17 The hip region
Disorders of the hip are common both in children and in adults. Prominent among childhood affections are developmental (congenital) dislocation of the hip and Perthes’ disease (osteochondritis) of the head of the femur. The hip is subject to all types of arthritis, but in adults osteoarthritis is overwhelmingly the most prominent affection.
SPECIAL POINTS IN THE INVESTIGATION OF HIP COMPLAINTS
History
Age incidence of hip disorders. Many of the important disorders of the hip occur in childhood, and often at a particular period of childhood. So true is this with some disorders that the age of the patient at the onset of symptoms affords some indication of the likely nature of the trouble, as shown in Table 17.1. (For ease of memorising, round figures have been given in the table but some latitude must be allowed.)
Table 17.1 Usual age incidence of common hip disorders at time of diagnosis
| Age at time of diagnosis (years) | Disease |
|---|---|
| 0–2 | Developmental (congenital) dislocation |
| 2–5 | Tuberculous arthritis; transient synovitis |
| 5–10 | Perthes’ disease; transient synovitis |
| 10–20 | Slipped upper femoral epiphysis |
| 20–50 | Osteoarthritis (secondary to previous injury or disease) |
| 50–100 | Osteoarthritis (primary) |
Exposure
For the proper examination of the hip the patient should be stripped except for a pelvic slip or underpants and, in women, a bra. The first part of the examination is conducted with the patient lying supine; afterwards the patient is examined standing and walking.
Steps in clinical examination
A suggested routine for clinical examination of the hip is summarised in Table 17.2.
Table 17.2 Routine clinical examination in suspected disorders of the hip
| 1. LOCAL EXAMINATION OF THE HIP REGION | |
| (Patient supine) | Examination for fixed deformity |
| Position of pelvis | Including Thomas’s manoeuvre for detection and measurement of fixed flexion deformity |
| Determine the lie of the pelvis and set it square with the limbs if possible | |
| Movements (active and passive) | |
| Inspection | Flexion |
| Bone contours and alignment | Abduction; abduction in flexion |
| Soft-tissue contours | Adduction |
| Colour and texture of skin | Medial (internal) rotation |
| Scars or sinuses | Lateral (external) rotation |
| Palpation | Power (tested against resistance of examiner) |
| Skin temperature | Estimate strength of each muscle group: |
| Bone contours | flexors, extensors, abductors, adductors, rotators |
| Soft-tissue contours | |
| Local tenderness | |
| Examination for abnormal mobility | |
| Measurement of limb length | Test for longitudinal (telescopic) movement |
| Real or true length: | Click test (in new-born) |
| Measure from anterior superior iliac spine to medial malleolus | (patient standing) |
| Examination for postural stability | |
| (angle between pelvis and limbs to be equal on each side) | Trendelenburg’s test |
| Gait | |
| ‘Apparent’ or false discrepancy: | |
| Measure from xiphisternum to medial malleolus. (Limbs to be parallel and in line with trunk) | |
| 2. EXAMINATION OF POTENTIAL EXTRINSIC SOURCES OF HIP SYMPTOMS | |
| This is important if a satisfactory explanation for the symptoms is not found on local examination. The investigation should include: | |
| 3. GENERAL EXAMINATION | |
| General survey of the other parts of the body. The local symptoms may be only one manifestation of a widespread or generalised disease | |
Setting the pelvis square
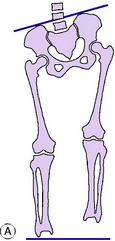
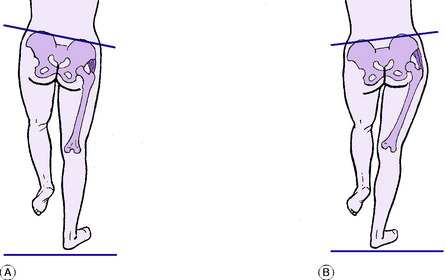
This is an important preliminary step. Determine from the position of the anterior superior iliac spines whether or not the pelvis is lying square with the limbs (Fig. 17.1). If it is not, an attempt is made to set it square. If this is impossible it means that there is incorrectable adduction or abduction at one or other hip (or, rarely, a severe and rigid curvature of the spine): in that event the fact that the pelvis is tilted should be noted and borne in mind during the subsequent steps of the examination.
Measuring the length of the limbs
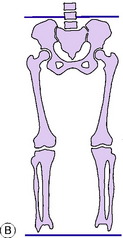
It is necessary to measure, first, the real or true length of each limb. Secondly, it is necessary to determine whether there is any ‘apparent’ or false discrepancy in the length of the limbs from fixed pelvic tilt (Fig. 17.2). Whereas it is always necessary to measure the true length, it is necessary to measure ‘apparent’ discrepancy only when there is an incorrectable tilt of the pelvis.
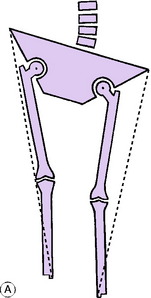
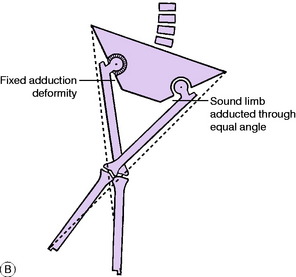
It should be noted that the anterior superior spine is well lateral to the axis of hip movement. This is of no consequence if the angle between limb and pelvis is the same on each side. But it will render the measurements fallacious if the angle between limb and pelvis is not the same on each side. This will be understood best by reference to Fig. 17.3A. It will be seen that abduction of a limb brings the medial malleolus nearer to the corresponding anterior superior spine, whereas adduction of the limb carries the medial malleolus away from the anterior superior spine. Thus if measurements are made while the patient lies with one hip adducted and the other abducted (a common posture in cases of hip disease) inaccurate readings will be obtained: the length will be exaggerated on the adducted side and underestimated on the abducted side.
The rule is, therefore, that to obtain an accurate comparison of their true length by surface measurement the two limbs must be placed in comparable positions relative to the pelvis. Thus if one limb is adducted and cannot be brought out to the neutral position, the other limb must be adducted through a corresponding angle by crossing it over the first limb before the measurements are taken (Fig. 17.3B). Similarly, if one hip is in fixed abduction the other must be abducted through the same angle before the measurements of true length are made.
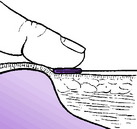
Fixing the tape measure at the anterior superior spine. A flat metal end (as found on the ordinary tailor’s measure) is essential. The metal end is placed immediately distal to the anterior superior spine and is pushed up against it. The thumb is then pressed firmly backwards against the bone and the tape end together (Fig. 17.4). This gives rigid fixation of the tape measure against the bone and minimises any error in measurement.
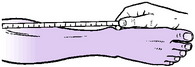
Taking the reading at the medial malleolus. The tip of the index finger is placed immediately distal to the medial malleolus and pushed up against it. The thumb nail is brought down against the tip of the index finger so that the tape measure is pinched between them (Fig. 17.5). The point of measurement is indicated by the thumb nail.
Determining the site of true shortening. If measurements reveal real shortening of a limb it is necessary to determine whether the shortening is above the trochanteric level (suggesting an affection in or near the hip), or below the trochanteric level (suggesting a disorder of the limb bones).
Shortening above the greater trochanter. Tests for shortening above the trochanteric level are: the measurement of Bryant’s triangle, Nelaton’s line, or Schoemaker’s line.
Measurement of ‘apparent’ discrepancy in limb length. ‘Apparent’ or false discrepancy in limb length is due entirely to incorrectable sideways tilting of the pelvis (Fig. 17.2A). The usual cause is a fixed adduction deformity at one hip, giving an appearance of shortening on that side, or a fixed abduction deformity, giving an appearance of lengthening. Exceptionally, fixed pelvic obliquity is caused by severe lumbar scoliosis.
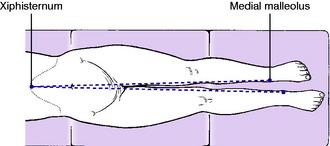
To measure apparent discrepancy the limbs must be placed parallel to one another and in line with the trunk. Measurement is made from any fixed point in the midline of the trunk (for example, the xiphisternum) to each medial malleolus (Fig. 17.6).
Examination for fixed deformity
Fixed adduction deformity. This is detected by judging the relationship between pelvis and limbs. It will already have been noted at an earlier stage of the examination. If fixed adduction is present the transverse axis of the pelvis (as indicated by a line joining the two anterior superior spines) cannot be set at right angles to the affected limb, but lies at an acute angle with it.
Fixed flexion deformity. This is determined by a manoeuvre known as Thomas’s test.
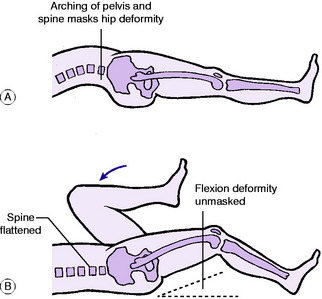
Principle of Thomas’s test. If there is a fixed flexion deformity at the hip the patient compensates for it, when lying on the back, by arching the spine and pelvis into exaggerated lordosis, as shown in Fig. 17.7A. This allows the affected limb to lie flat on the couch. To measure the angle of fixed flexion deformity it is necessary to correct the lumbo-pelvic lordosis. This is done by flexing the pelvis (and with it the lumbar spine) by means of the fully flexed sound limb (Fig. 17.7B).
Technique of the manoeuvre. One hand is placed behind the lumbar spine (between it and the couch) to assess the degree of lumbar lordosis. If there is no lordosis when the affected limb lies flat on the couch there can be no fixed flexion deformity and there is no need to proceed with the test. If there is excessive lordosis, as indicated by arching of the back (Fig. 17.7A), it is corrected in the following way: The sound hip is flexed to the limit of its range. The limb is then pushed further into flexion, thereby rotating the pelvis on a horizontal transverse axis until the arching of the spine is obliterated. During this manoeuvre the thigh of the disordered limb, if in fixed flexion, is automatically raised from the couch as the lumbar lordosis is reduced (Fig. 17.7B). The angle through which the thigh is raised from the couch is the angle of fixed flexion deformity.
Fixed rotation deformity. The most reliable index of the rotational position of the thigh is the patella, which normally points forwards when the hip is in the neutral position. If there is fixed lateral rotation or fixed medial rotation the limb cannot be rotated to the neutral position, with the patella directed forwards. The angle by which it falls short of the neutral when rotated as far as possible is the angle of fixed rotation deformity.
Movements
Flexion. The range of hip flexion is best demonstrated by flexing the hip and knee together; not by lifting the leg with the knee straight. Movement of the pelvis is best detected by grasping the crest of the ilium (Fig. 17.8). Only in this way is it possible to distinguish between true hip movement and the false flexion imparted by rotation of the pelvis. The normal range of true hip flexion is about 130 °, but it varies according to the build of the patient.
Abduction. The limb to be tested is supported by one hand while the other hand bridges the pelvis from anterior superior spine to anterior superior spine (Fig. 17.9). In this way true abduction at the hip can be differentiated from the false abduction that is imparted by tilting of the pelvis. The normal range of true abduction at the hip is 30 ° to 35 ° (more in children).
Abduction in flexion. This is often the first movement to suffer restriction in arthritis of the hip. The patient flexes his hips and knees by drawing the heels towards the buttocks. He then allows the knees to fall away from one another towards the couch (see Fig. 17.11B). The normal range is about 70 ° (90 ° in young children).
Examination for abnormal mobility
In infants it is important to examine for dislocation by the click tests of Ortolani and Barlow. These are described on page 344.
Examination for postural stability: the Trendelenburg test
Principle of the test. Normally, when one leg is raised from the ground the pelvis tilts upwards on that side, through the action of the hip abductors of the standing limb (Fig. 17.10A). (This automatic mechanism allows the lifted leg to clear the ground in walking.) If the abductors are inefficient they are unable to sustain the pelvis against the body weight and it tilts downwards instead of rising up on the side of the lifted leg (Fig. 17.10B).
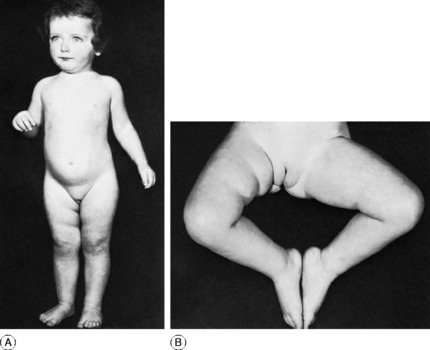
Fig. 17.11 Congenital dislocation of the right hip. A The right lower limb was slightly shorter than the left, as suggested here by the typical extra skin folds in the thigh. B shows the reduced range of abduction of the affected hip – another typical and important diagnostic feature.
Technique. Stand behind the patient. Instruct him first to stand upon the sound limb and to raise the other from the ground. Having thus got the idea of what he is required to do, he should now stand on the affected leg and lift the sound leg from the ground. By inspection, or by palpation with a hand upon the iliac crest, observe whether the pelvis rises or falls on the lifted side. Remember that the limb upon which the patient stands is the one under test. If the pelvis rises on the opposite side (normal) the test is negative (Fig. 17.10A). If it falls, the test is positive (Fig. 17.10B); in other words the abductor muscles are incapable of stabilising the pelvis upon the femur.
Causes of positive Trendelenburg test. There are three fundamental causes:
Gait
The patient’s ability to negotiate stairs must also be tested. A disability of the hip often precludes the normal rhythm of ascent and descent: on ascending, the foot of the sound leg is advanced first, and that of the affected side is then brought up to it. On descent, the affected leg is put down first and the sound leg is brought down to it.
Imaging
Computerised tomography (CT scanning) provides clear cross-sectional images of the pelvis or thigh and is useful in special circumstances. For instance, it can show accurately the orientation (degree of anteversion) of the acetabulum or of the neck of the femur. Or it may be used to outline bony or soft-tissue tumours in or about the pelvis or hip (see Fig. 2.3, p. 15).
DEVELOPMENTAL DYSPLASIA OF THE HIP
The term developmental dysplasia of the hip includes congenital dislocation of the hip, nearly always diagnosed either within a few days of birth or within the first two years of life; and dysplasia of the hip in adults, characterised by shallow configuration of the acetabulum, defective congruity between the femoral head and the socket, and a predisposition to osteoarthritis in middle or later life. Despite a trend towards re-naming congenital dislocation of the hip as developmental dysplasia of the hip, the title ‘congenital dislocation’ of the hip is so well established that it seems unnecessary to discard it. That title is therefore retained here for dislocation diagnosed in infancy.
CONGENITAL DISLOCATION OF THE HIP
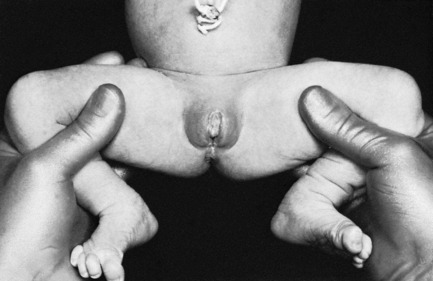
On examination at that time, the main features in unilateral cases are asymmetry (notably of the buttock folds), shortening of the affected limb (Fig. 17.11A), and restricted abduction in flexion. In bilateral cases the striking features are widening of the perineum and marked lumbar lordosis. The range of joint movements is full except for abduction in flexion, which is characteristically slightly restricted (Fig. 17.11B). In most cases the affected limb is abnormally mobile in its long axis (telescopic movement).
Imaging. Plain radiographs show three important features (Fig. 17.12):
These changes are not always shown conclusively before the age of 4 months.
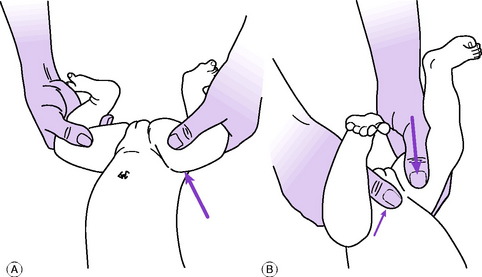
Diagnosis. In the new-born. Nearly always – though there are a few exceptions—dislocation or instability of the hip may be detected in the first few days of life by the diagnostic screening tests of Barlow or Ortolani (Fig. 17.13). In both tests the surgeon faces the child’s perineum and grasps the upper part of each thigh between fingers behind and thumb in front, the child’s knees being fully flexed and the hips flexed to a right angle (Fig. 17.14). While each thigh in turn is steadily abducted towards the couch the middle finger applies forward pressure behind the greater trochanter (Ortolani), and alternately the thumb, placed anteriorly, applies backward pressure while the thighs are adducted (Barlow). One of two abnormal states may be detected:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree