annual score change | −1.03 ± 2.18 | 0.07 ± 1.01 | −0.01 ± 0.04 | −1.31 ± 3.23 |
| SRM | 0.47 | −0.07 | 0.35 | 0.41 |
| MFM D3 score | ||||
| Mean annual score change | −0.71 ± 6.4 | −1.98 ± 3.99 | −0.10 ± 4.72 | 0.35 ± 3.62 |
| SRM | 0.11 | 0.50 a | 0.02 | −0.1 |
| MFM total score | ||||
| Mean annual score change | −1.78 ± 5.56 | −1.28 ± 1.51 | −0.22 ± 2.09 | −0.24 ± 3.51 |
| SRM | 0.32 | 0.85 a | 0.11 | 0.07 |
On the average, the 102 patients underwent 2.9 MFMs (2–6), and mean duration between 2 MFMs was 20 months ± 11.8 (6.5–62). The time between 2 MFMs was longer for CMT2 patients: 23.7 ± 17 months vs. 17.6 ± 8 than for CMT1, 18.6 ± 5.5 for other CMTs and 20.8 ± 13.7 for the non-specified CMTs. pour les ns CMTs.
There existed a progressive diminution of total MFM score in CMT1 patients (–1.78 ± 5.56 points a year), other CMTs (–0.43 ± 2.17 points a year) and ns CMTs (–0.24 ± 3.51 points a year). However, the standardized response mean (SRM) values remained low (< 0.50) ( Table 2 ). In the CMT2 patients, there was a diminution considered as significant in the sub-scores D1 (SRM = 0.68), D3 (SRM = 0.50) and, more particularly, TS (SRM = 0.85).
1.4
Discussion
The MFM is a recent functional scale that has been validated with regard to most neuromuscular diseases (NMD) . While it has already been studied in some diagnostic groups, particularly Steinert’s myotonic dystrophy and spinal muscular atrophy , it had never to our knowledge been specifically analyzed with regard to CMT.
Responsiveness study has shown a significant decrease over time of MFM for the different forms of NMD. In this work, Duchenne’s muscular dystrophy (DMD) patients constituted the largest NMD sub-group (41 patients), while patients suffering from hereditary neuropathy were represented by only 17 patients. The standardized response mean was significant in the DMD group, but not in the hereditary neuropathy group. In this study, it was suggested that MFM was able to detect a change for a period lasting at least two years.
Our study has shown that motor function in patients suffering from CMT, which is a gradually progressive disease with a high degree of clinical heterogeneity, can be effectively appraised using MFM, whatever the age and the diagnostic group of the CMT patients. Its responsiveness has been tested in 102 patients ranging in age from 4 to 80 years. As expected, CMT1 and CMT2 patients were heavily represented in our sample (CMTIA is the most frequently encountered form). Even though mean annual lowering of the TS, D1 and D3 MFM scores was observed in all the diagnostic groups, only in CMT2 patients did responsiveness reach significance (SRM = 0.68 for D1, = 0.5 for D3 and 0.85 for TS). Since the results recorded using the MFM cannot be compared with an external indicator such as the “Clinical Global Impression” (CGI) scale, it is not possible to determine whether or not the above-mentioned statistically significant differences have clinical relevance. As a matter of comparison, it has been shown in study of MFM responsiveness that a change of 5 points in the total MFM score was perceptible by the patient or his therapist ; even if the changes we have observed are significant with regard to D1 and D3, they remain inferior to the threshold of 5 points, which means that for the patient, their clinical relevance is hardly indisputable.
While several studies have shown that clinical signs or symptoms conclusively distinguishing CMT1 from CMT2 patients do not exist , our results are in agreement with those reported by Chung et al. and Ribiere et al., who demonstrated more severe disease (higher CMTNS scores) in CMT2A than in CMT1A patients, a finding explained by greater loss of sensitivity to pain in CMT2A patients .
Study of MFM sub-scores enables more precise description of the natural course of the disease, and the sub-scores for D1 and D3 appeared particularly interesting to analyze in CMT patients. In our CMT population, the D1 sub-score (standing position and transfers) was the first to be affected, and also the most pronouncedly. Contrarily to the other sub-scores, a substantial ceiling effect was observed for the D2 sub-score representing axial and proximal motor function (62.7% of the patients evaluated had a D2 sub-score of 100%). More precisely, the D2 sub-score was close to 100% in young subjects and underwent hardly any modification during disease development. These results are in congruence with clinical observations CMT, which is first and foremost a peripheral pathology.
Our results show that age was correlated with functional outcome for the D1 and D3 sub-scores and that there existed no significant difference in disease development according to types of CMT. It should be noted that a number of patients were over 60 years of age. While MFM has been validated for a population ranging in age from 6 to 60 years, life expectancy is higher in CMT than with regard to other NMDs, and the scale consequently appears altogether suited for follow-up in a more aged population.
In our population, MFM underscored a significant difference in disease development and outcome between ambulatory and non-ambulatory patients. Our results confirm the discriminative acuity of this scale, which can be applied whatever the severity of the disease and the status of the patient.
In our study, only 4.3% of the patients required respiratory assistance. That said, while pulmonary damage in CMT patients is relatively rare, it should be assessed using respiratory function tests such as the cardio-pulmonary effort test (CPET) on a treadmill with the objectives of studying oxygen consumption during the exercise (VO2), forced vital capacity (FVC), forced expiratory volume (FEV1), mean expiratory flow, functional residual capacity, maximum per-minute ventilation, breathing and heart rates as well as the anaerobic threshold. As the MFM scale does not take patient respiratory function into account, we are convinced it would be useful to supplement patient evaluation with respiratory function evaluation.
1.5
Study limitations
CMT with a non-specified diagnosis (ns CMT) represented a substantial number of patients (n = 100), and probably included different types of CMT. It is consequently difficult to compare this CMT group with the other groups. It would be interesting to more precisely identify the “miscellaneous” types of CMT so as to carry out a new study with more precisely delineated samples.
Another limit consisted in the highly variable time interval between two MFMs, which was the reason for which we calculated an annual trend line slope.
The number of patients present in the MFM databases is constantly growing. It would surely be interesting to proceed to a more in-depth study of MFM responsiveness once a higher number of patients shall have undergone several MFMs over longer time intervals; this would allow researchers to more effectively focus on a specific diagnostic category.
1.6
Conclusion
This study has shown that the MFM scale is applicable and suitable for CMT patients. It has evidenced a progressive lowering of scores and sub-scores according to age. That much said, it is recommended to take into account not the total score, but rather the different MFM sub-scores, of which D1 and D3 have been shown to contribute more information than D2. Finally, as concerns responsiveness or sensitivity to change, MFMs should not be carried out at overly short intervals; after all, CMT remains a slow, progressive disease.
The MFM scale is a useful tool allowing for enhanced evaluation of the long-term effectiveness of a given treatment, and it could be used, complementarily to other scales such as the CMTNS or the NIS, during therapeutic trials.
This work constitutes the first step of a process designed to validate the MFM scale on CMT patients. In order to successfully complete it, criterion validity and construct validity remain to be analyzed.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgements
First we wish to thank the CMT patients and their families.
We also wish to thank the CMT study group, which consists in the French and Swiss centers that included CMT patients in the MFM data base: G. Rode (médecine physique et réadaptation, hôpital Henry Gabrielle, hospices civils de Lyon, France), C. Bérard (service central de rééducation pédiatrique – L’Escale, hôpital femme mère enfant, hospices civils de Lyon, France), fondation Richard, centre d’éducation motrice et centre pour adultes, Lyon, France, S. Ragot-Mandry (service de rééducation pédiatrique, hôpital d’enfants de Brabois, Nancy, France), L. Féasson (service de rééducation, hôpital Bellevue, Saint Etienne, France), M. Fournier-Méhouas and C. Richelme (service de rééducation adulte, Hôpital de l’Archet, Nice, France), J.Y. Salle and M. Munoz (service de rééducation adulte, hôpital universitaire Dupuytren, Limoges, France), J.Y. Mahé (centre de rééducation de Pen, Bron, La Turballe, France), J.P. Gayraud (Centre Paul Dottin, Ramonville, France), F. Cottrel et C. Thémar-Noel (institut de myologie, Hôpital Pitié-Salpêtrière, Paris, France), P.Y. Jeannet (service de rééducation, centre hospitalier universitaire Vaudois, Lausanne, suisse), V. Tiffreau (centre de référence des maladies neuromusculaires, hôpital Swynghedauw, CHRU Lille, France), B. Berger and P. Bonnet (service de rééducation, hôpital Michallon, CHRU de Grenoble, France), A. Urtizberea (centre de référence neuromusculaire GNMH, hôpital Marin, Hendaye, France), S. Pellieux (médecine physique et réadaptation, centre Trousseau, Tours, France) and D. Pichancourt (médecine physique et de réadaptation enfants et adolescents, hôpital Trestel, Lannion, France).
2
Version française
2.1
Introduction
La maladie de Charcot-Marie-Tooth (CMT) est une des maladies neuromusculaires (MNM) héréditaires les plus fréquentes, avec une prévalence de 1 sur 2500 personnes en France . Il s’agit d’un groupe de maladies caractérisées par une atteinte des nerfs des jambes et des bras (nerfs périphériques), qui présente une grande hétérogénéité génétique, avec plus de 30 gènes potentiellement responsables . Les patients atteints de CMT sont classés en sous-formes selon l’atteinte nerveuse et le mode de transmission (CMT1 : forme démyélinisante, autosomique dominant ; CMT2 : forme axonale, autosomique dominant ou récessif ; CMT4 : forme démyélinisante, autosomique récessif, CMTX : forme liée au chromosome X et IAD : forme intermédiaire autosomique dominante) et présentent des tableaux cliniques très variables (atrophie des muscles péroniers, atteinte des muscles intrinsèques des mains, aréflexie, déformation des pieds…). L’évolution est souvent lentement progressive et l’âge de début des symptômes extrêmement variable d’un individu à l’autre .
Si à ce jour aucun traitement médicamenteux dans la CMT n’est disponible, des études réalisées sur des modèles animaux ont donné des résultats encourageants et des essais ont été ou seront prochainement menés chez l’homme. Ainsi, les effets chez l’homme de l’acide ascorbique, de la progestérone et ses dérivés, de la neurotrophine 3 ou du curcumin ont déjà été étudiés. Afin d’étudier précisément l’effet de thérapeutiques chez l’homme, des outils d’évaluation valides, sensibles et reproductibles sont nécessaires. Sur le plan clinique, l’évaluation fonctionnelle permet d’améliorer le suivi des patients sur le long terme ainsi que les connaissances sur l’évolution naturelle de la maladie. Une évaluation fonctionnelle peut permettre d’anticiper et de prévenir certaines conséquences de la maladie de manière à adapter la prise en charge et mettre en place des aides techniques adéquates.
Le 168th ENMC International Workshop de 2010 a permis de faire le point sur les outils d’évaluation disponible dans la CMT . Parmi les outils d’évaluation de patients CMT, les plus couramment utilisés sont le CMT neuropathy score (CMTNS) , seule mesure spécifique de la CMT, et la neuropathy impairment score (NIS) . La CMTNS et la NIS ont été validées chez des patients âgés de 10 ans et plus. La CMTNS prend en compte les données de l’examen neurologique, les données de l’électromyogramme, la sensibilité, et la force musculaire et l’échelle NIS est une échelle standard qui évalue 24 groupes musculaires, 5 réflexes ostéotendineux et les troubles sensitifs évalués à la face dorsale de la dernière phalange de l’index et du gros orteil. L’évolution naturelle de la CMT a été étudiée avec la CMTNS et la NIS uniquement chez les CMT1A et CMTX. Ces échelles ont montré leur capacité à détecter un changement et une progression de la CMT1A et les auteurs recommandaient d’étudier l’évolution des autres types de CMT avec cet outil .
La CMT est une maladie débutant en général dans la première décade, une échelle pédiatrique a ainsi été développée, la CMT Pediatric Scale (CMTPedS) . Cette échelle est bien tolérée, fiable, reproductible. Cependant, n’étant utilisable que chez les enfants, cette échelle ne permet pas un suivi longitudinal après la transition chez l’adulte.
La mesure de la fonction motrice (MFM) est une échelle précise et validée pour la plupart des MNM. Elle permet d’objectiver le retentissement de la faiblesse musculaire dans la fonction motrice et est adaptée à la plupart des MNM quel que soit le degré de gravité de la maladie. Cette échelle existe en deux versions, l’une composée de 32 items, validée pour des patients atteints de maladies neuromusculaires âgés de 6 à 60 ans (MFM-32), l’autre composée de 20 items (MFM-20) validée chez des enfants âgés de 2 à 6 ans . Les études de validation des MFM-32 et MFM-20 ont permis de distinguer 3 domaines de fonctions motrices :
- •
D1 : station debout et transferts (13 items pour la MFM-32 et 8 pour la MFM-20) ;
- •
D2 : motricité axiale et proximale (12 items pour la MFM-32 et 8 pour la MFM-20) ;
- •
D3 : motricité distale (7 items pour la MFM-32 et 4 pour la MFM-20).
L’étude de validation princeps de la MFM-32, conduite dans une population de 303 patients porteurs d’une MNM, dont 35 étaient atteints de neuropathie périphérique, avait permis de démontrer les propriétés métrologiques robustes de cet outil et des études ultérieures ont conclu à sa validité et à sa sensibilité au changement dans différents groupes de patients atteints de MNM .
L’avantage que présente la MFM-32, contrairement aux échelles CMTNS, NIS et CMTPedS, est qu’elle est applicable aux patients âgés de 6 à 60 ans et qu’elle ne prend pas en compte les données de l’électromyogramme qui reste un examen invasif et difficile à réaliser à chaque consultation.
L’objectif de ce travail est d’étudier l’applicabilité et la sensibilité au changement (pour le score total et les trois sous-scores, D1, D2 et D3) de la MFM chez des patients atteints de CMT.
2.2
Patients et méthodes
2.2.1
Design de l’étude
Il s’agit d’une étude de cohorte observationnelle multicentrique.
2.2.2
Population de l’étude
Les patients inclus dans l’étude étaient âgés d’au moins 4 ans, atteints de CMT (suspecté ou confirmé par analyse génétique) et ayant donné leur accord afin que des données médicales les concernant puissent être utilisées en recherche clinique.
Les patients ont été classés selon les groupes diagnostiques suivant : CMT1, CMT2, CMT autres (CMT4, CMTX et IAD) et CMT ns (non spécifié).
2.2.3
Recueil des données
Les données recueillies dans notre étude étaient issues de la base de données MFM. Cette base de données est disponible gratuitement sur Internet depuis 2007 et permet aux différents services participants d’entrer de façon sécurisée les données MFM de leurs patients (pour plus d’informations, consulter www.mfm-nmd.org ).
Les données recueillies comprenaient les scores des différents items de la MFM, la date de passation, la date de naissance des patients, le sexe, les antécédents chirurgicaux, la présence d’une ventilation ou non, le statut ambulant ou non (un patient est considéré comme ambulant si il est capable de faire 10 pas à l’intérieur sans assistance humaine, avec ou sans aide technique ou appareillage), l’âge d’apparition des premiers symptômes.
2.2.4
Services participants
Quinze services français et un service suisse de médecine physique et réadaptation, de neurologie et/ou consultations dans un centre de référence des maladies neuromusculaires ont inclus au moins un patient CMT dans la base de données MFM entre janvier 2007 et avril 2013.
2.2.5
L’échelle MFM
La MFM est une échelle générique évaluant la fonction motrice des enfants et adultes porteurs d’une maladie neuromusculaire. La MFM-32 a été validée chez des patients MNM âgés de 6 à 60 ans et comporte 32 items répartis en 3 sous-scores :
- •
D1 (station debout et transferts) ;
- •
D2 (motricité axiale et proximale) ;
- •
D3 (motricité distale).
L’étude initiale de validation de la MFM n’avait pas pris en compte le développement psychomoteur du jeune enfant ; la durée de passation de l’échelle et la complexité de certains de ses items n’étaient pas adaptées à de jeunes patients. Une version courte de la MFM-32, la MFM-20 composée de 20 items de la MFM-32, s’adressant spécifiquement aux enfants âgés de 2 à 7 ans a été développée .
La cotation de la MFM utilise une échelle de Likert en 4 points évaluant les capacités maximales du sujet sans l’aide d’une tierce personne. La cotation est 0 = n’initie pas le mouvement ou la position de départ ne peut être maintenue, 1 = réalise partiellement l’exercice, 2 = réalise complètement l’exercice, mais avec difficulté, compensations ou lenteur, 3 = réalise complètement et « normalement » l’exercice. Le score total varie de 0 à 100 % en additionnant toutes les cotations attribuées aux différents items de la MFM.
2.2.6
Statistiques
Les variables quantitatives ont été décrites en utilisant des moyennes, des déviations standard (SD) et des intervalles. Les variables qualitatives ont été décrites en utilisant des nombres et des pourcentages.
Les effets plancher et plafond ont été analysés respectivement en calculant le pourcentage de la population ayant un score MFM de 0 % et le pourcentage de la population ayant un score MFM de 100 %. Des pourcentages inférieurs à 20 % étaient considérés comme acceptables.
Les relations entre les scores MFM et l’âge des patients ont été analysées en utilisant un modèle de régression linéaire.
Les scores moyens des MFM ont été analysés par catégories diagnostiques et selon le statut ambulant des patients. Une analyse de variance (Anova) a été utilisée afin de mettre en évidence une différence significative entre groupes.
La sensibilité au changement a été étudiée chez les patients ayant été évalués au moins 2 fois par la MFM, avec un délai entre la première et la dernière MFM d’au moins 6 mois. Pour chaque patient, les mesures répétées des scores MFM D1, D2, D3 et du score total (TS) ont été résumées par la pente de changement exprimée en taux annuel en utilisant le unweighted least-square estimate . Ces pentes ont ensuite été exprimées en tant que standardized response mean (SRM) en calculant les rapports entre la moyenne des pentes de changement divisée par l’écart type de la moyenne. Ces valeurs de SRM ont été considérées comme élevées si > 0,80, modérées si allant de 0,50 à 0,79, et faibles si < 0,50 .
2.3
Résultats
2.3.1
Caractéristiques de la population
Au total, 25 MFM-20 et 407 MFM-32 provenant de 233 patients atteints de CMT, 111 hommes et 122 femmes, âgés de 4 à 86 ans ont été enregistrées dans la base de données MFM. Les caractéristiques des patients le jour de leur première passation d’une MFM sont décrites dans le Tableau 1 .








