The Malerich Procedure: Distal Scaphoid Resection
Louis W. Catalano III
O. Alton Barron
Indications
Chronic scaphoid nonunion with arthritis limited to the radial styloid-scaphoid joint
Contraindications
Arthritis at the proximal radial styloid-scaphoid joint
Capitolunate arthritis
Radiolunate arthritis
Proximal scaphocapitate arthritis
Scapholunate ligament rupture/dissociation
Preoperative Preparation
Patients most often complain of gradually worsening dorsoradial wrist pain and stiffness that is exacerbated by activity. A prior traumatic wrist injury may or may not be recalled.
Physical examination will reveal mild to moderate dorsoradial wrist swelling. Focal tenderness is usually present at the radioscaphoid joint. It is important to evaluate for tenderness at the scaphocapitate, lunocapitate, and radiolunate joints. Tenderness at these articulations may indicate more diffuse arthritic changes that precludes use of this technique.
Wrist range of motion is usually decreased, especially wrist extension and radial deviation. The Watson test may reveal painful crepitus, as the wrist is brought into radial deviation. Because weakness is usually present, grip strength should be objectively measured and compared to the other side.
Preoperative radiographs should be closely inspected for evidence of periscaphoid degenerative changes (Fig. 18-1). Any periscaphoid arthrosis, aside from changes at the radial styloid-scaphoid joint, is a contraindication to the procedure.
A preoperative computed tomography (CT) scan or magnetic resonance imaging (MRI) will clearly determine the extent of the carpal degeneration. In particular, the capitolunate joint must be clearly imaged to ensure that no arthritis is present prior to performing this procedure (Fig. 18-2).
The preoperative discussion with the patient should highlight several key points. First, the procedure requires only 2 weeks of postoperative immobilization and requires no bone grafting or bone healing. No internal fixation is used. In the unlikely scenario that the procedure fails, the procedure does not interfere with the more traditional wrist salvage procedures (i.e., scaphoid excision and four-corner fusion, proximal row carpectomy, total wrist fusion).
Wrist arthroscopy can be performed prior to the procedure to verify that isolated radial styloid-scaphoid arthritis exists and that the scapholunate ligament is intact. Synovectomy can be performed as well.
Technique
Starting at Lister’s tubercle extending distally along the thumb ray, use a 5- to 7-cm oblique incision (Fig. 18-3).
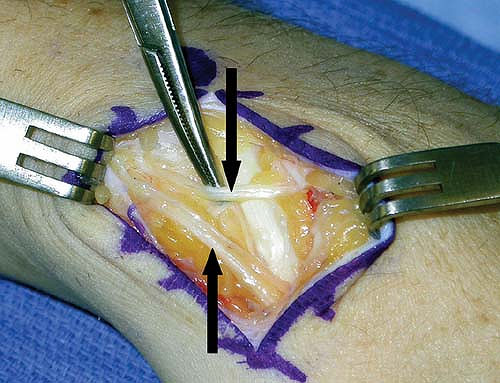
Identify and protect branches of the superficial radial and lateral antebrachial cutaneous nerves (Fig. 18-4).
Identify the radial artery near the scaphotrapezial joint, and protect it throughout the case (Fig. 18-5).
Release the extensor pollicis longus (EPL) compartment, and protect the EPL tendon is. Identify the extensor carpi radiate longus, and retract it ulnarly (Fig. 18-6).
Make a longitudinally capsular incision, starting at the distal radius and extending distally along the incision.
Sharply elevate the capsular flaps radially and ulnarly. The osseous architecture can be confusing due to distal scaphoid pole overgrowth and the appearance of an “extra joint” due to the nonunion site. Therefore, use intraoperative fluoroscopy to identify the nonunion site and to verify excision of the distal pole.

Figure 18-5 The arrow points to the radial artery as it travels through the anatomic snuffbox. This artery is dissected and protected throughout the surgery.

Get Clinical Tree app for offline access