Abstract
Objectives
If the benefits of single-event multilevel surgery (SEMS) in ambulatory children with cerebral palsy have already been validated, especially in terms of functional outcomes, fewer studies have evaluated SEMS in terms of quality of life and satisfaction with surgical outcomes, especially pertaining to the opinions of children and their family. The objectives of this study were to confront the perceptions of parents and the experience of their operated children in terms of quality of life and surgical outcomes.
Materials and methods
This was an observational, descriptive, single-center study conducted in a regional Pediatric Physical Medicine and Rehabilitation (PM&R) center, which is considered a reference center in this region of France. The subjects recruited were ambulatory children with cerebral palsy (CP) who had SEMS between 2009 and 2011, and one of their parents. The specific “child” and “parent” CP-related modules of the DISABKIDS questionnaire were used to assess these children’s quality of life post-surgery. Perceptions of parents and children regarding gait evolution and satisfaction with surgical outcomes were analyzed via a questionnaire developed by the author. Regarding quality of life and surgical outcomes, the correlation between the perception of parents and experience of children was estimated using the intraclass correlation coefficient (ICC) or prevalence-adjusted bias-adjusted kappa values (PABAK).
Results
Twelve children (83% of them boys) and their parents participated in the study. For the DISABKIDS questionnaire, a moderate correlation was found regarding functional impact (ICC = 0.58; P < 0.0178) but a high correlation was reported for the communication item of the questionnaire (ICC = 0.73; P = 0.0025). Regarding satisfaction with surgical outcomes, results showed a good correlation (PABAK = 0.64).
Conclusion
Concerning quality of life and satisfaction with surgical outcomes, our study showed a good or even high correlation between parents’ perceptions and their child’s experience. It is however essential to privilege the child’s opinion whenever possible.
Résumé
Objectif
Alors que les bénéfices de la chirurgie multi-étagée chez l’enfant paralysé cérébral marchant sont connus notamment en termes de résultats fonctionnels, ils le sont moins en termes de qualité de vie et satisfaction vis-à-vis de ce type de chirurgie, notamment en prenant en compte à la fois le point de vue de l’enfant et du parent. L’objectif était d’évaluer le niveau de concordance entre la perception des parents et celles des enfants opérés, concernant la qualité de vie des enfants et la satisfaction après cette chirurgie.
Matériels et méthodes
Étude observationnelle à visée descriptive monocentrique, réalisée dans un centre de médecine physique et de réadaptation pédiatrique de référence au niveau régional, auprès d’enfants paralysés cérébraux marchants ayant bénéficié d’une chirurgie multi-étagée entre 2009 et 2011, et un de leur parent. Les versions « enfant » et « parent » du module spécifique à la paralysie cérébrale (PC) du questionnaire DISABKIDS ont été utilisées pour évaluer la qualité de vie des enfants. La perception de l’évolution de la marche et la satisfaction après chirurgie a été évaluée par un questionnaire rédigé par l’auteur. La concordance parent–enfant a été estimée par le coefficient de corrélation intraclasse (CCI) ou le coefficient de kappa ajusté sur la prévalence (PABAK).
Résultats
Douze enfants (83 % de garçons) et leur parent ont participé. Une concordance modérée entre les réponses des parents et des enfants au DISABKIDS était retrouvée pour le domaine impact fonctionnel (CCI = 0,58 ; p < 0,0178) et importante pour le domaine communication (CCI = 0,73 ; p = 0,0025). Concernant la satisfaction, la concordance était jugée bonne (PABAK = 0,64).
Conclusion
En ce qui concerne l’évaluation de la qualité de vie et la satisfaction, un bon, voire excellent niveau de concordance parent–enfant était observé. Il est important de considérer l’avis des enfants aussi souvent que possible.
1
English version
1.1
Introduction
The prevalence of cerebral palsy (CP) ranges between 1.7 and 2.5 per 1000 live births in European and North American countries . This chronic pathology leads to frequent motor disabilities, especially severe gait impairments.
Initially, the child presents with a normal musculoskeletal system and non-progressive but irreversible brain damage. The consequences of this brain damage, called “primary impairments”, consist of several symptoms, such as loss of muscle tone, motor control and balance disorders, as well as spasticity (in most types of CP). Later on, muscle and tendon contractions and impairments of the musculoskeletal system appear. “Secondary impairments” are caused by abnormal mechanical stimulations imposed on a growing musculoskeletal system . Children try to walk in spite of their primary and/or secondary structural and dynamic impairments. The prevention and treatment of these impairments are based on physical therapy, medical treatment, orthotics, injections of botulinum toxin and surgery.
Surgical management for CP, including tendon lengthening and/or transfers, derotational osteotomy or joint stabilization, has always had a functional improvement objective. For a long time, it has been performed in a limited and successive manner in fear of doing too many surgical procedures that would yield to irreversible consequences .
