Chapter 3 The Malalignment Syndrome
Clinical findings commonly noted with malalignment
‘Malalignment syndrome’ seen with ‘rotational malalignment
The ‘malalignment syndrome’ associated with a sacroiliac joint ‘upslip’
Comments regarding the ‘malalignment syndrome’ and ‘outflare/inflare’ presentation
Combinations of asymmetries: a summary
Clinical findings commonly noted with malalignment
Malalignment syndrome will be discussed here in terms of findings on the physical examination that are commonly associated with the syndrome (Box 3.1).
Box 3.1 Physical findings associated with the ‘malalignment syndrome’
1. Asymmetry of pelvic orientation with any movement around the coronal, vertical and sagittal axes and in the three planes
2. Asymmetry of sacroiliac joint mobility
3. Pelvic obliquity and compensatory curvature, or ‘scoliosis’, of the lumbar, thoracic and cervical spine
4. Asymmetry of the thoracic and shoulder girdle ranges of motion
5. Asymmetry of lower extremity orientation
6. Asymmetry of foot alignment, weight-bearing and shoe wear
7. Asymmetry of muscle tension, strength and bulk
8. Asymmetry of ligament tension
9. Asymmetry of upper and lower extremity ranges of motion
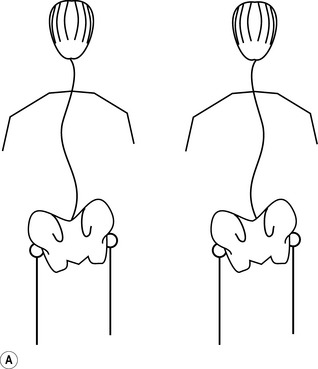
10. Apparent (functional) leg length difference
The prevalence of malalignment, and of the three most common presentations, has been detailed in Chapter 2. Basically:
1. some 80-90% of adults present out of alignment
2. ‘rotational malalignment’ is by far the most frequently seen, in approximately 80%, either on its own or in combination with one/both of the other presentations
3. an ‘upslip’ presents on its own in about 10% and in combination with ‘rotational malalignment’ and/or an ‘outflare/inflare’ in another 5-10% of cases
4. ‘outflare’ and/or ‘inflare’ is present in approximately 45-50%, either in isolation or combined with one or both of the other types
The ‘malalignment syndrome’ itself is seen only in association with:
The discussion will focus first on the ‘malalignment syndrome’ specifically as seen in association with ‘rotational malalignment’, with reference to SI joint ‘upslip’ where appropriate. A separate section emphasizes the major similarities and differences in the presentation of the syndrome seen in association with an SI joint ‘upslip’, as compared with ‘rotational malalignment’. There follows a discussion of the features of an ‘outflare/inflare’ presentation and how it differs from an ‘upslip’ and ‘rotational malalignment’. Significant clinical correlations are indicated at the end of most of the subheadings. Reference is also made to Chapters 5 and 6 and Appendices 1–13 for a more detailed analysis of the sports-specific implications of this syndrome.
‘Malalignment syndrome’ seen with ‘rotational malalignment
1. torsion of the sacrum around the right or left oblique axis, which adds to the distortion of the pelvic ring (Figs 2.42, 2.50)
2. evidence of dysfunction of movement of the symphysis pubis or of one or both SI joints, which can range from hypermobility to various degrees of decreased mobility or even complete ‘locking’ (see Ch. 2).
Description of ‘rotational malalignment’
In order to prevent needless repetition, the following abbreviations will be used:
1. ‘right (or left) anterior (or posterior)’ rotation
– referring to ‘anterior’ or ‘posterior’ rotation of the right or left innominate relative to the sacrum in the sagittal plane (Figs 2.10, 2.21, 2.42, 2.76)
2. ‘right (or left) locked’ on the kinetic rotational (Gillet) test
‘Right anterior, left locked’, for example, would refer to a person presenting with ‘anterior rotation’ of the right innominate and ‘locking’ of the left SI joint; there will very likely also be a compensatory ‘posterior’ rotation of the left innominate. For illustrative purposes, reference is frequently made to ‘right anterior and locked’, which refers to the combination of ‘right anterior rotation and locking of the right SI joint’ because this is the most frequently seen of all these patterns of ‘rotational malalignment’ (see Appendix 1).
