Chapter 8 Treatment
Manual therapy modes
Introduction
Manual therapy can be practised by numerous specialists such as physiatrists, osteopaths, physiotherapists, chiropractors, massage therapists, naturopathic doctors and athletic trainers. The techniques described in this chapter can be applied by some or all of these practitioners depending on their education and training (see Ch. 7 regarding the Canadian programme for post-graduate training of physiotherapists in the theory and practice of manual therapy, leading to designation as a ‘Fellow of the Canadian Association of Manual Therapists’ or ‘FCAMT’). Patients should not hesitate to ask their local practitioners what post-graduate training they have had in manual therapy!
Tissue types
Connective tissue
Fascia
Fascia is made up of collagen, elastin and a polysaccharide gel complex forming a three-dimensional cobweb covering the body’s tissues (Fig. 8.1). It has three continuous layers: (1) a superficial layer under the skin, (2) a deeper, ‘ensheathing’ layer which covers muscles, bone, nerves, blood vessels, and organs right down to the cellular level, and (3) the deepest layer, which connects with the dura of the central nervous system. The muscle is intimately connected with fascia, hence the term ‘myofascia’. Fascia functions to support our body, absorb shock, enhance cellular respiration and metabolism, and assist with fluid and lymphatic flow.
Malfunction of the fascial system can occur from poor or prolonged postures causing asymmetrical loading, trauma, and repetitive strain. Changes in fascial mobility occur when the fascia is bound down or restricted in areas. Due to its continuous nature it causes a global effect by pulling on the body at points distal to the primary site of dysfunction (see Chs 2, 3). This stimulates nociceptors, causing pain, and reduces the body’s ability to absorb and distribute forces that may be incurred with sudden trauma or repetitive loading. It can also alter an individual’s biomechanics and influence his or her posture and dynamic balance. Injuries to the fascial system do not result in typical nerve root or trigger point referral patterns and standard imaging tests (i.e. X-rays, CT scans, MRI, etc.) will not pick up fascial dysfunction, so typically these malfunctions usually go undiagnosed.
Contractile tissue
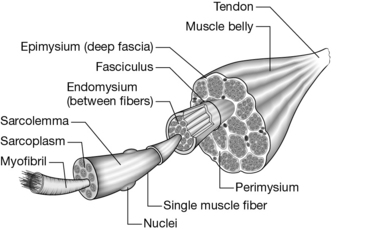
Muscles are comprised of bundles of fasciculi that, in turn, are made up of bundles of muscle fibres (Fig. 8.2; the latter) themselves are formed from bundles of myofilaments (myofibrils) composed of two main proteins, actin and myosin: the contractile elements of the muscle. Each layer of a bundle is separated by fascial tissue that helps transmit forces from muscle to tendon and bone.
1. the muscle spindle, which provides feedback regarding the length of the extrafusal fibres, and
2. the Golgi tendon organ, which is located in the tendomuscular junction and gives information about muscle tension.
When joint receptors are damaged by injury, the damage will alter the body’s position sense – or proprioception – and also affects muscle tone. When the antagonist muscles are unable to relax or are pathologically shortened, the normal range of motion is restricted which will again influence muscle tone. Certain muscles are over-active and tend to shorten, while others are underactive and tend to lengthening or atrophy. These are factors that contribute to the ‘malalignment syndrome’, where the pattern of muscular ‘facilitation’/’inhibition’ and strength is noted to be asymmetrical with an ‘upslip’ and ‘rotational malalignment’ (see Boxes 8.1, 8.2 for an example of muscles which become shortened or lengthened).
Neural tissue
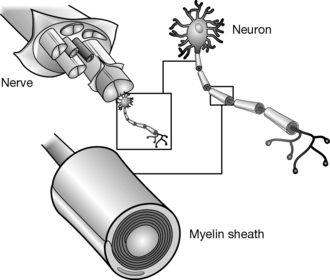
The nervous system is a continuous network of specialized cells that communicates information from the body to the brain and vice versa (Fig. 8.3). These messages or electrical signals, including perception and movement, are responsible for interaction with the environment. The nervous system is composed of neurons and glial cells which together generate electrical impulses that travel between our central nervous system (CNS) and peripheral nervous system (PNS). Generally, our CNS processes information in our spinal cord and brain and then sends signals back to our PNS where sensory, motor, and autonomic nerves leave the spinal cord to innervate our muscles, articular structures, organs, and glands. The neurons communicate with each other via electrochemical signals or neurotransmitters to transmit impulses from one neuron to the next.
1. lack of oxygen secondary to compression will cause increased intraneural pressure that can take several weeks to reverse
2. separation of nerve fibres occurs with sustained pressure
Articular structures
Joint receptors
Type 3 receptors are found in ligaments near bony attachments but not in the longitudinal ligaments of the spine (Fig. 3.68). These receptors are stimulated by extremes of dynamic movement when the ligaments are stressed. They are dynamic receptors that are inactive at rest, have a high threshold and are slow to adapt. Clinically, these receptors can be stimulated by providing a strong, prolonged distraction on a joint to help reduce tone in the surrounding muscles.
Visceral tissue
Visceral tissue is specialized tissue unique to each organ/viscera in the body, all of which are encapsulated in a fascial covering. With the support of fascia and specialized ligaments, viscera and organs are suspended in the body, decreasing gravitational strain on these important structures (Fig. 4.43). Posture, alignment of the bones and muscle balance all play a role in ensuring the proper force through the fascia required to maintain the position of the organs and viscera. When the ‘malalignment syndrome’ is present, fascial pull through the body can affect organ position and cause stress to affect its function. A detailed explanation of viscera and organ tissue is beyond the scope of this book. It is suggested the reader refer to more specialized anatomy and physiology texts.