Recently, single-level surgery has been replaced by the concept of multilevel surgery consisting of two teams operating simultaneously on both of the patient’s lower limbs during one single surgical procedure; thus, requiring only one hospitalization and one post-surgical rehabilitation stay.
The effectiveness of multilevel surgery has been validated in several studies, which have underlined the reduced number and total duration of hospitalizations during childhood, improvement in gait parameters, joint range of movement, decreased energy cost when walking, as well as improvement in functional abilities evaluated via the Gross Motor Function Measure (GMFM) .
Numerous studies lately have been focusing on assessing the functional results of this surgery, however, very few studies have evaluated the quality of life and satisfaction after this type of surgery. One should underline that the opinion of children is rarely studied in today’s literature.
The main objective of this study was to evaluate the correlation between the perception of parents and experience of children regarding quality of life and satisfaction with multilevel surgical outcomes. The secondary objective was to describe the perception of children regarding the evolution of their general state and most specifically gait abilities.
1.2
Material and methods
1.2.1
Study design
Descriptive, observational, single-center study conducted in a Pediatric Physical Medicine and Rehabilitation (PM&R) center of reference. Recruited subjects were ambulatory children with cerebral palsy who had multilevel surgery. The evaluation was done based on self-assessment questionnaire and semi-directed interviews. This study was approved by the local Ethics committee and all parents signed an informed consent form before study inclusion.
1.2.2
Characteristics of the studied population
The following inclusion criteria for the study were:
- •
children diagnosed with cerebral palsy and ambulatory capacities [Gross Motor Function Classification Scale (GMFCS) I to III];
- •
children aged < 18 years old at the time of surgery;
- •
children who had multilevel surgery in the Lorraine regional university hospital center between 2009 and 2011. To be defined as multilevel surgery, the procedure had to include in a single surgical procedure at least two muscle–tendon (lengthening or transfer) or bone surgical gestures on one or two limbs;
- •
children who spent their post-surgical rehabilitation in the regional reference PM&R center of Lorraine, France.
Exclusion criteria were children with mild intellectual disability (intelligence quotient below 70), as well as children and/or parents who refused to participate to the study.
1.2.3
Collected data
All data were collected between November 2012 and May 2013, by the team who took care of the child, during a half-day evaluation of the multilevel surgical outcomes. Children and the parent present during this evaluation filled out, independently, a self-assessment questionnaire on the child’s quality of life. They also participated in a semi-directed interview regarding their satisfaction pertaining to surgical outcomes and perception of gait evolution. Furthermore, surgical-related data were collected from the patients’ medical charts.
1.2.3.1
Demographics and surgical data
Based on the interview with the families and the patient’s medical chart, the following data were collected: sex, age, educational attainment at the time of the study, type of cerebral palsy, GMFCS levels before and after surgery, age at the time of surgery, number of surgical procedures, levels of surgery, time elapsed between surgery and the study, duration of post-surgical rehabilitation in the PM&R center.
1.2.3.2
Quality of life
The children and adolescents who had multilevel surgery as well as one of their parents filled out the specific cerebral palsy module of the DISABKIDS questionnaire .
DISABKIDS is a quality of life questionnaire designed for children with chronic conditions; it is validated and has been translated in six European languages, including French . Several versions of the questionnaire are available, i.e. the long version (37 items) evaluating the following three domains: mental (sub-scales: independence and emotion), social (sub-scales: inclusion and exclusion) and physical (sub-scales: limitations and medications) , the short version (12 items) evaluating the same domains, and finally, the version designed for children under the age of 7 using smileys (7 items). Furthermore, 7 modules specific to chronic conditions exist, including one for cerebral palsy , the latter consists of 12 items divided into two dimensions, i.e. functional impact of the disease and communication. Each module has a “child” and “parent” version. A score was obtained for each of the dimensions that ranged from 0 to 100 (100 meaning the best quality of life possible).
1.2.3.3
Satisfaction with surgical outcomes and perception of gait evolution
In order to know if patients and their parent were satisfied with this type of surgery and if they perceived a subjective improvement of their general state, the PM&R physician in charge of the study conducted a semi-directed interview with children and their parent asking questions related to gait evolution, which is the main improvement objective for this type of surgery. This interview included 16 questions:
- •
two closed-ended question (Yes/No) pertaining to satisfaction and whether in hindsight they would agree again to having the surgery;
- •
fourteen questions pertaining to changes to the child’s general state and gait evolution, these closed-ended questions all had the same answer modalities (agree/do not agree/do not know).
Children and their parent were invited to comment their answers. Participants also needed to give a global satisfaction score between 0 and 10.
1.2.4
Statistical analysis
All data collected were the object of a descriptive analysis, with quantitative variables expressed in mean (± standard deviation) and qualitative variables expressed in numbers ( n ) and percentages (%).
The scores of the 2 dimensions of the CP-specific module of the DISABKIDS were computed for children and their parents. The intraclass correlation coefficient (ICC) was used to calculate the correlation for continuous variables between parents and children. For qualitative variables, the correlation was estimated by the prevalence and bias-adjusted kappa (PABAK) comprised between –1 and +1 associated to the prevalence index (PI) and bias index (BI).
A bias between the judges (BI) exists when a response modality is more reported by one person than the other. The prevalence index (PI) exists when an answer is overly reported by children or their parents. This was the case in this study so we used PABAK .
The interpretation of the ICC and PABAK indexes is based on the Landis and Koch classification, i.e.:
- •
0.21 to 0.40 low correlation;
- •
0.41 to 0.60 moderate correlation;
- •
0.61 to 0.80 good correlation;
- •
0.81 to 1.00 excellent correlation .
We used the SAS 9.3 software for the statistical analysis [SAS Inst., Cary, NC]. Differences were considered significant at P < 0.05.
1.3
Results
1.3.1
Demographics
Overall 19 patients were eligible for the study. Three children were lost to the touch (two moved to another region, one patient remained unreachable). After having delivered complete information on the study, 4 parents refused for their children to participate. The main reasons were: previous involvement in other studies, medical care management already requiring too much time and thus refusing additional appointments. In the end, 12 families were enrolled in the study.
The main demographic and surgical characteristic of the 12 children who participated in the study are listed in Table 1 .
| Demographics and clinical data | Surgical data | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pat. | Sex | Age at study (years) | Educational attainment | Type of CP | GMFCS before | GMFCS after | Age at surgery (years) | Procedures ( n ) | Levels ( n ) | Time between surgery and the study (months) | Duration of PM&R stay (months) |
| A | M | 19 | Special class middle school level | Diplegia | III | III | 14 | 10 | 3 | 54 | 9 |
| B | M | 19 | Liberal Arts college | Diplegia | I | I | 17 | 7 | 2 | 26 | 2 |
| C | M | 15 | 8th grade + special class | Diplegia | II | I | 13 | 6 | 2 | 21 | 3 |
| D | M | 21 | Community college | Diplegia | III | III | 18 | 16 | 3 | 39 | 9 |
| E | F | 16 | 11th grade | Diplegia | III | III | 11 | 8 | 2 | 55 | 7 |
| F | M | 13 | 7th grade | Diplegia | II | II | 12 | 7 | 3 | 12 | 5 |
| G | M | 18 | Special class middle school level | Diplegia | II | II | 14 | 6 | 2 | 34 | 10 |
| H | M | 20 | Stopped school, special class before | Diplegia | III | III | 18 | 9 | 3 | 23 | 3 |
| I | M | 18 | 10th grade | Diplegia | III | III | 14 | 8 | 3 | 41 | 3 |
| J | M | 16 | 12th grade | Hemiplegic left side | I | I | 14 | 7 | 2 | 17 | 8 |
| K | F | 13 | 6th grade | Hemiplegic left side | I | I | 11 | 3 | 2 | 22 | 4 |
| L | M | 13 | 7th grade | Diplegia | III | III | 12 | 14 | 3 | 17 | 2 |
Children who participated in the study, including 83% of boys, had a mean age of 14 at the time of surgery ( R ; 11–18) and a mean delay of 2.5 year between surgery and the day of the functional assessment.
The day of the functional assessment, 6 children (50%) were GMFCS level 3, two were GMFCS level 2 and four were GMFCS level 1. Ten children presented with spastic diplegia CP and 2 with hemiplegic CP. Seven children/adolescents were in a normal school program, 4 children had special assistance in school and one patient was out of school.
In average, the surgery included 8 procedures with at least one bone procedure and one muscle–tendon procedure. Six patients benefited from a 3-level surgery (hip, knee and ankle-foot) and the other 6 children had a 2-level surgery. The mean postoperative hospitalization in a PM&R center was 6 months ( R : 2–10 months).
1.3.2
Quality of life
The DISABKIDS questionnaire was completed by the 12 families. The quality of life scores of the two dimensions of the DISABKIDS reported by children and their parents are presented in Fig. 1 .
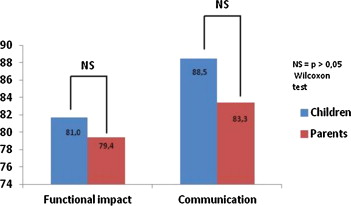
For the functional impact domain, mean scores were 81.0 (min: 57.5; max: 97.5; SD: 13.7) and 79.4 (min: 65; max: 92.5; SD: 9.8) for children and parents, respectively. Regarding the communication domain, mean scores were 88.5 (min: 37.5; max: 100; SD: 22.3) and 83.3 (min: 37.5 max: 100; SD: 26.3) for children and parents, respectively. There was no statistically significant difference between the score reported by parent and the one reported by their children (functional impact P = 0.58 and communication P = 0.61) ( Fig. 1 ).
There was a moderate parent–child correlation for the functional impact domain (ICC = 0.58; P < 0.0178) and a high correlation for the communication domain (ICC = 0.73; P < 0.0025). In the functional impact domain, 7 parents out of 12 underestimated the quality of life perceived versus the quality of life reported by their child, and 5 parents overestimated it. Regarding the communication domain, 11 parents had exactly the same perception as their child and 1 parent underestimated his/her child’s perception.
1.3.3
Satisfaction towards surgery
One parent did not answer the questions during the semi-directed interview because of time constraints.
Regarding satisfaction, 92% of children and 91% of parents were satisfied with the surgical outcomes with a good parent–child correlation (PABAK: 0.64).
The mean global satisfaction rate was 8.3/10 for parents and children. There was a moderate correlation between the satisfaction score for parents and children (ICC = 0.52; P = 0.04).
Overall, 83% of children and 91% of parents would in hindsight agree to have the surgery again. The reasons regularly brought forward were that surgery either improved gait or it prevented further loss of gait abilities. Several children or parents noticed an improvement in self-confidence, especially in the way others looked at them. However, most described a long and difficult journey from the surgery procedure and time spent in the rehabilitation center in order to achieve maximum improvement.
1.3.4
Perception of the evolution of the children’s general state and most specifically gait
Results, issued from the semi-directed interview pertaining to the perceived changes regarding the child’s general state and gait, are presented in Table 2 . For all these questions, the PABAK coefficient ranged between –1 and +1.
| Since surgery | Children | Parents | PABAK | PI | BI | ||||
|---|---|---|---|---|---|---|---|---|---|
| Agree n (%) | Disagree n (%) | Do not know n (%) | Agree n (%) | Disagree n (%) | Do not know n (%) | ||||
| Life is easier | 10 (83.3) | 2 (16.7) | 0 (0) | 7 (63.6) | 4 (36.4) | 0 (0) | 0.64 | 0.45 | 0.18 |
| Falls are less frequent | 8 (66.7) | 4 (33.3) | 0 (0) | 8 (72.7) | 3 (27.3) | 0 (0) | 0.64 | 0.45 | 0.00 |
| Possibility to stand up for longer periods of time | 8 (66.7) | 3 (25) | 1 (8.3) | 9 (81.8) | 2 (18.2) | 0 (0) | 0.78 | 0.44 | 0.11 |
| Possibility to walk for longer periods of time | 11 (91.7) | 1 (8.3) | 0 (0) | 9 (81.8) | 2 (18.2) | 0 (0) | 0.82 | 0.73 | 0.09 |
| Easier to wear shoes | 3 (25) | 8 (66.7) | 1 (8.3) | 3 (27.3) | 8 (72.7) | 0 (0) | 0.50 | 0.25 | 0.25 |
| Pain is less intense | 5 (41.7) | 7 (58.3) | 0 (0) | 4 (36.4) | 7 (63.6) | 0 (0) | –0.27 | –0.27 | 0.00 |
| A new physical activity has been started | 5 (41.7) | 7 (58.3) | 0 (0) | 4 (36.4) | 7 (63.6) | 0 (0) | 0.82 | –0.18 | 0.10 |
| Increased gait speed | 8 (66.7) | 4 (33.3) | 0 (0) | 9 (81.8) | 2 (18.2) | 0 (0) | –1.00 | 0.00 | 1.00 |
| Walking is less tiring | 10 (83.3) | 2 (16.7) | 0 (0) | 8 (72.7) | 3 (27.3) | 0 (0) | 1.00 | –1.00 | 0.00 |
| Knees can better extend during gait | 11 (91.7) | 1 (8.3) | 0 (0) | 11 (100) | 0 (0) | 0 (0) | 0.82 | –0.91 | –0.10 |
| Knees are less turned inwards | 12 (100) | 0 (0) | 0 (0) | 10 (90.9) | 1 (9.1) | 0 (0) | 0.82 | –0.91 | –0.10 |
| Easier to put the foot flat on the ground while walking | 11 (91.7) | 1 (8.3) | 0 (0) | 9 (81.8) | 2 (18.2) | 0 (0) | 1.00 | –1.00 | 0.00 |
| Less feet dragging when walking | 10 (83.3) | 1 (8.3) | 1 (8.3) | 9 (81.8) | 2 (18.2) | 0 (0) | –1.00 | 0.00 | 1.00 |
| Feet are less turned inwards | 12 (100) | 0 (0) | 0 (0) | 10 (90.9) | 1 (9.1) | 0 (0) | 0.82 | –0.91 | –0.10 |
In fact, 83% of children reported that their life was easier since surgery. They underlined that they felt better about themselves, less disabled, that moving around was easier and that overall “everything was a little easier”.
Children who used to fall before surgery (67%) reported that falls were less frequent or absent all together. Overall, children perceived that they were able to stand up (66.7) and walk (91.7) for longer period of times.
Among the 4 patients who wore orthopedic shoes prior to surgery, 2 of them were able to get rid of the shoes after surgery.
For the 9 patients (75%) who reported pain before surgery, 5 of them perceived being in less pain, whereas 4 thought they were in more pain.
Overall for the 12 children, 5 of them had started a new physical activity since surgery. Most children thought they were walking faster (66.7%), that walking required less energy (83.3%), they perceived that their knees (100%) and feet (100%) were less turned inwards, and that they were better able to put their feet flat on the floor (91,7%), and that during gait their feet were dragging less on the floor (83,3%).
1.4
Discussion
The parent–child correlation level pertaining to the perception of the children’s quality of life and their satisfaction regarding multilevel surgery was studied in a population of ambulatory CP children.
Main results showed a good correlation between what parents and children reported regarding quality of life and satisfaction following multilevel surgery.
Quality of life (QoL) was evaluated using the specific cerebral palsy module of the DISABKIDS questionnaire because of technical constraints and the association of this scale with the questions of the semi-directed interview. In order to obtain the most relevant QoL measure, it was decided to only use the specific CP module rather than the generic long version. The DISABKIDS questionnaire authors consider the specific cerebral palsy module to be “a specific, cost-effective and readily available tool to evaluate the quality of life of children with cerebral palsy and that can be used in interventional studies” (DISABKIDS guide).
This QoL scale is one of the rare sales specifically designed for cerebral palsy . To this day, it is the only one translated and validated in French.
No study using the specific CP module of the DISABKIDS questionnaire was found in the literature, thus, limiting the possibility of comparing our results.
As a matter of fact, this study is the first pertaining to the parent–child correlation regarding satisfaction after multilevel surgery.
1.4.1
Quality of life studies after multilevel surgery
To date, only 7 publications have assessed quality of life or satisfaction of children and/or their parent after multilevel surgery. Cuomo et al., in 2007, were the first who studied quality of life progression after multilevel surgery . In multicenter study on a population of 57 ambulatory CP children who benefited from multilevel surgery on soft tissues, the authors used the Pediatric Quality of Life Inventory (PedsQL), which is a multidimensional (Physical, Emotional, Social, School Functioning) generic QoL scale , before and after surgery. They observed an improvement for the total QoL score of the parent version (+17.6%; P < 0.001) and for the physical dimension of the scale (+25.0%; P < 0.001). They observed the same thing, but in a statistically non-significant manner for the total score of the child’s version (+8.4%; P = 0.104) and the physical dimension (+8.6%; P = 0.189). Gorton et al. also used the PedsQL and reported similar results .
Himpens et al. evaluated the quality of life of children after multilevel surgery using the Cerebral Palsy Quality of Life Questionnaire for Children (CP QOL-Child) as well as their own self-designed questionnaire, in 40 children and their parents. They classified subjects according to their age, GMFCS level, as well as time elapsed since surgery. Their results showed a high quality of life score on the CP QOL-CHILD. For all the questionnaire’s domains, scores reported by children were significantly higher than those reported by their parents. Significant differences were found for the functional-related domains of the CP QOL-Child between GMFCS level III and levels IV–V, but not for the socio-emotional domains. Older children at the time of surgery (15–18 years of age) reported significantly less pain and feeling about disability than younger children operated between 10 and 14 years of age. All aspects evaluated in the author’s own questionnaire, i.e. ability to accomplish activities of daily living (ADL), physical activities and mood were improved after surgery.
The present study finds results similar to the ones reported by Himpens regarding the questionnaire designed by the author with perceived improvements in gait, pain, physical activity and fatigue.
1.4.2
Studies on satisfaction after multilevel surgery
Capjon and Bjørk conducted a study on 8 children with cerebral palsy and their parents, which included a semi-directed interview evaluating family situation, rehabilitation, and multidisciplinary cooperation after surgery. Children who reported little pain after surgery were satisfied with the procedure with an improvement in strength and gait capacities, leading to better social participation. Some children considered that there was very little physical improvement, those children had experienced severe pain after surgery. Most families found that there was a lack of information and communication regarding the different levels of rehabilitation available, and that the rehabilitation programs were difficult .
Borowsky et al. focused on parents’ satisfaction after this type of surgery. The study included 52 children with CP. During a follow-up consultation, the authors conducted a subjective evaluation on the satisfaction of parents post-surgery. Forty-three parents (82.6%) reported an improvement post-surgery and declared that they would take the same decision all over again. Five parents (9.6%) noticed no real improvement in their child’s life and 2 parents (3.8%) noted some deterioration .
Lee et al. also assessed parents’ satisfaction and parameters influencing their satisfaction. The study included 279 patients with CP. Their satisfaction was evaluated using a visual analog scale (VAS) from 0 to 10. Parents whose child was classified as GMFCS I were more satisfied than those whose children were GMFCS II and III. Satisfaction was higher when the procedure was unilateral than bilateral. After multiple regression analysis, several predictive factors of satisfaction were isolated: good GMFCS level pre-surgery, spastic hemiplegic CP type, being older at the time of surgery and longer follow-up . The same authors (Lee et al.) studied the evolution of the Pediatric Outcomes Data Collection Instrument (PODCI) scores after multilevel surgery and assessed the relationship between the improvement of the scale’s score and parents’ satisfaction level in 61 parents of ambulatory CP children. Factors significantly correlated to parental satisfaction after multilevel surgery were: older age at the time of surgery, good GMFCS level and importance of improvement in the sport and physical activity category of the PODCI .
Regarding satisfaction with surgical outcomes, this study found results similar to those reported in the literature with a good level of satisfaction. Lee et al., who also evaluated parents’ satisfaction and parameters influencing their satisfaction, found a mean satisfaction score of 7.9, close to our mean score of 8.3.
1.4.3
Correlation between the opinions of parents and their children
The present study is the only one with the one published by Himpens et al. that focused on measuring children’s quality of life as perceived by children themselves and their parent, as well as the correlation between the answers provided by children and their parent after this type of surgery. Himpens et al. showed significantly higher scores in children/adolescents in their study vs. parents in all the CP QOL domains. Other authors, such as Majnemer et al. using PedsQL in school-age children with CP, conducted a study outside of a surgical context and found a moderate to important correlation coefficient and thus reported that the vision of parents and children were comparable.
Contrarily to the Himpens’ study, our study found a moderate to important correlation between the perception of parents and children regarding the quality of life of the operated child, however similarly to other studies, parents had a tendency to underestimate the quality of life of their child. Our study found results close to those reported by Majnemer et al. but their study did not focus surgical outcomes.
Our study, with the one from Capjon and Bjørk, is the only one evaluating the satisfaction of children and not only their parents. Several studies have underlined the importance of not only focusing on the parents’ point of view. Most studies show that parents underestimate their child’s quality of life, regardless of their child’s pathology. Varni et al. reported that children with cerebral palsy were able in more than 50% of cases to evaluate their quality of life and that we should limit third-party evaluations to children enable to self-assess their quality of life or use these third-party evaluations to study the correlation between the perception of parents and their children .
Our study found a good parent–child correlation regarding the quality of life measures for children after multilevel surgery. For children who are able to self-assess their state, their opinion should be taken into account as soon as possible.
The parent–child correlation evaluation was done with the only parent who attended the half-day evaluation, mainly mothers. In fact, it was not possible for most children to be accompanied by both their parents due to the duration of the evaluation and distance between the family’s home and location of the study center (which was frequently a problem).
In spite of having tried to be as thorough as possible, we realize that the number of participants to the study was quite low. The results from the questionnaire designed by the author must be interpreted with caution, since it was not previously validated for reliability. The great variability in delays between surgery and the evaluation as well as the absence of preoperative data might have led to overestimating the quality of life as underlined by Gage et al. . Furthermore, a longitudinal study is required to show the impact of multilevel surgery on the quality of life of children with CP with a pre- and postoperative evaluation. This could also facilitate the evaluation of the parent–child correlation according to these two specific pre- and postoperative measures. The present study should be considered as a pilot study on ambulatory children with CP regarding the correlation between the perception of parents and perception of their children regarding quality of life and satisfaction after multilevel surgery. Further multicenter studies would be needed to validate these results. Selecting candidates for this type of therapeutic program is difficult because of the complexity of the surgery, high requirements of the subsequent rehabilitation stay, eventual neuro-psychological or behavioral disorders, and sometimes limited comprehension of the parents.
1.5
Conclusion
After multilevel surgery in ambulatory children and adolescents, a good correlation was found between the perception of parents and experience of children regarding surgical outcomes and quality of life assessed from the specific CP module of the DISABKIDS.
Most patients and their families were satisfied with the results. Children and parents reported improvements regarding standing up and gait, which represented the main objective of this type of surgery.
Even though a good correlation was found between the perception of parents and the experience of their children, it is important when possible to no focus only on the parents, since children are the first concerned by these issues, and in most cases are able to express their opinion.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
La paralysie cérébrale (PC) dont la prévalence est comprise entre 1,7 et 2,5/1000 naissances vivantes dans les pays européens et nord-américains , est à l’origine de fréquentes limitations d’activité motrice chez l’enfant, avec notamment un retentissement au niveau de la marche.
L’enfant présente initialement un appareil musculo-squelettique normal et une lésion cérébrale stable et définitive. Les conséquences de cette lésion cérébrale appelées « anomalies primaires » entraînent des manifestations diverses, à savoir une faiblesse musculaire, des troubles de la commande et de l’équilibre, ainsi que de la spasticité pour la majorité d’entre eux. Plus tard, des rétractions musculo-tendineuses et des vices architecturaux apparaissent. Les « anomalies secondaires » sont la conséquence directe de stimulations mécaniques anormales sur un appareil musculo-squelettique en croissance . Il en résulte un enfant tentant de marcher malgré ses anomalies structurales et dynamiques, certaines primaires et d’autres secondaires. La prévention et le traitement de ces anomalies reposent sur des techniques de kinésithérapie, des traitements médicamenteux et orthétiques, des injections de toxine botulique ainsi que des interventions chirurgicales.
Le traitement chirurgical, comportant des allongements et/ou des transferts tendineux, des ostéotomies de dérotation ou des stabilisations articulaires, et ayant toujours eu des objectifs fonctionnels, a longtemps été réalisé de façon limitée et successive par crainte de gestes chirurgicaux excessifs, aux conséquences irréparables .
De manière assez récente, le concept de chirurgie sur un seul niveau a été remplacé par celui de chirurgie multi-étagée, effectuée sur les deux membres inférieurs par deux équipes chirurgicales conjointes durant un seul temps opératoire, nécessitant une seule hospitalisation et un seul séjour de rééducation postopératoire.
L’efficacité de la chirurgie multi-étagée a été démontrée par de nombreuses études mettant en évidence une diminution du nombre et de la durée totale des hospitalisations au cours de l’enfance, une amélioration des paramètres de la marche, une augmentation des amplitudes articulaires, une diminution du coût énergétique de la marche, ainsi qu’une amélioration des capacités fonctionnelles évaluée à l’aide de l’évaluation motrice fonctionnelle globale (EMFG) .
Alors que les études s’intéressant à l’évaluation des résultats fonctionnels par méthode objective commencent à être nombreuses dans la littérature, il en existe très peu sur l’évaluation de la qualité de vie et la satisfaction après ce type de chirurgie. Il faut souligner que le point de vue des enfants est tout particulièrement peu étudié dans la littérature actuelle.
Cette étude avait pour objectif principal d’étudier la concordance parent–enfant concernant le niveau de qualité de vie des enfants et la satisfaction après chirurgie multi-étagée. L’objectif secondaire était de décrire la perception des enfants quant à l’évolution de leur état général et plus particulièrement dans le domaine de la marche.
2.2
Matériels et méthodes
2.2.1
Schéma général de l’étude
Étude observationnelle à visée descriptive monocentrique, réalisée dans un centre de médecine physique et de réadaptation pédiatrique de référence au niveau régional, auprès d’enfants paralysés cérébraux marchants ayant bénéficié d’une chirurgie multi-étagée à partir d’auto-questionnaire et d’entretien semi-dirigé. Cette étude a été approuvée par le comité d’éthique local et un consentement éclairé a été signé par chaque parent participant à l’étude.
2.2.2
Caractéristiques de la population étudiée
Pour participer à cette étude, les enfants devaient répondre aux critères d’inclusion suivants :
- •
être paralysé cérébral marchant (Gross Motor Function Classification Scale (GMFCS) I à III) ;
- •
avoir moins de 18 ans révolus au moment de la chirurgie ;
- •
avoir bénéficié d’une chirurgie multi-étagée dans l’établissement hospitalo-universitaire de référence régionale, Lorraine, France, entre 2009 et 2011. Pour être définie comme chirurgie multi-étagée, l’intervention chirurgicale devait comporter lors d’un seul temps opératoire au moins deux gestes chirurgicaux musculo-tendineux (allongement ou transfert musculaire) ou osseux, sur un ou deux membres inférieurs ;
- •
avoir bénéficié de la rééducation postopératoire au centre de médecine physique et de réadaptation pour enfants de référence régionale, Lorraine, France.
Les enfants qui présentaient une déficience intellectuelle légère (quotient intellectuel en dessous de 70), ou les enfants et/ou leur parent qui refusaient de participer à l’étude n’étaient pas inclus dans l’étude.
2.2.3
Données recueillies
Toutes les données ont été recueillies entre novembre 2012 et mai 2013, lors d’une demi-journée d’évaluation de la chirurgie multi-étagée, durant laquelle les enfants et le parent présent ont répondu, et ce de manière indépendante, à un auto-questionnaire de qualité de vie de l’enfant et à un entretien semi-dirigé par le médecin responsable de l’étude concernant la satisfaction vis-à-vis de la chirurgie et leur perception de l’évolution de la marche. De plus, des données liées à la chirurgie ont été recueillies à partir du dossier médical des patients.
2.2.3.1
Données démographiques et chirurgicales
À partir de l’entretien avec les familles et le dossier médical, les données suivantes étaient recueillies : sexe, âge, niveau scolaire au moment de l’étude, type de paralysie cérébrale, niveau selon la classification GMFCS avant et après la chirurgie, âge au moment de la chirurgie, nombre de procédures chirurgicales, niveaux opératoires, temps écoulé entre la chirurgie et l’étude, durée de rééducation postopératoire en centre.
2.2.3.2
Qualité de vie
Chaque enfant ou adolescent opéré ainsi qu’un de ses parents renseignaient le module spécifique à la PC du questionnaire DISABKIDS .
Le DISABKIDS est une échelle de qualité de vie conçue pour des enfants présentant des maladies chroniques, validée et traduite en six langues européennes, notamment française . Plusieurs versions du questionnaire sont disponibles, à savoir la version longue (37 items) évaluant les domaines mental (sous-domaines : indépendance et émotion), social (sous-domaines : inclusion et exclusion) et physique (sous-domaines : limitations et traitement) , la version courte (12 items) et évaluant les mêmes domaines, et la version conçue pour les enfants de moins de 7 ans utilisant des smileys (7 items). Enfin, 7 modules spécifiques à une pathologie chronique existent, dont un spécifique à la PC , constitués de 12 items répartis en deux dimensions, l’impact fonctionnel de la maladie et la communication. Chaque module dispose d’une version « enfant » et d’une version « parent ». Pour chaque dimension, un score était calculé variant de 0 à 100 (100 étant la meilleure qualité de vie possible).
2.2.3.3
La satisfaction vis-à-vis de la chirurgie et la perception de l’évolution de la marche
Afin de savoir si les patients et leurs parents étaient satisfaits de ce type de chirurgie et s’ils percevaient une amélioration subjective de leur état en général, un entretien semi-dirigé avec des questions en lien avec le domaine de la marche, principal objectif d’amélioration de ce type de chirurgie, a été réalisé par le médecin de médecine physique et de réadaptation responsable de l’étude, auprès des enfants et un de leur parent. Cet entretien comportaient 16 questions, comprenant 2 questions fermées avec comme modalité de réponse (Oui/Non) sur la satisfaction et le fait de redonner son accord a posteriori pour une telle chirurgie et 14 questions concernant la perception des changements de leur état général et le domaine de la marche à réponse fermée présentant toutes les mêmes modalités de réponse (D’accord/Pas d’accord/Ne sait pas). Les enfants et leur parent étaient invités à argumenter leur réponse. Les participants devaient également donner une note de satisfaction globale entre 0 et 10.
2.2.4
Analyse statistique
Une analyse descriptive de l’ensemble des données recueillies a été réalisée, telle que les variables quantitatives sont exprimées en moyenne (± écart-type) et les variables qualitatives par l’effectif ( n ) et leur proportion (%).
Les scores des 2 dimensions du module spécifique PC du DISABKIDS ont été calculés, pour les enfants ainsi que les parents. La concordance parent–enfant est estimée pour les variables continues, par le coefficient de corrélation intra classe (CCI). Pour les variables qualitatives, la concordance est estimée par le coefficient kappa ajusté sur le biais de prévalence (PABAK) compris entre –1 et +1, accompagné des indices PI (Prevalence Index) et BI (Biais index).
Un biais entre les juges (BI) existe lorsqu’une modalité de réponse est plus souvent rapportée par l’un que par l’autre. Un effet de prévalence (PI) existe lorsqu’une modalité de réponse est majoritairement rapportée, que ce soit par les enfants eux-mêmes ou par leur parent. Ce qui est le cas, pour cette étude, d’où l’utilisation du PABAK .
L’interprétation des indices CCI et PABAK est basée sur la catégorisation faite par Landis et Koch, à savoir :
- •
0,21 à 0,40 concordance faible ;
- •
0,41 à 0,60 concordance modérée ;
- •
0,61 à 0,80 concordance bonne ;
- •
0,81 à 1,00 concordance excellente .
L’analyse statistique a été réalisée à l’aide du logiciel SAS 9.3 [SAS Inst., Cary, NC]. Les différences étaient considérées significatives avec p < 0,05.
2.3
Résultats
2.3.1
Caractéristiques démographiques
Dix-neuf patients étaient éligibles à l’étude. Trois enfants étaient perdus de vue (deux pour cause de déménagement dans une autre région, une patiente est restée injoignable). Après avoir reçu une information éclairée de l’étude, quatre parents ont refusé que leur enfant y participe. Les principaux motifs de refus étaient la participation antérieure à d’autres études, une prise en charge médicale considérée comme consommatrice en temps, d’où un refus pour un nouveau rendez-vous. Au final, 12 familles ont participé à la présente étude.
Les principales caractéristiques démographiques et chirurgicales des 12 enfants ayant participé à l’étude, sont présentées dans le Tableau 1 .