Clinical correlation
Localized pain may arise from one or both SI joints. Those with hypomobility or ‘locking’ of one SI joint not infrequently complain of pain from the region of the other, supposedly ‘normal’, SI joint. One explanation is that the pain is attributable to the increased stress placed on this ‘normal’ joint, its capsule and ligaments as it tries to compensate for the lack of mobility in the impaired SI joint (Figs 2.4, 2.5, 2.19).
The pain may also result from:
1. a passive increase in muscle or ligament tension; for example, the constant increase in tension in the right sacrotuberous and sacrospinous ligaments as long as a ‘right posterior, left anterior’ innominate rotation and torsion of the sacrum around the left oblique axis are present (Fig. 2.21)
2. a chronic increase in tension or even spasm in muscles that reflects:
Pain may also result from an increased or abnormal pressure on the malaligned, and hence incongruent, SI joint surfaces. Given the propeller-shape of this L-shaped joint, with the convex surface of one part of the ilium or sacrum fitting its concave counterpart, it is not hard to imagine how little displacement of one surface relative to the other is actually needed to result in stress on the joint (Fig. 2.3). Development of the convex iliac ridge and matching sacral concavity by the 3RD decade (Fig. 2.7B), also subsequently of other seemingly matching depressions and elevations or just degenerate changes will only further increase the stress that results with even minimal displacement of these joint surfaces whenever pelvic malalignment recurs. Bone scans may actually show increased and/or asymmetrical activity in the SI joints (Fig. 4.39). In the absence of any indications of an inflammatory condition, such as a seronegative spondyloarthropathy or ankylosing spondylitis, these abnormalities on the bone scan may simply reflect an increase in bone turnover triggered by an increase in pressure on the joint surfaces. Unless there is an actual inflammatory element, the abnormalities on the bone scans usually disappear with time as the pressure on the surfaces is finally relieved by keeping the joint in alignment.
1. a previous severe sprain or strain of the ligaments, such as can occur with a shear injury to the SI joint sustained by falling and landing on one buttock or leg (Fig. 2.51B)
2. ligament lengthening that has occurred with time as the ligaments are:
3. generalized joint hypermobility, related to:
A quick test to assess the degree of mobility is to have the person flex the wrist and then passively bring the thumb toward the volar aspect of the forearm (Fig. 3.1). In most tests, the thumb will end up parallel to the forearm. If the thumb is further away from the forearm (e.g. the person on the left in Fig. 3.1A), or if it ends up close to or even touching the forearm, the person may well have generalized joint hypo- or hypermobility, respectively. This should be confirmed by doing a more complete assessment of the amount of joint play possible on passive movement of other joints; for example, the 9-point Beighton scale may be appropriate (Beighton et al. 1999; Fig. 3.1B). A side-to-side comparison is also important to make sure one is not just dealing with laxity attributable to previous injury of specific ligaments on that side.
Variants of the syndrome seen with ‘rotational malalignment’
Malalignment of the pelvis, spine and extremities can result from a number of interacting causes. Postural distortion, for example, may result in a muscle imbalance but the distortion may itself be the result of such an imbalance. As Maffetone indicated in 1999, potentially more than one postural distortion can result from the same muscle imbalance. He gave the example of psoas major, indicating that inhibition of tension tone in this muscle on one side, for whatever reason, typically causes the pelvis to tilt. The pelvis usually rises on the opposite side, where psoas major is now in relative ‘overfacilitation’, the tension tone in the muscle being increased compared with that on the inhibited side (Fig. 3.2A). The effect would be to rotate the innominate anteriorly on the ‘facilitated’ side, raising the iliac crest. Maffetone, however, went on to say that:
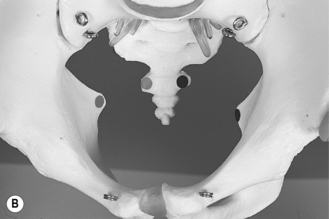
1. the ‘left anterior and locked” pattern (Fig. 3.3A)
2. the ‘more common’ rotational patterns (Fig. 3.3B)



Fig. 3.3 Two variants of the ‘rotational malalignment’ presentation (see also Figs 3.22, 3.23). (A) With the rare ‘left anterior and locked’ pattern – the left foot turned outward from the midline and pronating, the right in toward midline and supinating: (i) standing and (ii) walking view. (B) With one of the ‘more common’ patterns: the right foot is turned outward and pronating; the left inward (may even cross the midline) and supinating (see Fig. 3.19Bii).
