CHAPTER 17 The latarjet procedure—technique and fixation constructs
 Optimal bone contact, blood supply and fixation strength are important for optimal coracoid graft healing.
Optimal bone contact, blood supply and fixation strength are important for optimal coracoid graft healing. The proposed classifications allow us to predict the likely region of osteolysis on the coracoid graft.
The proposed classifications allow us to predict the likely region of osteolysis on the coracoid graft.Introduction
The Latarjet procedure,1 first described in 1954, involves coracoid bone transfer to stabilize the shoulder by the static action of the transferred bone block and its attached coracobrachialis tendon sling. Although coracoid graft transfer often successfully stabilizes anterior shoulder instability for a selected group of patients,2 eventual osteolysis of the transferred coracoid bone graft has been reported.3,4
The glenoid bone graft prevents engagement of a humeral head bone lesion by extending the glenoid arch to such a degree that the shoulder cannot externally rotate far enough for the Hill-Sachs lesion to engage the front of the graft.5
An important factor contributing to shoulder stability after a Latarjet procedure is the “sling effect” from the conjoined tendon that slings across the anterior-inferior capsule when the shoulder is in 90 degrees abduction and 90 degrees external rotation. This mechanism acts to prevent engagement of the Hill-Sachs lesion even before the anterior capsule is repaired. Stability from this “noncapsular Latarjet procedure” also is contributed from an increased tension in the inferior fibers of the subscapularis muscle due to the transferred coracoid graft with its attached conjoined tendon over the top of the lower subscapularis tendon. Because we trust in the effects of the Latarjet procedure,6,7 we do not stress any capsular repair on the glenoid or any capsular reinforcement.
Revision surgery after a failed Latarjet reconstruction is complex, and the success of revision surgery is low. This procedure should therefore be carefully performed.4 In Burkhart,8 Allain,3 and Hovelius9 series, where the capsule is restored on the glenoid margin or in overlap fashion, mild or residual instability is reported at 5%, 12%, and 7%, respectively. At our surgical center, we have reported a rate of around 10%.
Coracoid graft osteolysis concept and proposal of classification system
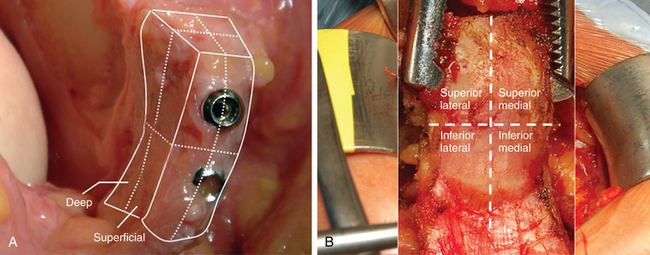
For there to be proper bone healing, there should be good contact between the coracoid bone graft and the glenoid bone bed, an adequate blood supply from the coracoid bone graft and the glenoid bone surface, and satisfactory mechanotransduction (mechanisms by which mechanical cues modulate bone healing) at the bone healing site. To date, no classification for coracoid bone graft osteolysis has been described that illustrates how these different factors come into play. We present our understanding of coracoid osteolysis and a classification system that divides the coracoid bone graft into eight regions. The two major regions are superficial and deep, which in turn are each divided into superior, inferior, medial, and lateral (Fig. 17-1).
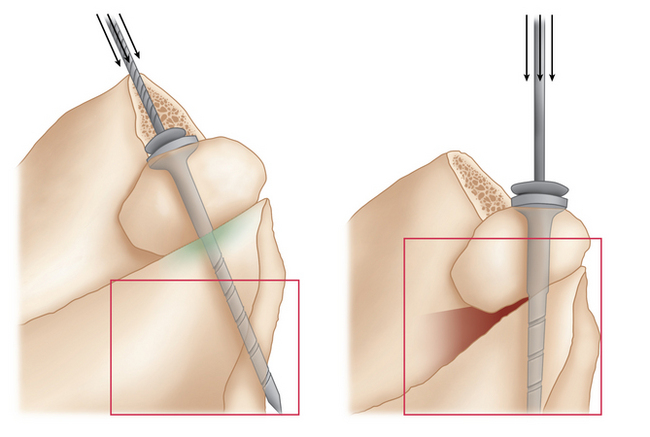
During the Latarjet procedure, screws for fixation of the coracoid bone graft to the glenoid neck surface should be directed posteromedially because of the steep glenoid neck surface rather than positioned at 90 degrees to the coracoid bone and glenoid neck bone surface. This is done to avoid penetration into the shoulder joint. Because of this, there tends to be a mismatch of the medial aspect of the coracoid bone graft and the corresponding glenoid neck bone surface, which can affect the healing of the medial side of the bone graft. There tends to be good contact between the graft bone surfaces in the lateral regions of the coracoid graft (Fig. 17-2).
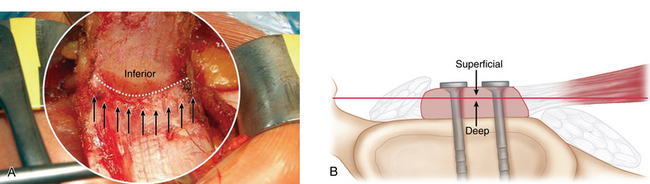
The blood supply of the coracoid bone graft arises from the coracobrachialis attachment, which is on the inferior region of the graft. This promotes healing in the region. The contact of the glenoid bone surface blood supply with the coracoid graft promotes healing in the deep regions of the coracoid graft (Fig. 17-3).
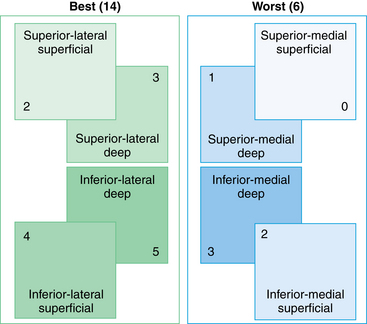
Mechanotransduction factors can modulate the healing of bone graft.10,11 The humeral head tends to influence and promote healing of the lateral regions of the coracoid graft. The coracobrachialis attachment sling on the inferior regions of the graft tends to promote healing of the graft’s inferior regions (Fig. 17-4). If each of these factors is given a score of 1, the superficial superomedial region has the lowest score, which corresponds to our findings on computed tomography studies that indicate that osteolysis most often occurs in the superficial superomedial region. The classification system produces an overall score of 6 on the medial side of the graft and a score of 14 on the lateral side (Fig. 17-5 and Table 17-1). The medial region of coracoid graft therefore has less favorable healing potential compared with the lateral regions.
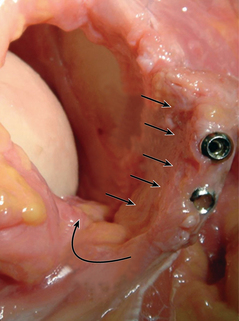
FIGURE 17-4 Mechanotransduction forces from the humeral head and the coracobrachialis attachment sling.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree