19 The leg, ankle, and foot
In the orthopaedic out-patient clinic disorders of the foot are second in frequency only to disorders of the back. Their prevalence may have several causes. Hereditary factors: The foot is probably in a state of relatively rapid evolution consequent upon man’s assumption of the upright posture, and perhaps for that reason it is prone to variations in structure and form which may impair its efficiency. Postural stresses: Overweight throws an increased burden on the feet, and they may be unable to withstand the stress without ill-effect, especially if the intrinsic muscles are poorly developed. Footwear: The wearing of shoes is a potent cause of foot disorders. Many types of shoe interfere seriously with the mechanics of the foot, and the ladies’ shoe with high heel and pointed toe is particularly to blame.
SPECIAL POINTS IN THE INVESTIGATION OF LEG, ANKLE, AND FOOT COMPLAINTS
Steps in clinical examination
A suggested plan for the routine clinical examination of the leg, ankle, and foot is summarised in Table 19.1.
Table 19.1 Routine clinical examination in suspected disorders of the leg, ankle, and foot
| 1. LOCAL EXAMINATION OF THE LEG, ANKLE, AND FOOT | |
| Inspection | At the toes: |
| Bone contours and alignment | Flexion |
| Soft-tissue contours | Extension |
| Colour and texture of skin | |
| Scars or sinuses | Power (tested against resistance of examiner) |
| Palpation | Each muscle group to be tested in turn. (Power of calf muscles is best tested with the patient recumbent and then standing) |
| Skin temperature | |
| Bone contours | |
| Soft-tissue contours | (Compare with other side) |
| Local tenderness | Stability |
| State of peripheral circulation | Integrity of ligaments—particularly the lateral ligament of the ankle |
| Dorsalis pedis pulse | |
| Posterior tibial pulse | Appearance of foot on standing |
| Popliteal pulse | Colour |
| Femoral pulse | Shape of longitudinal arch |
| ? Cyanosis of foot when dependent | Shape of forefoot |
| Movements (active and passive, compared with normal side) | Efficiency of toes |
| At the ankle: | Efficiency of calf muscles (? ability to raise heel from ground while standing on affected leg alone) |
| Plantarflexion | |
| Extension (dorsiflexion) | Gait |
| At the subtalar joint: | |
| Inversion-adduction | Condition of footwear |
| Eversion-abduction | Sites of greatest wear. (Compare with other side) |
| At the midtarsal joint: | |
| Inversion-adduction | |
| Eversion-abduction | |
| 2. GENERAL EXAMINATION | |
| General survey of other parts of the body. The local symptoms may be only one manifestation of a widespread disease | |
Assessing the state of the peripheral circulation
Clinical assessment. This is based on a study of the texture of the skin and nails, colour changes, skin temperature, the arterial pulses, auscultation, and exercise tolerance. Texture of skin and nails: The skin of an ischaemic foot loses its hair and becomes thin and inelastic. The nails are coarse, thickened and irregular. Ulceration of the tips of the toes may be noted. Colour changes. A brick-red rubor or cyanosis occurring when the foot is made dependent after a period of elevation (Buerger’s test) denotes serious impairment of the arterial circulation. Temperature: A foot with impaired arterial supply is colder than normal, but little reliance can be placed on this test as applied clinically at the bedside. Arterial pulses: The pulses to be felt for are the dorsalis pedis, the posterior tibial, the popliteal and the femoral. The popliteal pulse is often difficult to feel even in normal individuals. Palpation should be made with the fingertips of both hands supporting the slightly flexed knee. Pulsation of the dorsalis pedis artery is best felt at the dorsum of the foot between the bases of the first and second metatarsals. The posterior tibial artery is felt about 2 cm behind and below the tip of the medial malleolus. Absence or impairment of arterial pulsation is an important sign of defective circulation. It should be remembered, however, that a normal pulse is easily masked by thickening or oedema of the soft tissues. Capillary return: In limb ischaemia capillary return is slowed after blanching of a digital pulp or nail by pressure. Auscultation: A bruit over one of the major limb vessels, caused by turbulence of blood flow, may denote partial obstruction or an arterio-venous communication.
Special investigations. These may be indicated when the clinical examination shows evidence of vascular impairment. They include ankle blood pressure recordings, Doppler ultrasound probe analysis, combined probe analysis and ultrasonography, pulse volume recording (plethysmography), and digital arteriography. For more detail on these and the treatment of limb ischaemia readers should consult a textbook of vascular surgery.
Movements at the ankle and tarsal joints
Ankle movement. The ankle is strictly a hinge joint. The only movements are extension (dorsiflexion) and plantarflexion. The range should be judged from the excursion of the hindfoot rather than the forefoot, so that any contribution from the tarsal joints is disregarded. Similarly, in testing the passive range, the foot should be controlled from the heel (Fig. 19.1). The normal range of ankle movement varies in different subjects; so the normal ankle must be used as a control. An average range is about 25° of extension (dorsiflexion) and 35° of plantarflexion.
In clinical examination the range of movement contributed by each component can be determined separately. To test subtalar movement support the lower leg by a hand gripping the ankle. With the other hand lightly grasp the calcaneus from below (Fig. 19.2). Instruct the patient alternately to invert and evert the foot, observing the range through which the heel rocks from side to side. Compare with the sound foot. The normal range is about 20° on each side of the neutral position.
To test midtarsal movement grasp the calcaneus firmly so that subtalar movement is eliminated. With the other hand lightly grasp the midfoot near the bases of the metatarsals (Fig. 19.3). Instruct the patient alternately to twist the foot inwards and outwards into inversion and eversion, and compare the range with that on the sound side. The normal is a rotation of about 15° on each side of the neutral position.
Toe movements. Determine the active and passive range at the metatarso-phalangeal and interphalangeal joints. It should be remembered that the normal range of dorsiflexion of the great toe at the metatarso-phalangeal joint is nearly 90° (Fig. 19.4). The range varies, but limitation to less than 60° of dorsiflexion is certainly abnormal. The range of downward flexion is about 15° but it varies between individuals. Movement at the lesser toes is variable: there should be not less than 30° of flexion at the metatarso-phalangeal joints and at the interphalangeal joints.
Examination of the feet under weight-bearing stress
Instruct the patient to stand evenly on both feet. Observe the general shape of the ankle, foot, and toes. Study the shape of the longitudinal arch. Is it of normal shape? Is it flattened so that the navicular region is in contact with the ground (pes planus or valgus)? Or is it higher than normal (pes cavus)? It is important to view the heel from the back, so that any inward (varus) or outward (valgus) deviation may be noted. Next study the forefoot. Is it splayed and broader than normal? Assess the function of the toes. Normally they can be pressed upon the ground by the action of the intrinsic muscles so that the metatarsal heads are lifted up and relieved of weight-bearing pressure. Finally, examine the efficiency of the calf muscles. The crucial test is to ask the patient to stand on the affected leg and to raise the heel from the ground (see Fig. 19.5).
Examination of spine
Certain deformities of the foot – especially pes cavus with clawing of the toes – may be caused by a neurological abnormality in the thoraco-lumbar or lumbar region of the spine, associated with spina bifida or other developmental anomaly (see p. 171). Examination should therefore be made for a tell-tale dimple, pigmented area, or tuft of hair on the overlying skin.
Footwear
The examination of the foot is not complete until the patient’s shoes have been inspected and compared on the two sides. Note the position of greatest wear. When the foot is normal the greatest wear in the sole occurs beneath the ball of the foot and slightly to the medial side. In the heel it is at the posterior border slightly to the lateral side. The state of the uppers is also important: excessive bulging on the medial side suggests a valgus foot and excessive bulging on the lateral side an inverted foot.
Radiographic examination
When laxity of the lateral ligament is suspected a special inversion film is required. This is an antero-posterior projection taken while the heel is held in fullest inversion by an assistant. If the lateral ligament is torn or lax the talus will then be shown tilted in the ankle mortise (see Fig. 19.10, p. 433).
DISORDERS OF THE LEG
RUPTURE OF THE CALCANEAL TENDON
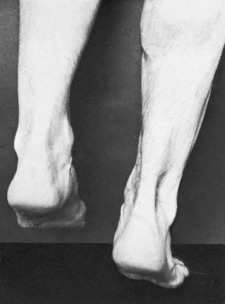
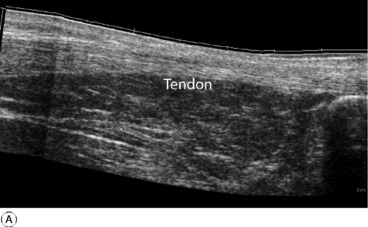
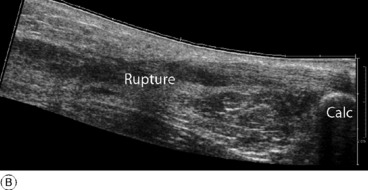
Diagnosis. The retention of some power of plantarflexion may deflect the unwary from the correct diagnosis. The crucial test is to ask the patient to lift the heel from the ground while standing only upon the affected leg (Fig. 19.5). This is impossible if the tendon is ruptured. In cases of doubt the gap in the tendon may be well demonstrated by ultrasound or MRI scanning (Fig. 19.6).