These differences will be highlighted in the discussion of the specific asymmetries.
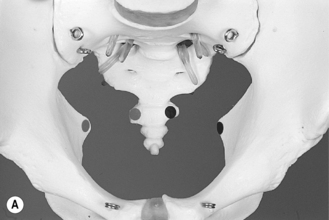
Asymmetry of pelvic orientation in the coronal (frontal) plane
As indicated in Chapter 2, ‘rotational malalignment’ results in a complete asymmetry of the major pelvic landmarks (Figs 2.42, 2.73A,B, 2.76), both side-to-side and front-to-back, because of an asymmetry of the sacrum and the innominates with:
1. rotation around all 3 axes (Fig. 2.9)
2. a possible simultaneous element of translation of the innominate(s) relative to the sacrum (at the SI joints) and/or to each other (at the symphysis pubis) in the three planes:
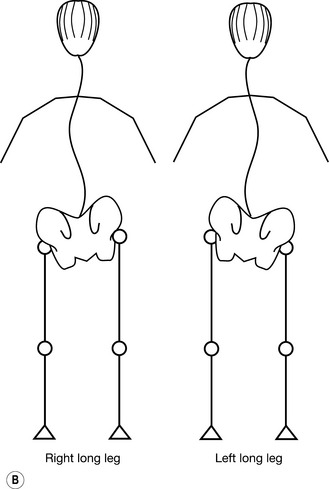
1. the position in which the person is examined: with a ‘right anterior’ rotation, for example, the right iliac crest may be higher or lower in standing but will usually be higher in sitting and definitely in prone-lying; the most common pattern is shown in Figures 2.73C and 2.76B
2. a coexisting anatomical (true) leg length difference (Figs 2.72B, 2.74A), ‘upslip’ or ‘downslip’ (Fig. 2.73A,B)
3. the direction of a sacral torsion, if present (Figs 2.10, 2.14, 2.42, 2.88)
4. the side of SI joint ‘locking’, if present (Figs 2.119–2.121)
Clinical correlation: coronal (frontal) plane asymmetry
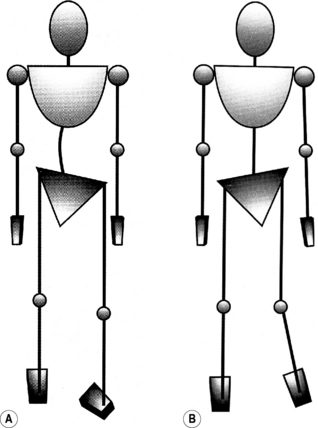
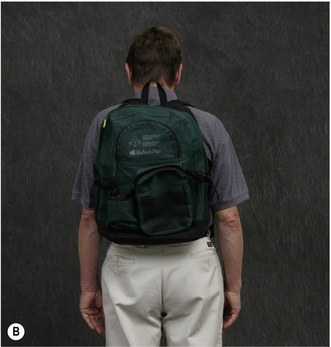
The difference in the elevation of the iliac crests is sometimes strikingly obvious and may be accentuated by the cut of a costume. The visual effect of this may distract from the aesthetic appearance. In disciplines such as dancing and figure-skating, this could conceivably affect the perception and judgement of style. In anyone, there may be mundane problems related to clothing, straps or belts repeatedly slipping down or even completely off on one side, just as objects carried over the ‘lower’ shoulder will tend to slip off (Figs 2.70, 2.76B, 2.90, 2.95A, 3.4).
Sitting is likely to present problems. The ischial tuberosities are at different levels: raised on the side of the ‘anterior’, lowered on the side of the ‘posterior’ rotation (Figs 2.76D, 6.4). With a ‘right anterior’ rotation, the right ischial tuberosity can easily end up 1 cm off the seating surface, the weight now borne primarily by the left tuberosity. The person often talks of ‘sitting more on one buttock than the other’ or ‘off to one side’ and may get relief simply by putting a hand, small pillow or a magazine under the raised tuberosity to fill the gap when riding (see Ch. 6), driving, flying, or travelling by other means, or in any other situation where they are sitting for a longer period of time.
Sitting increases the pressure on the lower tuberosity and creates a shearing force on the ipsilateral SI joint by pushing the innominate upward relative to the sacrum. In addition, the ischial tuberosities serve as the insertion of the sacrotuberous ligament and the origin of the hamstrings (Figs 2.5, 2.6, 2.21). These structures are more vulnerable to direct pressure at this site on the side of the ‘posterior’ rotation, especially when sitting in a slouched position or on a hard surface. Slouching or sitting in a bucket seat allows the pelvic ring – the innominates and sacrum – to tilt posteriorly as a unit, further increasing pressure, especially on the ischial tuberosity and the PSIS on the side of the posteriorly rotated innominate. Aside from using a hand, cushion or magazine between the raised ischial tuberosity and the seat to actually fill in the gap created by the ‘anterior’ rotation, the person may have found that he or she gets comfort by:
1. increasing the general amount of cushioning under both buttocks, allowing the lower one to sink in further than the higher one – memory foam is ideal for this (Fig. 7.42)
2. placing a cushion under the thighs, ahead of the ischial tuberosities; better still, a pillow that is tapered down from buttocks to thighs (which also shifts weight-bearing forward, more under the thighs)
3. continuously shifting weight-bearing from side-to-side to off-load the tender ischial tuberosity
None of these methods may work very well, especially when the person has to remain seated for a longer period of time in a confined space or when the seating area is small and hard, such as a church pew, a rowing shell or a bicycle seat. In riding, a lowered left ischial tuberosity may increase pressure on the horse’s left paravertebral musculature, by digging into the muscles directly (bareback) or through the saddle (Fig. 6.4A). The increased pressure can cause a reflex increase in tension in these muscles so that the horse starts to appear ‘stiff’ on that side, hesitating or eventually even refusing to veer to the right on command (see Ch. 6).
Asymmetry of pelvic orientation and movement around the vertical axis in the transverse plane
With ‘rotational malalignment’, the pelvic unit often appears rotated counterclockwise, around the vertical axis in the transverse plane some 5–10 degrees, rarely more. This probably relates to the fact that ‘right anterior, left posterior’ rotation, which tends to twist the pelvic ring in a counterclockwise direction and brings the right ASIS forward and the left backward, is by far the most frequently noted pattern. Therefore, the pelvis is more likely to jut out a bit at the front on the right side and recede on the left when the person is standing (Fig. 3.5A). Rotation in this plane will, however, also be influenced by the position of examination. Consider the example of the person who has such seemingly obvious right forward rotation in standing. When he or she goes to lie prone on a hard plinth, the protruding right ASIS will be the first to contact the plinth and will be forced posteriorly. In this position, therefore, the pelvis could now look level, or the right PSIS may even end up protruding backward compared to the left, as if the pelvis had rotated clockwise in the transverse plane.
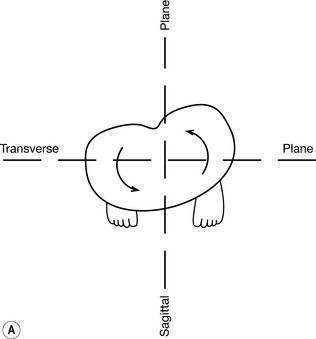
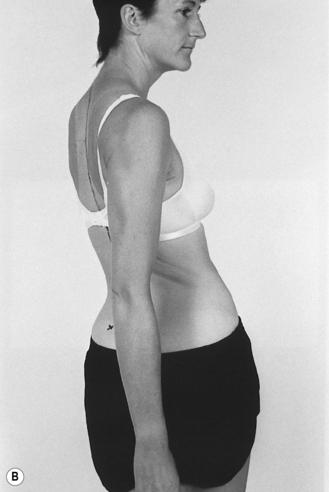
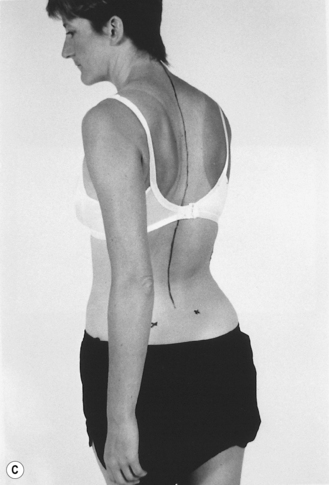
Fig. 3.5 Asymmetry of pelvic rotation around the vertical axis in the transverse plane typically seen with ‘rotational malalignment’. (A) Passive: standing – asymmetry, usually with some counterclockwise rotation of the pelvis (left side positioned relatively backward, right forward on a superior view); the trunk may rotate in the opposite or the same direction, with compensatory rotation of the head and neck to keep them in midline (not shown). (B) Active clockwise rotation to 40 degrees. (C) Active counterclockwise rotation decreased to 30 degrees (note the decreased facial, shoulder girdle and chest profile compared with Fig. 3.5B).
Restriction into the side of the ‘posterior’ rotation can occur for the following reasons:
First, counterclockwise rotation of the pelvis in the transverse plane seen normally during the walking cycle – right ASIS forward with right ‘swing’ leg – occurs with the simultaneous contrary rotation of the innominates: right posterior and left anterior (Figs 2.12, 2.21, 2.22, 2.41). The pattern is reversed with clockwise rotation on swinging the left leg forward.
Second, when there is ‘rotational malalignment’ with the right innominate seemingly held in ‘anterior’, and the left in ‘posterior’ rotation, clockwise rotation is increased in part due to the fact that the malaligned innominates can rotate further from their resting position in the directions needed to allow this particular movement (Fig. 3.5B). The left one, which starts off rotated posteriorly, can rotate anteriorly through more degrees until it reaches the end of available range in the sagittal plane than if it had started from its normal position. Similarly, the anteriorly rotated right innominate can rotate posteriorly through more degrees until it reaches the end point in that direction. Also, on account of the wedging of the sacrum, the left innominate already flares slightly inward, the right outward. Overall, this translates into more degrees of clockwise rotation.
Conversely, counterclockwise rotation is limited by the fact that the innominates are already rotated part way into the directions required for them to move into for this manoeuvre (Fig. 3.5C). Namely, the right is already rotated anteriorly and the left posteriorly, restricting further movement into these directions required for counterclockwise rotation.
A rotation of 40 degrees to the right and only 30 degrees to the left would, for example, not be unusual in someone with ‘rotational malalignment’ with ‘right anterior/left posterior’ innominate rotation (Fig. 3.5B,C). Discrepancies of greater magnitude can occur, the degree of limitation appearing to be proportionate to the degree of difference in ‘anterior’ versus ‘posterior’ innominate rotation. However, correction of the malalignment immediately removes this restriction and may now allow for an equal amount of rotation: 40 degrees to right and left, in the example given. The fact that rotation might actually now be 45–50 degrees or even more bilaterally suggests that other restrictive factors were operative prior to realignment, such as restriction caused by sacral torsion and/or rotation, asymmetry of muscle tension, and asymmetry of the hip ranges of motion (see below).
Clinical correlation: transverse plane asymmetry
This asymmetry interferes with the ability to execute turning manoeuvres that require pelvic rotation in the transverse plane when both feet are on the ground. The prime example is downhill skiing, in which turns are initiated in large part by movement of the pelvis in this plane, combined with shifting weight onto the appropriate edges. The skier is more likely to experience limitation on attempting a turn into the side of a posterior innominate rotation (see Ch. 5).
1. the thorax is pinned to the floor, such as in wrestling (Fig. 5.36)
2. a gymnast restricts thoracic rotation by holding on to the apparatus with both hands while spinning or twisting the pelvis and legs (Fig. 5.11B,D).
Conversely, a restriction of rotation of the pelvic unit in one direction at the pelvic level may require a compensatory increase in the amount of rotation of the thoracic spine. Such an increased demand on the thoracic segment is more likely with activities that normally require a simultaneous rotation of both the pelvis and trunk while standing upright: with certain field events (discus, hammer, shot and javelin), on playing golf, baseball, and court sports, or simply reaching to the right or left (Fig. 2.44). The increased stress placed especially on the thoracolumbar (T/L) junction may account for the onset or aggravation of mid back pain, especially if these actions are a part of the person’s work or sports activities. This issue is discussed further under ‘Curvatures of the lumbar, thoracic and cervical segments’ (see below).
Asymmetry of sacroiliac joint mobility
Those presenting with ‘right’ or ‘left anterior’ rotation show SI joint mobility dysfunction, which may take any of the forms shown in Box 3.2.
Box 3.2 Sacroiliac joint movement dysfunction
1. ‘Locking’: jamming of the innominate and sacrum against each other on one side, (e.g. excessive ‘anterior’ rotation of an innominate) can result in a loss of movement between the two, so that they now move together instead; on the affected side, this results in:
2. Partial ‘locking’, which results in:
3. ‘hypermobility’ or ‘laxity’:
1. the previously noted hypomobility or actual ‘locking’ may still be detectable on the same side; also, sometimes these problems may actually have ‘switched’ sides
2. more likely than not, movement on lumbosacral flexion, extension and kinetic rotational tests will now be found to be normal (i.e., ‘locking’ resolved)
3. the side previously felt to be hypomobile may now turn out to be hypermobile, suggesting a possible underlying problem of ligament laxity, joint osteoarthritis, muscle weakness, impaired control or a combination of these that was previously hidden by the ‘locking’.
Curvature of the lumbar, thoracic and cervical segments
What follows is an abbreviated discussion of how the resting curves of the spine are influenced by:
1. side-flexion of the spine and/or rotation of the pelvis and spine
2. malalignment of the pelvis and excessive rotation of individual vertebra(e) or a vertebral segment.
In 1903, Lovett pointed out that:
1. the spine is a flexible rod that is already bent in one plane (sagittal) to create the lumbar lordosis and thoracic kyphosis
2. the rod, therefore, cannot be bent in another plane (e.g. coronal or ‘frontal’) without twisting at the same time.
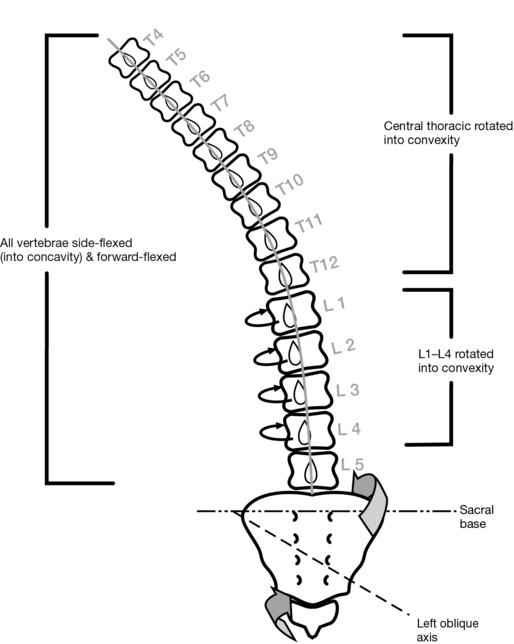
First, the components of the lumbar spine are twisted. For example, on side-bending the trunk to the left, the bodies of vertebrae L1–L4 inclusive rotate to the right, into the convexity formed. Their spinous processes, therefore, rotate to the left, toward the concavity formed (Figs 2.42, 2.96, 3.6, 4.6, 4.24). This rotation is accompanied by simultaneous side-flexion of the vertebrae into the concave side, as well as either extension or forward flexion; that is, as discussed in Ch. 2, there is movement in all three planes (Figs 2.42, 2.52B, 2.94, 2.96).
The combination of Forward flexion, Side-flexion and Rotation constitutes the so-called ‘FSR movement’; should extension occur, the result would be an ‘ESR movement’. These patterns are delineated by the so-called ‘laws’ of Fryette (1954). A vertebra may become excessively rotated to the right or left and/or into extension or flexion, and become ‘stuck’ in that position. Movement in one facet joint will then be pathologically restricted, causing the vertebra to rotate around that facet on flexion or extension (Figs 2.52B, 2.94A).
Second, it is harder to predict the direction of vertebral rotation in the thoracic segment, which is affected by the attaching ribs, the overlying scapulae and soft tissue attachments. The clear-cut correlation that exists in the lumbar segment is missing. The central thoracic vertebrae are more likely to rotate into the convexity (Fig. 3.6); the upper ones are less likely to do so (Lee 1992b).
Third, during normal gait, there is a continuous change in the convex/concave curve patterns seen in the thoracic and lumbar spine, changing in direction on right and left swing-through to weight-bearing back into swing-through phase of the cycle while the pelvis and thorax rotate in opposite directions in the transverse plane, balanced by contrary movement of the arms (Fig. 2.41). During normal gait, therefore, there is a matched rotation of the pelvis and spine which helps to balance body weight while the head remains centred throughout.
Effect of malalignment on the spine
1. The spine cannot accommodate without simultaneous rotation of the vertebrae in the thoracic and lumbar segments.
2. The curve formed in the thoracic segment is usually opposite in direction to that formed by the lumbar vertebrae, resulting in the typical double curve, or ‘scoliosis’ (Figs 3.7A, 3.8, 2.70, 2.90, 2.91, 2.95, 2.120C).
3. The lumbar and central thoracic vertebral bodies appear to rotate into the respective convexity of these curves (Fig. 3.6).
4. X-Rays will show this typical double, ‘scoliotic’ curve, with a reversal at the thoracolumbar junction (Figs 4.6, 4.31) and possibly also noticeable aggravation of any ‘intrinsic’ curves on comparison to X-rays taken when the person is in alignment.
There is, therefore, a further reversal in the curvature of the spine in order that the head will, hopefully, end up straight and in midline. This reversal usually occurs at the level of the cervicothoracic junction (Fig. 2.91A). It may, however, start as far down as T4 or T5, which accounts for a large number of those people with a very obvious curvature of the lower and mid-thoracic segment convex, for example, to the right yet with the shoulder and scapula dipped down on the right side instead of the left, as might be expected (Fig. 2.91B). Reversal occurring in the upper thoracic region creates another stress point and may account for reports of interscapular and upper back discomfort. Also, there is likely to be a constant increase in tension or outright contraction in muscles attempting to straighten the cervical spine and avoid any rotation of the head and neck.
The direction of the curves associated with ‘rotational malalignment’ (or an ‘upslip’) may differ depending on whether the person is examined standing, sitting or lying prone. The curves are probably best regarded as an adaptation of the spine to the interaction of several factors, including the direction of sacral torsion, the pelvic obliquity, the lateralization of ‘anterior’ and/or ‘posterior’ innominate rotation and SI joint ‘locking’, and the presence of any lengthening having occurred with prolonged stretching, or increased tension or actual contracture of soft tissue attaching to the pelvis, ribs and spine. More important than defining the direction of these curves is to determine if there are any factors that may have resulted in formation of the curves, including malalignment of the pelvis or rotation of individual vertebrae, that can be treated using manual therapy (see Ch. 7).
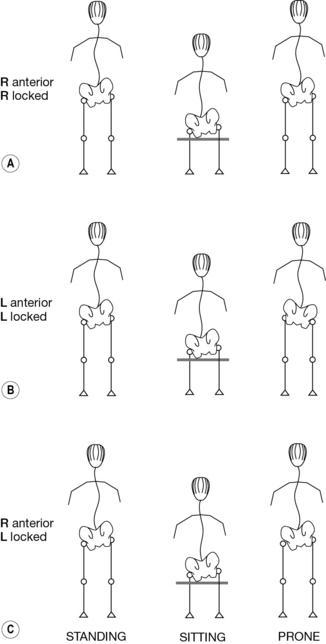
When one looks at the combination of pelvic obliquity and the pattern of the thoracic and lumbar curves, the pattern is least likely to change from standing to sitting to lying prone if the anterior innominate rotation and ‘locking’ are both on the right side (Fig. 3.8A). With the ‘left anterior and locked’ pattern, the obliquity will change from the right side usually being higher in standing and sitting, to the left being higher when lying prone; whereas the curves may remain the same or change on going from one position to another (Fig. 3.8B). When the ‘anterior’ rotation is on one side and the ‘locking’ on the other, the curves are likely to change on lying prone; whereas the pelvic obliquity may stay the same, but this is not predictable (Fig. 3.8C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree