Fig. 63.1
Accurate surgical planning requires a systematic and comprehensive diagnostic approach. This worksheet embodies one such approach. The eight possible diagnoses that lead to revision surgery are listed in the left-hand column. This constitutes a “differential diagnosis” as well as a sequential algorithm for clinical evaluation. Data points necessary to confirm each diagnosis and plan the revision occupy the cells to the right. “Systematic” evaluation means that every problem TKR is evaluated according to this method. “Comprehensive” means that even if one diagnosis is discovered (e.g., sepsis), all of the rest must also be considered. An infected TKR may also have a ruptured extensor mechanism, and a stiff TKR might also be infected
Papers often tout the advantages of specific implants for revision, suggesting that products are the answer when in fact clear thinking, solid principles, and a sound concept of how to set the knee “right” will prevail [27, 28]. The surgeon whose first question is: “which prosthesis do I use” is generally asking the wrong question. Despite the appeal of technology for salvage, experienced surgeons remind us to exercise caution with this approach [29].
There is a bias against reporting poor results, perhaps because failure attracts neither admiration nor future patients. And yet, we would learn more from the analysis of what went wrong than reports of what went right. Published results tend to be interpreted optimistically. Some midterm follow-ups report mostly short-term follow-ups, converted by survivorship analyses into longer-term studies [23].
Only two registries track revision TKR [30, 31]. Australia limits their assessment to first revisions for aseptic failure and does not report the reasons for failure of the revision [32]. The New Zealand registry tracks the small number of second (and third and fourth) revisions with deep infection (41.6 %), loosening (31.5 %), and instability (8.7 %) the main causes of failure.
There is even less information for the “endgame” that hazardous time after a revision fails when “few pieces are left on the board,” but before “checkmate” when the arthroplasty and patient are in jeopardy. Innovative surgeries in difficult circumstances become case reports if successful: failures are rarely submitted to journals. If that successful procedure were performed 100 times, how often would it succeed? In clinical situations where decisions are more important than products, studies rarely reveal how patients were selected for unusual surgery and who was declined.
63.2 How Failures Fail: Again
We know how primary TKRs fail and accordingly why revisions are performed [20, 26, 33, 34]. While we can characterize how revision knee replacements might fail [26], we lack good clinical data as to how they actually do fail, much less why [21].
The data on failed revision TKRs is clear on one point: infection is problematic [22, 23, 35]. Mortazavi et al. evaluated 476 knees between 25 and 159 months after revision. Sepsis was the reason for revision in 19 %. Deep infection complicated 9 % of cases overall, and 21 % of cases that had been revised for sepsis [35].
A review of 349 revision TKRs concluded that infection (31.25 % of their failed revisions), instability (18.75 %), and loosening (15.63 %) were the main reasons that revision surgeries fail. Twenty-nine cases were revisions of unicompartmental knee replacements, and there was a heavy dependence on constrained implants in a series of “first” revisions (non-linked constrained in 42.7 % and rotating hinges in 21.2 %). A variety of fixation methods were used, including the tenuous combination of constrained implants without additional fixation. The conclusion of a survivorship analysis was reported, remembering that this is a statistical technique designed to predict survival of all cases at the duration of the longest followed case, with the important assumption that all cases will be subject to the same probability of failure. Accordingly, the predicted values applied to those followed for only one year are a source of concern, especially when the authors indicate a growing preference for constraint as the study period progressed [23].
Suarez et al. [22] reported 566 revision TKRs (16 deceased and 58 lost) in a paper remarkable for its candor but confusing in the broad mix of surgeries that qualified as “revision”: 342 complete revisions, 116 single-component revisions, and 108 isolated polyethylene exchanges. They concluded that isolated polyethylene exchange and single-component revisions should probably be avoided in favor of full revisions. The highest failure rate was noted in the group treated for infection where 61.5 % succumbed to recurrent or persistent sepsis, but their data are confounded by the cases treated with open debridement and polyethylene exchange (ODPE). Overall, 12 % failed at an average of 40 months. Aseptic loosening occurred in 19 % of them and instability in 13 % [22]. Poor motion [36] and extensor dysfunction can be added to significant problems in revision TKR.
63.3 The Path to Calamity
Infection is common to most cases that end badly, often preceded by several “simple” interventions that seemed “worth a try.” These decisions are never easy, as surgeons are frequently criticized either for doing too much or not enough. All surgeries, even those regarded as “easier” or less risky, should be condemned if performed without an incisive evaluation [26] followed by definitive and timely action directed at the root cause of a problem.
Simple complications can easily become serious. Sepsis often complicates fixation of the fractured patella in knee arthroplasty [37, 38]. Without effective surgery, extensor ruptures can deteriorate to destructive recurvatum instability from a compensatory “back-knee gait.”
Simple procedures are seductive. Isolated polyethylene exchanges for stiffness or instability [27, 28], single-component revisions, and revision with primary [39] or unicompartmental components [40] have a low probability of success, but can still result in infection. Arthroscopy has been advocated for problem TKRs [41–43]. Arthroscopy of arthroplasties has been complicated by infection [43, 44]. Once infection occurs, arthroscopic debridement cannot eliminate purulent material between the metal and plastic components and should be avoided.
Wound problems without deep sepsis require prompt, aggressive, and usually surgical attention [45, 46]. John Insall’s position: “we condemn procrastination and the prolonged use of oral antibiotics, when infection is only suspected and not confirmed by bacteriological evidence” [47] still applies. When the obligatory arthrocentesis identifies deep sepsis [48], treatment shifts from wound management to periprosthetic infection. New information on the definition of periprosthetic infection [49], guidelines for diagnosis of established sepsis [48, 50], and quantification of fluid aspirated acutely after surgery provide essential guidance [51].
Arthrotomy and debridement with obligatory modular polyethylene exchange (ODPE) can be justified during a short interval after primary TKR or immediately after the onset of infection from hematogenous spread. There is discouraging evidence that failure rates may exceed 80 % when Staphylococcus aureus is the organism [52]. Furthermore, clinical experience suggests that failed debridement may contribute to failure of an eventual two-stage protocol [52, 53].
The ideal treatment of periprosthetic infection is covered in Chaps. 46, 59 and 60. Some surgeons advocate a single-stage treatment of selected infected arthroplasties [54], acknowledging that success rates, though good, may fall short of those achieved with two-stage procedures [55]. If we are intent on protecting patients from catastrophic outcomes, we may choose the approach that yields the fewest failures.
If infection is suspected in all painful primary TKRs, it should be assumed in all problem revisions.
The rules are:
Simple solutions may not exist for complex problems. A multicenter report of bilateral infected TKRs concluded that simultaneous bilateral resection arthroplasties and a two-stage reimplantation protocol were superior to less aggressive attempts to salvage the prosthesis surgically [58]. This is a daunting surgery and not for the uninitiated. Many catastrophes result from well-intentioned but failed procedures. To paraphrase an aphorism, “the road to amputation is paved with good intentions.”
63.4 The Infected Revision
In a benchmark paper, surgeons at the Mayo Clinic reported results at a mean 7.2 years (range 0.1–9.8 years) for 94 infected TKRs treated with a two-stage reimplantation. The survivorship (free of implant removal for any reason) was 90 % at 5 years and 77.3 % at 10 years. The survivorship free of reinfection was 93 % at 5 years and 85 % at 10 years [59]. These excellent results from experienced surgeons nonetheless include 7 % failures at 5 years and 15 % at 10 years. These patients face a difficult situation.
Another study tracked 20 patients who suffered persistent infection after a two-stage protocol for an infected TKR. The results were discouraging with ten solid arthrodeses, five persistent infections on suppressive antibiotics, four above-knee amputations, three pseudarthroses after attempted arthrodesis, and one permanent resection arthroplasty. Only one in twenty had a successful, functioning reimplantation after a second two-stage protocol [60] (Fig. 63.2).

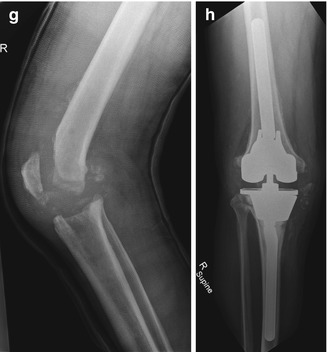

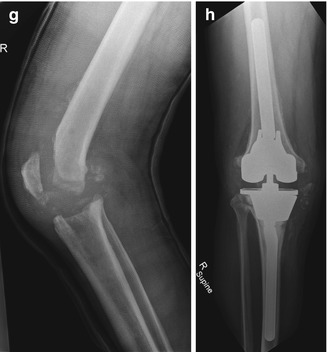
Fig. 63.2
(a) Lateral radiograph of an infected TKR 18 weeks after surgery. Wound drainage was treated with “washouts” but not modular polyethylene exchange: 1 at 16 days and another 2 days later. This means that pus between the metal and the polyethylene would not have been cleared. No cultures were obtained, and the wound eventually closed with antibiotic therapy. Because of persistent swelling, an aspiration was performed in week 11, but was reported as a “dry tap.” (b) Lateral radiograph showing extrusion of a commercially available antibiotic-impregnated polymethyl methacrylate (PMMA) articulating spacer, very soon after placement: skin staples and drain still in place. This surgery, performed 20 weeks after the primary, was necessitated by persistent wound problems. Cultures obtained at surgery grew methicillin-resistant Staph aureus (MRSA) an organism less likely to be eradicated by prior simple surgeries [54]. There may be residual PMMA from the primary TKR in the tibial canal (arrow). This type of spacer probably requires additional PMMA that has been heavily loaded with antibiotics, for additional nonpermanent fixation to prevent dislodgement and increase local antibiotic concentration. (c) Anteroposterior (AP) radiograph of the second spacer; non-articulating antibiotic-impregnated PMMA placed at 22 weeks after primary TKR and left in place for 29 weeks. (d) A reimplantation performed at week 51, with an uncemented metaphyseal engaging stem in the femur and non-linked constrained prosthesis. The patella has never been resurfaced, and there is concern that the avascular articular cartilage may harbor bacteria. (e) Clinical photograph at 59 weeks: several days after, a third debridement was performed. The patient did reasonably well for 2 months after the reimplant and then presented with sepsis and wound drainage. Infection could not be controlled. (f) AP radiograph after initiation of a second two-stage reimplantation protocol. Aggressive bone resection and debridement of the medullary canals have been combined with a classic protocol, using no spacer. (g) Lateral radiograph of the second resection arthroplasty demonstrating that medullary canals are clear and, despite bone resection, extensor mechanism is intact. (h) AP radiograph of the second reimplantation, with trabecular metal cones in both the tibia and femur to reconstruct bone and augment fixation. Fixation for the non-linked constrained implant has been achieved with uncemented, diaphyseal engaging stem extensions. This healed well without recurrent problems until the patient’s demise a year later from myocardial infarction
Hart and Jones reported six persistently infected cases after 48 two-stage revisions for sepsis. Two remained on chronic suppressive antibiotic therapy, and four had further surgery resulting in successful reimplantation in two and arthrodesis in two. Azzam et al. reported better results: 4 failures in 18 patients at 24–83 months, perhaps because of better techniques but possibly due to more cautious patient selection [61]. For unexplained reasons, Backe et al. reported uniform eradication of infection after failure of a two-stage reimplantation with a second two-stage protocol followed by arthrodesis in three and reimplantation in nine cases.
Cierny and DiPasquale [62], supported by McPherson et al. [63], clarify the situation, by focusing the attention on the patient’s ability to recover from periprosthetic infection.
Type “A” hosts are “healthy and without healing deficiencies.”
Type “B” patients are compromised by local or systemic problems.
Type “C” hosts are not considered candidates for aggressive surgery (Table 63.1).
Table 63.1
Cierny hosts
A
B
C
Local
Systemic
No compromise
Chronic lymphedema
Malnutrition
Unfit for surgery
Venous stasis
Immune deficiencies
Major arterial disease
Chronic hypoxia
Arteritis
Malignancies
Extensive scarring
Diabetes mellitus
Radiation fibrosis
Extremes of age
Retained foreign body:
Chronic tobacco use
Suture, buckshot
Major organ failure
Of the factors that compromise the knee “locally,” scarring can be improved by tissue transfer where feasible [64]. Malnutrition and blood glucose control in diabetics, along with cessation of smoking, can improve outcome of treatment for infection in systemically compromised patients. Otherwise, the results correlate very closely with the patients’ status (Table 63.2). Reliable serologic testing to clear the way for reimplantation may be important [65].
Table 63.2
Results of two-stage protocols by Cierny category
Patients in two-stage protocol | A | B | C |
|---|---|---|---|
Percent: reimplantations attempted | 91 | 66 | 24 |
2-year survival rate | 100 | 86 | Zero |
Surgical debridement remains the cornerstone of effective treatment for infection. Persistent infection implies chronic osteomyelitis [66–68], sequestrae, and biofilm formation [69–71] necessitating more aggressive surgery. Fungal infections may complicate chronic infection especially in compromised hosts [72, 73], and necrotizing fasciitis [74, 75] has been described as a complication of TKR. There is a need for innovation, and as an example, local administration of high-dose antibiotics has been encouraging [76].
63.5 First Choice Reimplantation: The Challenges
63.5.1 Soft Tissue Envelope Loss
Compromised integument is a formidable obstacle to reimplantation. Tissue expanders [61, 62] are only feasible before trouble starts, and this is the preferred time for tissue transfers as well. The timing of transfers differs for trauma patients, where osseous union is the priority despite infection. Accordingly, infection can be treated with hardware removal and debridement after fractures heal. By contrast, an arthroplasty is lost if infected. As a result, preemptive soft tissue transfers to prevent infection may be necessary.
While exposed prostheses were covered with gastrocnemius flaps in early reports [77–79], these arthroplasties are ipso facto infected, and it is now acknowledged that they will often have to be removed if the flap is to survive [80]. The flap that is turned unsuccessfully to “save” an exposed prosthesis will have been an unfortunate gambit. It is better to remove the prosthesis, control the infection, and create a hospitable environment for the flap. Later reports emphasize the utility of early (prior to bacterial colonization) reconstruction with the gastrocnemius [64, 65] and other flaps [66–70] prior to arthroplasty, concurrent with reimplantation or at the second of a two-stage protocol for infection [64, 81]. In some cases, an “interval” or third procedure, turning the flap onto the resection arthroplasty, will be optimal, still leaving reimplantation and arthrodesis as later options. Tissue transferred to close a revision prolongs surgery and increases infection. Postoperative immobilization risks stiffness.
Concomitant soft tissue envelope and extensor mechanism loss has been treated with gastrocnemius flaps [82–84], extending the Achilles tendon into the extensor defect, or latissimus dorsi free flaps combined with extensor mechanism allografts [85]. Infection and extensor rupture often require arthrodesis. Negative-pressure dressings (vacuum therapy) may have a limited role in treating some superficial wound problems, perhaps in the obese [86]. Salvage of an exposed prosthesis with these devices is unlikely, despite the occasional fortuitous short-term reports [87].
63.5.2 Extensor Mechanism Loss
Rupture of the extensor mechanism may be the worst complication in knee arthroplasty, and numerous reconstructions have been described [88, 89]. The results of extensor mechanism allograft are probably the best, but depend heavily on a complicated surgical technique [90, 91]. The reconstructed extensor must be very tight at the completion of surgery, so that as the chronically contracted quadriceps eventually stretches to its normal length, extensor power is maintained. At surgery, the medial and lateral host capsule should meet and cover the allograft, concealing it inside the joint. This can be difficult distally, where the allograft tubercle is embedded in a trough and a muscle flap may be necessary. Achilles tendon allografts necessarily weave allograft from inside the joint distally to outside the joint over the patella, leaving the arthrotomy breached by foreign material [92].
When extensor rupture is combined with extensive loss of the proximal tibia, a proximal tibial allograft that includes the extensor mechanism is a logical solution [93]. Extensor loss may accompany knee dislocation when the extensor is the last structure holding an unstable arthroplasty together. The arthroplasty should be revised for stability when the allograft is reconstructed. Reconstitution of the extensor mechanism over an unstable arthroplasty, no matter how creative, is misguided [94].
The cause and effect may be difficult to distinguish when infected arthroplasties also have ruptured extensor mechanisms. Perhaps bacteria eroded the extensor, or mechanical rupture exposed the joint to colonization. While these patients may be treated with a two-stage protocol including an extensor allograft at reimplantation, arthrodesis is often recommended.
63.5.3 Ligamentous Compromise
Surgery for instability has the potential for the best results of any revisions [95, 96]. Three basic modes of instability should be considered: coronal, sagittal, and flexion.
Coronal or varus-valgus instability will be the most familiar, where alignment and dynamic gait alterations contribute to the problem. Cases where revision for instability has failed include hip abductor dysfunction, scoliosis, and tibial posterior rupture in addition to the obvious implications of knee alignment. An arthroplasty that has failed with valgus instability cannot be expected to succeed if the post revision alignment remains in excess valgus. Heavily constrained implants are less important than an accurate evaluation and correction of the deforming forces responsible for the problem. In some cases, allograft reconstruction of collateral ligaments is a useful adjunct to revision [97]. Ligament reconstructions without revision fail [98] with rare exception [99].
Sagittal instability takes the form of recurvatum or fixed flexion contractures with buckling. Recurvatum from component subsidence responds to restoration of the arthroplasty, although serious technical problems ensue from extreme loss of the distal femur. Recurvatum from neurologic quadriceps paralysis is best treated with arthrodesis. Buckling may result from patellar dislocation, where revision will address axial alignment and the rotational position of tibial and femoral components [100]. When chronic ruptures of the extensor or patellectomies are responsible, extension power should be restored to eliminate the causative “back-knee” gait [88]. Implants with mechanical hyperextension stops provide stability initially, but are subject to mechanical overload and breakage or loosening [101, 102].
Flexion instability generally results from a flexion gap that is larger than the extension gap and where the modular tibial polyethylene insert was chosen to achieve full extension, at the expense of stability in flexion. Full revision is preferred [24]. With the exception of extensor problems, there is usually adequate host tissue for straightforward and highly successful surgery. Few of these problems should ever proceed to the salvage situation, unless complicated by sepsis or extreme tissue loss.
63.5.4 Bone Deficiency from Osteolysis and Surgery
Engh and Park described three levels of bone loss in 30 patients where the most severe or “type III” [103] involved metaphyseal defects requiring “bulk allograft or custom components.” There were no failures in the initial report at 24–120 months [104]. In a review of a different but probably overlapping cohort of 54 revisions [89], 17 cases had failed, though fewer failed amongst those where bulk allograft (usually the femoral head) had been used.
Two points emerge:
1.
There were fewer failures amongst the presumably more severe failures where bulk allograft was used, favoring definitive even if more extensive surgery.
2.
Salvage scenarios do not arise primarily from large bone defects—they arise when the first surgical reconstruction for them fails, especially if it becomes infected, ergo the advantage of definitive surgery at the outset.
Extensive bone loss is not simply a matter of replacing missing material with allograft or metal. The real problems are component fixation and sizing. Consider how much surface area is available for the “bond” between augment or graft and the deficient host anatomy and how load will be transferred. In addition, as the bone is lost from the proximal tibia, the circumference diminishes along with the cancellous bone, until only a narrow, sclerotic cortical rim remains. The residual cortical perimeter accommodates a disproportionately small tibial component. Eventually, both the flexion and extension gaps are spacious. The extension gap can be filled with distal femoral augmentation and thicker polyethylene, but there will be limits to the size of femoral component, essential in managing the flexion gap, that can be coupled with an unnaturally small tibial component. The usual recourse when soft tissue tension cannot be restored is to increase constraint. Unfortunately, increased constraint and poor fixation is a dangerous combination, and failure leads to the “endgame.”
Sculpted allografts that maximize surface contact area with host bone have been serviceable [96, 105, 106]. Newer porous metal augments, because of their superior fixation qualities [107], have largely replaced conventional augments and structural allografts for large defects. While structural allografts have been used once infection is eliminated [106, 108, 109], avascular bone is undesirable when bacterial colonization is possible. The unique surface geometry of trabecular metal components seems to resist bacterial colonization [110, 111]. These devices liberate surgeons to debride aggressively and control infection. In low-demand patients, massive bone loss and ligamentous instability are sometimes ignored, with hinged implants that are otherwise reserved for tumor surgery [112, 113].
63.5.5 Skeletal Loss from Periprosthetic Fracture
Conventional internal fixation of supracondylar femur fractures with and without knee replacements usually succeeds [114–121]. Revision TKR is feasible if fixation fails [122]. Both unoperated arthritic knees [123–126] and primary TKRs complicated by supracondylar fractures have been treated with revision-style prostheses. Some periprosthetic fractures have been reconstructed with the clever addition of intramedullary stem extensions to accommodating femoral components [127, 128]. Bolder approaches may be necessary for aseptic failures with osteopenic bone, comminuted fractures, and loose components (Fig. 63.3). Distal femoral comminution can be discarded and the arthroplasty reconstructed with distal femoral allograft [129], distal femoral replacement prostheses [126, 130], “mega-prostheses” [112], “tumor prostheses” [131], or “resection prostheses [113, 125]”. In general, these function well in highly selected cases, but the loads sustained by the devices can predispose to mechanical failure [132].


Fig. 63.3
(a) Radiograph of a Stanmore hinged arthroplasty 18 years after TKR in a male patient now aged 81 years. (b) There is extensive osteolysis in the distal femur and a full-thickness defect in the posterior cortex at the tip of the femoral stem. (c) A periprosthetic fracture has occurred at the tip of the stem. (d) Some callous has formed with the bones malaligned. The limb is neither comfortable nor functional. The goals of further surgery have been specified preoperatively: (1) stabilize the fracture, (2) revise the loose hinge, (3) restore secure fixation, (4) and bypass and reconstruct bone defects. This will be a challenging surgery, but the plan is definitive and does not ignore any of the clinical problems. The arthroplasty is not infected. Any surgery that does not address all problems and that might then become infected could preclude successful reconstruction in the future. (e) AP radiograph of revision with a linked (i.e., hinge) fully constrained implant that has stabilized the fracture with extra long, press-fit stem extensions. Fixation has been augmented with step cones in the metaphysis to aid rotational fixation, and bone graft has been applied to the fracture site and areas of deficient cortex, satisfying all the goals of the procedure. (f) Lateral radiograph with healed fracture. (g) Lateral radiograph showing flexion to 60°
Infected fracture fixation is a serious salvage situation fraught with complications. Bezwada reported one above-knee amputation in 30 periprosthetic fractures treated with open reduction and internal fixation, but complicated by infection [133]. Tumor-style prostheses enable very aggressive debridement of infections, but these expensive implants may be wasted if infection persists. Insightful treatment based on chess-like algorithms is appropriate [134].
63.5.6 Combined Infection and Bone Loss
When infection is accompanied by significant bone loss, arthrodesis will be technically difficult and resection arthroplasty inutile, leaving amputation or reimplantation as options. A two-stage reimplantation protocol is recommended, but stabilization of the interval construct is challenging. Embedding intramedullary fixation nails, heavy Steinman pins, or spinal rods in antibiotic-impregnated methacrylate cement and placing them between the tibia and femur as a non-articulating spacer block during a two-stage protocol have been in wide practice (Fig. 63.4). Two groups have reported similar techniques in incomparably heterogenous patient groups [135, 136]. Technically, one group covered all exposed metal with antibiotic cement, and the other did not. There is no basis to claim the results of one are better than the other [136].


Fig. 63.4
(a) Anteroposterior and (b) lateral radiograph of a multiple operated knee undergoing a second two-stage reimplantation protocol. Aggressive debridement leads to extensive bone loss. A non-articulating methyl methacrylate spacer, loaded with high doses of antibiotic powder, has been placed in the knee. It is stabilized with heavy Steinman pins that overlap inside the bulk of the spacer. This facilitates removal at reimplantation. An incompletely successful attempt has been made in this case, to coat the pins entirely with antibiotic cement
There is one pertinent case report on the subject of infection and extensive bone loss, although the failed arthroplasty was of the hip. The spacer used here is a long-stem hip prosthesis, covered in antibiotic-impregnated methacrylate and embedded in the residual distal femur. The final implant is undeniably a “total femoral replacement,” including excision of the distal femur and knee reconstruction with a hinge attached to the hip femoral stem. This technique, with a true “total femur spacer”, can be adapted to the treatment of an infected revision TKR below a hip arthroplasty, which usually has a colonized medullary canal. This case report adheres to principles: aggressive (and potentially calamitous) debridement of contaminated and devascularized tissue, with removal of foreign material and biofilm [137].
Macmull et al. reported a sophisticated, albeit expensive, approach in 19 difficult cases, where two custom-fabricated, mega-prostheses (Stanmore Modular Individualized Lower Extremity System) were used to treat infection in cases of extreme bone loss—the first as an articulating spacer and the second for definitive reconstruction. The formidable surgery may be precisely the feature that enables extreme debridement and success. Infections had been present for a mean of 23 months (range 4–71), and all had failed debridement with antibiotic therapy. Excluding simple debridement, these patients had a mean of 3.7 failed surgeries (range 1–17 procedures) [138] (Fig. 63.5)
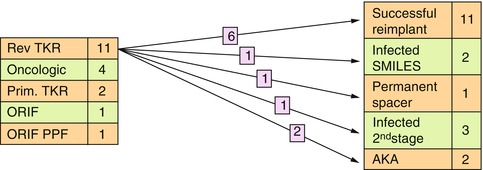
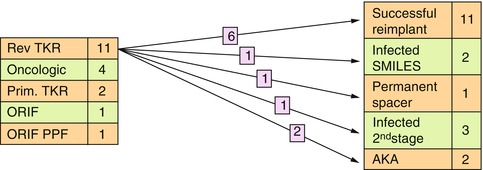
Fig. 63.5
Results of one of the few published series that include treatment of infected revision TKRs. The protocol used a sophisticated custom-made hinged spacer followed by a second custom-made hinged implant. Table on the left lists indications for entry into the protocol. The table on the right lists the outcomes for all cases from the table on the left. The numbers on arrows connote the specific results for the infected revision TKRs, with 6 of 11 (54 %) succeeding
63.5.7 Ipsilateral Total Hip Replacement
Periprosthetic fractures between hip and knee replacements are problematic if not disastrous. Hip stems compromise the endosteal blood supply, and strut allografting or plate fixation disrupts the cortical circulation. A knee prosthesis constrained in the coronal plane creates a large lever arm extending from the hip to the ankle, with a bending moment focused on the fracture site. It may be tempting to plate these diaphyseal fractures as if no arthroplasties were present, but huge loads and avascularity portend failure and disaster if infected. While it may seem unjustified to sacrifice a well-fixed hip arthroplasty stem, early reconstruction of a periprosthetic fracture between a hip and a stemmed constrained TKR with a “total femur replacement” can be a more direct route to success [139–142]. Alternately, custom-fabricated intramedullary stem extensions have been linked to hip stems for revisions, and custom arthrodesis devices have been linked for fusions [143].
Once sepsis occurs, ipsilateral hip prostheses may render the infected limb incurable, remembering that the medullary canal is a likely source of positive culture material [63]. Infected biofilm on the hip stem and cement will not be eradicated by knee resection even with debridement of the canal. The “total femur” approach may be required for limb salvage. Tragically, if this technique is used only after failed surgeries end in sepsis, success may not be possible.
63.6 Second Choice: Arthrodesis
Arthrodesis is rarely performed and with good reason. Although it can theoretically provide a comfortable, stable limb, the patient will probably abandon simple activities like cinema and public transportation. Women are unable to negotiate most public lavatories. In cultures where high flexion is important, arthrodesis is crippling. Even the patient with an above-knee amputation can be more easily taken on and off a modern jet liner in the standard aviation wheelchairs. Persistent knee pain has been reported in 15–36 % of knees fused after failed TKR [144].
In favor of arthrodesis, Somayaji et al. [145] remind us that while the energy cost, as measured by oxygen consumption, of ambulation with an arthrodesis is 30 % greater than normal [146], walking with an above-knee amputation is a further 25 % higher than a fusion [147]. That, combined with the revulsion at loss of a limb and the patient’s ability to get up in the middle of the night without donning a prosthesis, provide support for fusion. Two papers argue that patients with arthrodesis may enjoy levels of independent lifestyle comparable to those with revision TKR. Benson et al. conceded that revision patients did better on global scores, observing however that for 6 of 8 SF-36 categories, the two groups were equivalent [148]. DeVil et al. studied 19 arthrodesis patients and concluded that the functional results, as evaluated by SF-36 and “Oxford 12-item knee scores,” were comparable to revised hinged arthroplasties. Contrary to conventional wisdom, patients have been reported who requested contralateral arthrodesis after one TKR failed and was fused, resulting in bilateral stiff knees [149].
Arthrodesis for failed TKR has been the subject of numerous reviews [145, 150, 151]. Conway et al. concluded that the most common indication for knee arthrodesis as of 2004 was pain and instability in an unreconstructable infected TKR [146]. They argued for the superiority of arthrodesis over amputation.
The most common reason for arthrodesis of a failed TKR at present is infection that cannot be controlled. And yet, a generation ago, arthrodesis was often preferred over revision TKR [152]. This means that fusions were attempted with minimal bone loss and sometimes without infection. Despite this, surgeons from Harvard Medical School reported a 30 % pseudarthrosis rate, problematic limb shortening, and poor function [153]. Woods et al., using classic techniques to eradicate infection first, reported better union rates with external fixation devices [154]. Knutson reported 4 failed TKRs fused with intramedullary rods and then published a national review of 91 cases, three quarters of which had failed for infection. Two died of infection and four required amputation. Fusion, with a variety of techniques, was achieved in only 50 % of cases [155]. A final series of twenty cases demonstrated improved results with intramedullary devices as well as external fixators, but only after multiple surgeries [156].
A fundamental problem with arthrodesis is timing. Most patients refuse arthrodesis until the alternative is amputation. By then, lost bone and soft tissue plus established infection indicate that the opportunity for fusion has passed. Rand et al. reported 145 failed TKRs treated with arthrodesis: at 1 year 25 (21 %) failed, as defined by nonunion attributable to bone loss [157]. The decision to fuse, though difficult, is best made when other options still seem viable. Infection should be controlled as a condition for arthrodesis with the possible exception of external fixation techniques [158]. Persistent infection complicating a solid arthrodesis was reported in two patients treated with external fixation. As with trauma care, union was achieved first, and then infection was treated surgically [159].
The ideal technique for fusion is difficult to ascertain, as many modern clinical series include mixed indications and techniques. A meta-analysis of five series by Damron and McBeath concluded that intramedullary nail arthrodesis offered higher union rates, but that gram-negative and mixed flora infections were risk factors for failure [160]. Mabry et al. reached similar conclusions about the superiority of IM nailing [161] as did Yeoh et al. [162]. Klinger et al. reported 20 infected TKRs that were treated with arthrodesis between 1990 and 2002. There were multiple indications for fusion, including bone or soft tissue loss, poor bone quality, and recurring infections. External fixation was selected for 18 single-stage procedures, and two cases received intramedullary fixation in a two-stage procedure. Arthrodesis failed in 3 (1.5 %) patients. Two with external fixation for failed hinge arthroplasties were left with uninfected nonunions, equivalent to a resection arthroplasty, and a third required an above-knee amputation for persistent MRSA infection [163]. Bierwagen et al. reported 90 attempted arthrodeses after failed revision for infected TKR in patients aged 20–88 years. Three methods were used: external fixation, compression nailing, and plate osteosynthesis, with the second regarded as superior. Patients appeared to mobilize earlier, with less pain, and have a better quality of life with this technique [164].
63.6.1 Intramedullary Fixation
Knee arthrodesis with intramedullary fixation has been reviewed in detail [165]. It probably offers the highest likelihood of union, but with the following limitations:
1.
Infection must be eradicated first or risk dissemination to the hip.
2.
Long straight nails cannot easily fuse in slight flexion or valgus.
3.
Limb shortening.
Recurrent infection rates with IM fixation range from 10 to 17 % according to Talmo et al. [165]. Bargiotas et al. reported 12 patients with infected TKRs who were fused with a long IM nail as part of a two-stage protocol: 10 of 12 succeeded [166]. They later published a description of their surgical technique using a long locked nail. They prepared the distal femur with a concave reamer (as for femoral head resurfacing) and the tibia with a conventional acetabular reamer [167]. Long nails may be difficult to remove if broken [168], enhancing the appeal of the short stainless steel [169] and short Huckstep nails [170].
McQueen et al. introduced an intramedullary compression device for knee arthrodesis and reported 12 patients, 10 of whom had suffered failed TKRs. All achieved union [171]. A subsequent report of 44 selected cases performed by 33 surgeons showed excellent results [146]. Independent users favored this device over external fixation, remembering however that infection may be more prevalent in cases treated with external fixation [172]. A detailed description of the technique was published recently [173], and this remains the preferred salvage option [174]. Compression fusion is not likely to be practical if inordinate bone has been lost.
Arthrodesis with noncompressive, modular or coupling nails, first introduced by Enneking and Shirley for tumor patients, facilitates surgery, by addressing problems of surgical access, sterilization of very long implants, and managing the wide range of tibial and femoral canal diameters [175]. A modular titanium rod, described by Arroyoa, Garvin, and Neff in 1997, was used in 21 patients, 5 of whom had failed TKRs and were fused successfully [176]. Subsequent reports confirm high fusion rates with modular nails [162, 177–179] but not without complications [180] and controversy [181].
63.6.2 External and Ilizarov Fixators
Conventional external fixators [182–190] seem to have been supplanted by Ilizarov frames. Oostenbroek published a series of 15 infected TKRs fused with an Ilizarov frame. Eight cases had been treated unsuccessfully with other fusion techniques first, yet they were able to achieve union in all but one, with the frames in place for an average of 28 weeks [191]. Manzotti et al. used the Ilizarov successfully in two difficult cases: one a nonunion after conventional external fixation for an infected TKR and the other a multiply-operated infected revision TKR where an arthrodesis with plate fixation had failed: both had been infected with Staph aureus [192].
Bone loss presents a particular challenge for fusion surgery. Manzotti et al. later reported 5 successes out of 6 cases with the Ilizarov [193] and eventually one case of fusion plus lengthening [194]. Tokizaki reported three cases of distraction arthrodesis, with an IM device and bone grafting, to preserve bone length [195]. Spina reported union in 13 of 17 infected TKRs: two patients suffered infected nonunions and two others abandoned treatment. Five patients in this cohort had undergone 6 revision arthroplasties [196]. David and Shtarker reported success in all 13 failed TKR treated with the Ilizarov frame [197]. Computer navigation has been reported to supplement the Ilizarov technique [198]. The Ilizarov spatial frame seems appropriate in complex cases, with the additional advantage of not disseminating infection to the hip joint.
63.6.3 Arthrodesis with Internal Extramedullary Fixation
Nichols et al. reported success with dual compression plates for 11 failed, infected TKRs [199]. Pritchett et al. reported “tension band plating” for knee arthrodesis, where 6 of 26 cases had prior failed TKR. They concluded this was a superior method to obtain union, but it is difficult to evaluate the extent of bone loss they encountered. Talmo and Burke advocated plate fixation in specified circumstances after TKR: with long bone deformity, significant bowing, and either ipsilateral hip arthroplasty or osteoarthritis, adding that it should be avoided in patients who require but cannot undergo soft tissue reconstruction and would accordingly have poor coverage of plates. A two-stage approach is required to eradicate infection first [144]. Plate osteosynthesis, not previously recommended for osteoporotic bone, may be feasible with modern locking plates. Plate fixation has not generally been popular, and perhaps because if infection is cleared and the soft tissues can tolerate double plating, reimplantation is generally preferred.
Pulsed electromagnetic fields appeared to aid arthrodesis union after failed TKR, but no further reports followed this preliminary study [200]. Minimal fixation with cannulated screws, described by Lim et al., might be ideal in conjunction with good bone stock, if prolonged cast immobilization is acceptable. Surgical dissection would be limited and infection less likely to disseminate [201]. Vascularized fibular rotatory flaps have been used for arthrodesis for tumor and failed arthroplasty [202]. Two cases have been reported of fusion with pedicled fibular flaps: one fixed with plate osteosynthesis and the other with cannulated screws, following a revision TKR that failed due to infection [203].
63.6.4 Intramedullary Nail Arthrodesis with Major Bone Loss
Early experience with arthrodesis for failed TKR attributed nonunions to bone loss [157]. Although some shortening is required with arthrodesis to accommodate swing phase, excessive bone loss is problematic and one that tumor surgeons have addressed with intercalary allografts [204]. Stiehl and Hanel described bulk allografts with combined intramedullary and plate fixation to avoid leg shortening with arthrodesis after failed arthroplasty [205]. Lee et al. described a “distraction arthrodesis,” with interposition of large amounts of iliac crest autograft and femoral head allograft, to restore leg length. Their paper clarifies the indications for arthrodesis (Table 63.3). Infection after resection was diagnosed strictly and treated with second debridement prior to reimplantation. Before distraction arthrodesis, clinical evidence of infection had disappeared, and inflammatory markers had normalized. Their surgical technique is straightforward: manual traction was applied, and a long Huckstep nail was used in five and a short one due to femoral bowing in three. All patients entered into a two-stage protocol, presumably with the goal of reimplantation. Union was reported in eight cases (Fig. 63.6) [206].
Table 63.3




Indications for distraction arthrodesis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