In the majority of younger patients, particularly those who wish to continue athletic pursuits after healing, operative treatment is preferable. It entails repair of the tendon, using non-absorbable sutures of synthetic material, tension on the suture line being relaxed by immobilising the limb with right-angled knee flexion and moderate ankle plantarflexion for 2 weeks. For the next four weeks a below-knee plaster with the ankle at 90° is worn. Certain protocols allow earlier mobilisation of the ankle under close supervision of a physiotherapist.
ACUTE OSTEOMYELITIS (General description of acute osteomyelitis, p. 85)
The pathological and clinical features and treatment conform to the general description on page 89.
CHRONIC OSTEOMYELITIS (General description of chronic osteomyelitis, p. 90)
Brodie’s abscess. This rather uncommon lesion was described on page 92. It is a special form of chronic osteomyelitis which arises insidiously, without a recognised acute infection preceding it. The tibia is the commonest site (see Fig. 7.7, p. 93).
SYPHILITIC INFECTION OF THE TIBIA (General description of syphilitic osteitis, p. 95)
Although skeletal syphilis is now rare in Western countries, it still occurs in other parts of the world, and when it does occur the tibia is often the bone affected. The infection may take the form of a localised gumma or of diffuse osteoperiostitis (see Fig. 7.11A&B, p. 96). There is a gradually enlarging swelling, with moderate pain. It is important to bear the possibility of syphilis in mind, because the swelling is easily mistaken for a tumour.
TUMOURS OF BONE
Benign tumours (General description of benign bone tumours, p. 106)
Chondroma
In the tibia or fibula this is seldom found except in multiple form in the condition of dyschondroplasia (p. 65). The individual tumours in this condition resemble enchondromata. They arise from the growing epiphysial cartilage plate, and they interfere with the normal growth of the bone. An important effect is that the growth of the tibia and fibula may be unequal, with the consequence that the bones may become curved or the plane of the ankle joint may be tilted away from the horizontal (see Fig. 6.4A, p. 65).
Malignant tumours (General description of malignant bone tumours, p. 112)
Osteosarcoma (osteogenic sarcoma)
This tumour usually affects the upper metaphysis of the tibia: the lower end of the tibia and the fibula are affected much less often. The tumour metastasises rapidly through the blood stream, especially to the lungs. Treatment was described on p. 117.
INTERMITTENT CLAUDICATION
Pathology. The basic disturbance is ischaemia of muscle, in consequence of which metabolites cannot be removed speedily enough when the muscle is exercised. The accumulation of metabolites is believed to be responsible for the pain, which subsides within a few minutes when the muscle is rested. The muscles usually affected are those of the calf, but in some instances other muscle groups are involved, according to the site of the arterial obstruction. The vascular lesion is usually a complete occlusion of the femoral or the popliteal artery. In claudication affecting the buttock the aortic bifurcation or the iliac artery may be occluded.
On examination there is objective evidence of impaired arterial circulation in the lower limb (p. 421). The posterior tibial, dorsalis pedis, and popliteal pulses are absent. There may be ischaemic changes in the skin of the foot. Evidence of widespread arterial or cardiac disease is nearly always found on general examination.
DISORDERS OF THE ANKLE
PYOGENIC ARTHRITIS OF THE ANKLE (General description of pyogenic arthritis, p. 96)
Pyogenic arthritis of the ankle is uncommon. The organisms reach the joint through the blood stream or through a penetrating wound; local spread from a focus of osteomyelitis of the tibia or fibula is rare because the bony metaphyses are entirely extra-capsular (see Fig. 7.2, p. 87).
TUBERCULOUS ARTHRITIS OF THE ANKLE (General description of tuberculous arthritis, p. 98)
Treatment. Early conservative treatment (p. 102) may restore a mobile ankle, but if in a resistant case articular cartilage is badly eroded or destroyed arthrodesis may have to be undertaken.
RHEUMATOID ARTHRITIS OF THE ANKLE (General description of rheumatoid arthritis, p. 134)
One or both ankles are often affected by rheumatoid arthritis in common with other joints in the lower limb, particularly the foot. There may be marked destruction of the articular cartilage and subchondral bone with pain, stiffness, and deformity (Fig. 19.7).
Treatment. Medical treatment is along the lines suggested for the disease as a whole (p. 137). Local treatment: In the active phase rest in a plaster is sometimes required, but in most cases the patient should be encouraged to remain active as far as possible, with such help as may be gained from local support by a moulded polypropylene splint. Operation is advised mainly when destruction of articular cartilage has led to intractable pain with marked impairment of capacity for walking. Arthrodesis and replacement arthroplasty are the methods available. Arthrodesis is usually the operation of choice because it gives permanent relief of pain with good function. If the subtalar and midtarsal joints are also severely affected they should be included in the fusion. Replacement arthroplasty of the ankle is appropriate in some patients (Fig. 19.8). The operation is technically demanding because of the limited surgical access to the joint, while the long-term results are much less satisfactory than with the hip or knee because poor bone support may lead to early implant loosening.
OSTEOARTHRITIS OF THE ANKLE (General description of osteoarthritis, p. 140)
Clinical features. The symptoms are pain which slowly increases over months and years, and limp. On examination the joint is a little thickened from hypertrophy of bone (osteophyte formation) at the joint margins. Movements are restricted slightly or severely according to the degree of arthritis.
Radiographs show the typical features of osteoarthritis – narrowing of the cartilage space, a tendency to sclerosis of the bone adjacent to the joint, and osteophyte formation at the joint margins (Fig. 19.9).
Surgical treatment should usually be by arthrodesis, which provides a painless stable joint for many years. A number of different methods are available to produce reliable bony fusion and with the introduction of arthroscopic techniques to remove the degenerate cartilage, combined with rigid internal fixation across the opposed bone surfaces, the post-operative rehabilitation is rapid. Unfortunately, after 10–15 years more than 50% of these patients develop further disability from hindfoot pain because of the accelerated onset of arthritis in the adjacent sub-talar and talo-navicular joints. In an attempt to overcome this problem in younger patients, replacement arthroplasty with resurfacing prostheses has been explored as a possible alternative (see Fig. 19.8). As with arthroplasty for rheumatoid arthritis, the long-term results are still uncertain because of bone resorption and implant loosening and it is not yet widely recommended.
RECURRENT SUBLUXATION OF THE ANKLE
When the lateral ligament of the ankle is torn and fails to heal there may be persistent instability with recurrent attacks of giving way in which the talus tilts medially in the ankle mortise. Anterior displacement relative to the tibial articular surface may also occur. The causative injury is always a severe inversion force.
Radiographic features. Routine radiographs do not show any abnormality. Antero-posterior films must be taken while the heel is held fully inverted. If the lateral ligament is torn or lax the talus will then be shown tilted away from the tibio-fibular mortise at the lateral side through 20 or 30° or more (Fig. 19.10). Anterior displacement of the talus relative to the tibial articular surface may sometimes also be demonstrated in lateral radiographs taken while the foot is pushed forwards.
Treatment. If the disability is slight it may be sufficient to strengthen the evertor muscles (mainly the peronei) by exercises, to enable them to control the ankle more efficiently. Stability may also be enhanced by broadening and ‘floating out’ the heel of the shoe. If the disability is severe operation is required. A new lateral ligament may be constructed either from the peroneus brevis tendon or from the peroneus tertius. Trials are also proceeding with the use of artificial ligaments, either as substitutes or as a means of promoting the growth of new ligamentous tissue.
DISORDERS OF THE FOOT
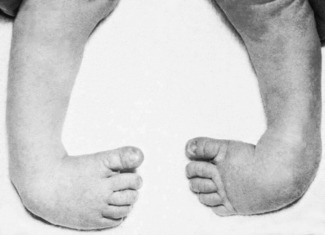
CONGENITAL CLUB FOOT (Talipes equino-varus)
The rather vague term ‘club foot’ has come to be synonymous in the minds of most surgeons with the commonest and most important congenital deformity of the foot—talipes equino-varus (Fig. 19.11). The less common, and usually less serious, form of club foot, talipes calcaneo-valgus, will be considered later under that title.
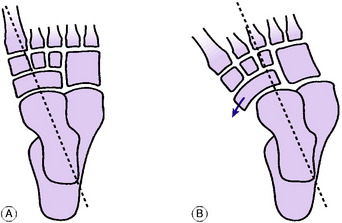
Pathology. The crucial component of the deformity is subluxation of the talo-navicular joint, so that the navicular bone lies partly on the medial aspect of the head of the talus instead of on its distal aspect (Fig. 19.12). The soft tissues at the medial side of the foot are under-developed and shorter than normal. The foot is adducted and inverted at the subtalar, midtarsal, and anterior tarsal joints, and is held in equinus (plantarflexion) at the ankle. In most cases under-development of the calf and peroneal muscles is a striking feature. Thus if only one foot is affected there is a marked discrepancy in the girth of the calf between the two sides.