Chapter 9 T65 Standing: vertical trunk single leg T66 Standing: single foot lift test T67 Standing: spinal roll down test T72 Standing: single leg small knee bend test T73 Standing: one leg small knee bend + trunk rotation away test Lateral rotation/abduction control T75 Standing: single leg high knee lift test T76 Standing: one leg small knee bend + trunk rotation towards test T77 4 point: bent knee hip extension test The vast majority of hip pain referred to in the research and clinical literature primarily relates this pain to degenerative osteoarthritis (OA) of the hip. This pain usually originates from the groin with inconsistent patterns of radiation and referral of symptoms towards the trochanteric region and presents with varying degrees of movement restriction and loss of function. Simms (1999) states that hip pain is usually related to particular movements or sustained positions of the hip joint. Hip pain related to non-degenerative causes is largely under-reported in the literature. Hip pain from non-degenerative causes is often poorly diagnosed and frequently attributed to potential lumbar and sacroiliac referral mechanisms. A clinical reasoning process is required to differentiate groin, trochanteric and buttock pain arising from the hip as opposed to that arising from the lumbar spine or sacroiliac joint (Sahrmann 2002; Lee 2011). Sahrmann (2002) and Lee (2001) both describe patterns of altered muscle function (or ‘muscle imbalances’) to classify hip dysfunction. They argue that the presence of these patterns of altered muscle function, when linked to painful or dysfunctional hip movements, can be used to diagnose and differentiate hip-related pain from lumbar or sacroiliac sources. A study comparing manual therapy (manipulation and mobilisation) with exercise therapy in osteoarthritis of the hip showed the manual therapy program to be superior to the exercise therapy program (Hoeksma et al 2004). However, motor control issues were not specifically identified or addressed in this paper. Hardcastle & Nade (1985) state that one of the most consistent markers of hip dysfunction is the lack of lateral control of the hip and pelvis in single leg stance. Several studies have attempted to make links between hip joint pain and altered function of the gluteal muscles. The majority of these studies have focused on measuring weakness during strength tests. Strength deficits are commonly reported. Some studies have evaluated changes in muscle size and appearance with pain or altered muscle function. Arokoski et al (2002) showed that subjects with hip osteoarthritis (OA) had a decrease in abduction strength by as much as 31% compared to controls. The cross-sectional area (CSA) of the pelvic and thigh muscles, however, did not show significant differences between the two groups. Those with hip OA demonstrated a 13% decrease in the CSA of the gluteals and the adductors on the more severely affected hip as compared to the better hip. Interestingly, the decrease in CSA in the abductor and adductor muscles was not a direct indicator of muscle strength deficits. Robinson et al (2005) presented a series of eight case reports of subjects with hip pain. All cases presented with a decrease of CSA in the piriformis, gemelli inferior, obturator externus or a combination of one or more of these muscles. Grimaldi et al (2009) evaluated changes in gluteus maximus and tensor fasciae latae (TFL) muscle volumes in subjects with unilateral hip joint pathology. Twelve subjects with hip joint pain ranging from labral pathology to advanced OA were evaluated by magnetic resonance imaging (MRI), in order to achieve a volume measurement, and compared to 12 control subjects. The MRI evaluation of gluteus maximus identified two functionally differentiated compartments within gluteus maximus: an upper (superficial lateral) compartment (UGM) and a lower (deep medial) compartment (LGM). Their results demonstrated the LGM had a significant decrease in volume related to pain and OA while the TFL and UGM, which insert into the iliotibial band, both maintained muscle bulk in the presence of OA hip pain. Findings such as this suggest that assessment of gross strength deficits per se may not adequately identify hip dysfunction. Variations in the timing and sequencing of activation of various hip muscles have been reported by several authors. Many authors (Janda 1983; Long et al 1993; Sahrmann 2002) report changes in the neuromuscular coordination between TFL and gluteus medius (GMD). They demonstrate increased activity, earlier recruitment and loss of extensibility in TFL in some subjects. During a prone hip extension movement a delay in the activation of GMD or failure to maintain efficient holding tension in inner range has been reported (Janda 1983; Richardson & Sims 1991; Bullock-Saxton et al 1994; Sahrmann 2002; Lehman et al 2004). Abnormal control of femoral translation and femoral rotation has been linked to anterior hip pain and pathologies of the labrum and associated hip capsule and anterior muscles (Sahrmann 2002; Lee 2001; Shindle et al 2006; Lewis et al 2007). The authors postulate that tissue loading and pathology results from a variety of biomechanical mechanisms, which include mechanical impingement, rotational strain and instability. Lewis et al (2007) developed a biomechanical model that found that decreased force contributions from the gluteal muscles (during hip extension) and decreased iliopsoas force (during hip flexion) resulted in an increase in anterior hip loading. They also reported that the hip loading was greater if the hip was positioned in extension to initiate these movements. Sahrmann (2002) describes clinical tests to palpate for the presence of excessive or uncontrolled femoral head anterior glide during hip flexion and hip extension movements. Sahrmann (2002) postulates that the development of excessive hip medial rotation leads to abnormal loading on the anterior hip structures, which in turn results in hip pain and pathology. Levinger et al (2007) demonstrate excessive and uncontrolled hip medial rotation during a single leg squat. Lewis et al (2007) report that the hip demonstrates increased medial rotation if the iliopsoas force decreases and the TFL force increases, and that this ‘imbalance’ produces an excessive increase in anterior hip loading. The diagnosis of the site and direction of UCM at the hip can be identified in terms of the site (being hip) and the direction of medial rotation, lateral rotation, flexion, extension and forwards glide (Box 9.1). As with all UCM, the motor control deficit can present as uncontrolled translational movement (e.g. forwards glide) or uncontrolled range of functional movement (e.g. hip flexion) (Sahrmann 2002). The key principles for assessment and classification of UCM are described in Chapter 3. All dissociation tests are performed with the hip in a mid-range neutral training region. However, this may be closer to end range but not at end range (e.g. close to extension while attempting to prevent flexion). • In sagittal plane movements (flexion or extension), palpation of the trochanter during passive hip movement is used to identify the location of the neutral axis of hip motion. The ability to maintain the neutral axis and prevent excessive forwards glide of the trochanter during active unassisted flexion or extension is compared with the passive evaluation. • In axial plane movements (lateral rotation and abduction), palpation of the anterior prominence of the femoral head during passive movement with manual stabilisation is used to identify the location of the neutral axis of hip motion. The ability to maintain the neutral axis and prevent excessive forwards glide of the anterior prominence of the femoral head during active unassisted lateral rotation and abduction is compared with the passive evaluation. A global range-specific hip flexion UCM can be identified in motion testing in several ways: • Observe or palpate excessive or hypermobile range of hip flexion. During the test movement, the therapist relies on visual observation or manual palpation to identify if the subject cannot control (prevent or eliminate) additional hip flexion. The subject demonstrates an inability to prevent movement into further hip flexion when instructed to prevent flexion. • Observe or palpate that during a functional multi-joint movement into flexion, hip flexion dominates the initiation of the movement pattern. The subject demonstrates an inability to reverse this pattern. They cannot easily initiate the movement with thoracolumbar flexion or lower leg flexion when instructed to do so. • Place a long piece of adhesive strapping tape across the posterior hip (e.g. from the posterior superior iliac spine (PSIS) to the upper portion of the posterior thigh), with the hip positioned in an extension position relevant to the specific test. By skin tensioning from the lowermost attachment (below) to the uppermost attachment, if the subject cannot prevent or control hip flexion, the tape pulls off the skin when uncontrolled flexion motion is produced. A global range-specific hip extension UCM can be identified in motion testing in several ways: • Observe or palpate excessive or hypermobile range of hip extension. During the test movement, the therapist relies on visual observation or manual palpation to identify if the subject cannot control (prevent or eliminate) additional hip extension. The subject demonstrates an inability to prevent movement into further hip extension when instructed to prevent extension. • Observe or palpate that during a functional multi-joint movement into extension, hip extension dominates the initiation of the movement pattern. The subject demonstrates an inability to reverse this pattern. They cannot easily initiate the movement with thoracolumbar extension or lower leg extension when instructed to do so. • Place a long piece of adhesive strapping tape across the anterior hip (e.g. from the anterior superior iliac spine (ASIS) to the upper portion of the anterior thigh) with the hip positioned in a flexion position relevant to the specific test. By skin tensioning from the lowermost attachment (below) to the uppermost attachment, if the subject cannot prevent or control hip extension, the tape pulls off the skin when uncontrolled extension motion is produced. A global range-specific hip medial rotation UCM can be identified in motion testing in several ways: • Observe or palpate excessive or hypermobile range of hip medial rotation. During the test movement, the therapist relies on visual observation or manual palpation to identify if the subject cannot control (prevent or eliminate) additional hip medial rotation. The subject demonstrates an inability to prevent movement into further hip medial rotation when instructed to prevent rotation. • Observe or palpate that during a functional multi-joint movement into rotation, hip medial rotation dominates the initiation of the movement pattern. The subject demonstrates an inability to reverse this pattern. They cannot easily initiate the movement with thoracolumbar rotation or lower leg rotation when instructed to do so. • Place a long piece of adhesive strapping tape across the lateral hip (e.g. from the posterior iliac crest to the medial portion of the anterior thigh) with the hip positioned in a lateral rotation position relevant to the specific test. By skin tensioning from the lowermost attachment (below) to the uppermost attachment, if the subject cannot prevent or control hip medial rotation, the tape pulls off the skin when uncontrolled motion is produced. • Observe or palpate excessive or hypermobile range of hip lateral rotation or abduction. During the test movement, the therapist relies on visual observation or manual palpation to identify if the subject cannot control (prevent or eliminate) additional hip lateral rotation or abduction. The subject demonstrates an inability to prevent movement into further hip lateral rotation/abduction when instructed to prevent this movement. • Observe or palpate that during a functional multi-joint movement into rotation, hip lateral rotation or abduction dominates the initiation of the movement pattern. The subject demonstrates an inability to reverse this pattern. They cannot easily initiate the movement with thoracolumbar rotation or lower leg rotation when instructed to do so. • Place a long piece of adhesive strapping tape across the medial hip (e.g. from the inguinal ligament and anterior iliac crest to the lateral portion of the posterior thigh) with the hip positioned in a medial rotation and adduction position (relevant to the specific test). By skin tensioning from the lowermost attachment (below) to the uppermost attachment, if the subject cannot prevent or control hip lateral rotation and abduction, the tape pulls off the skin when uncontrolled motion is produced. • global hip lateral rotation/abduction – uncontrolled lateral rotation or abduction during active unilateral lower leg movement or thoracolumbar rotation dissociation tests • segmental hip forwards glide – uncontrolled segmental anterior translation of the femoral head during active hip lateral rotation/abduction or ‘turnout’ movements. 1. natural or ‘automatic’ forwards bending 2. natural rocking backwards on to hips in 4 point kneeling The subject is instructed to stand with the feet in a natural stance and bend forwards in a normal relaxed pattern. Ideally, there should be even flexion throughout the lumbar and thoracic regions with the hips flexing to approximately to 70°. The spinal flexion and hip flexion should occur concurrently. The fingertips should reach the floor without the need to bend the knees (Figure 9.1). • Thoracolumbar restriction of flexion: thoracic or lumbar flexion restriction may also contribute to compensatory increases in hip flexion range. This is confirmed with manual assessment of hip flexion range. • Gastrocnemius or talocrural joint restriction of ankle dorsiflexion: the ankle lacks normal range of dorsiflexion in standing forwards bending. The hip frequently may increase flexion to compensate for the lack of ankle mobility. Gastrocnemius extensibility can be tested passively and dynamically with manual muscle extensibility examination and restrictions of talocrural joint dorsiflexion can be confirmed with manual assessment of joint mobility. • Hip flexion: the hip may initiate the movement into flexion; contribute more to producing forward bending while the thoracolumbar contributions start later and contribute less. At the limit of forwards bending, excessive or hypermobile range of hip flexion may be observed. During the return to neutral the hip flexion persists and unrolls late. With the subject on hands and knees and the spine and pelvis in neutral alignment, place the knees hip width apart. The subject is instructed to rock backwards towards their heels. Monitor pelvic motion with one hand placed on the sacrum to identify the point of initiation of posterior pelvic tilt. This point identifies the limit of hip flexion range as the posterior hip structures are tensioned and pull the pelvis into posterior tilt. Ideally, the person should have the ability to dissociate the lumbar spine and pelvis from hip flexion as evidenced by 120° of hip flexion during backward rocking while preventing lumbar flexion or posterior pelvic tilt (Figure 9.2). After 120° hip flexion the pelvis should start to tilt posteriorly and the spine should start to flex as the pelvis moves towards the heels. • Thoracolumbar restriction of flexion: thoracic or lumbar flexion restriction may also contribute to compensatory increases in hip flexion range. Soleus extensibility can be tested passively and dynamically with manual muscle extensibility examination, and restrictions of talocrural joint dorsiflexion can be confirmed with manual assessent of joint mobility. • Hip flexion: the hip may initiate the movement into flexion; contribute more to producing rocking backwards while the thoracolumbar contributions start later and contribute less. Greater than 120° of hip flexion range is observed during backward rocking before any posterior pelvic tilt or lumbar flexion is produced. The person can almost sit back onto their heels using excessive hip flexion while maintaining a straight lumbar spine. The person stands upright with the feet hip width apart (heels approximately 10–15 cm apart) with the inside borders of the feet parallel (not turned out) and the 2nd metatarsal aligned along the ‘neutral line’ of weight transfer (a line that is 10° lateral to the sagittal plane). Perform a bilateral small knee bend (SKB) by flexing at the knees and dorsiflexing the ankles while keeping the heels on the floor. Hold the knee out over the foot to orientate the line of the femur out over the 2nd toe (on the ‘neutral line’) (Figure 9.3). The knees are to bend as far as the heels can stay on the floor and correct rotational alignment is maintained. Ideally, the trunk should stay vertical (as if sliding down a wall) and the knees flex so that a vertical plumb line dropped from the front of the knees should fall 3–8 cm past the longest toes, without any hip medial rotation or midfoot pronation (Figure 9.4). Body weight should stay equally distributed on each foot and there should be no lateral shift of the pelvis. • Hip flexion: the natural pattern of movement is that the hips initiate the movement and contribute more to producing the SKB while the ankle and knee contributions start later and contribute less. Observe that the trunk leans forwards into hip flexion. With a SKB on correct rotational alignment the knees do not move sufficiently past the toes. • Stand in neutral foot alignment with correct tibial rotational alignment (2nd metatarsal on the neutral line of weight transfer). • Perform a SKB (in weight bearing, flex the knees and dorsiflex the ankles while keeping both heels on the floor). • Control femoral rotational alignment (femurs of neutral line of weight transfer). • Knee bend as far as the heels can stay on the floor. • Observe the relative sagittal alignment of hip, knee and ankle in the natural pattern (without cueing and alignment correction). The long axis of the femur and the 2nd metatarsal are both aligned to the lower limb neutral line (a line 10° lateral to the sagittal plane) (Figure 9.4). • With a SKB on correct alignment the knees do not move sufficiently past the toes. The knee alignment is less than 3 cm past the toe. It is common for the knees to only move as far as the metatarsal heads. To maintain functional ability to bend down, hip flexion significantly increases as uncontrolled compensation. The subject cannot correct the pattern or finds it very difficult to correct. Many do not realise that the hips are ‘hanging out the back’ and often believe that the trunk is vertical when it is obviously inclined forwards. • With a SKB on correct alignment the knees do not move sufficiently past the toes. The knee alignment is greater than 8 cm past the toes. Hip flexion significantly decreases. The subject cannot correct the pattern or finds it very difficult to correct. The trunk is often inclined backwards to maintain balance. Sagittal alignment can be classified into one of three groups: 2. Hip flexion dysfunction (Figure 9.5): a. plumb line dropped from the front of the knee falls less than 3 cm in front of the toes b. relatively restricted knee flexion and ankle dorsiflexion c. relatively excessive or uncontrolled hip flexion d. the trunk leans forwards from vertical (more hip flexion than ideal) to keep the centre of mass balanced over the midfoot. 3. Lower leg flexion dysfunction (Figure 9.6): a. plumb line dropped from the front of the knee falls more than 8 cm in front of the toes b. relatively restricted hip flexion c. relatively excessive or uncontrolled hip flexion and ankle dorsiflexion d. the trunk leans backwards from vertical (more hip extension than ideal) to keep the centre of mass balanced over the midfoot. The person stands with the feet hip width apart (heels approximately 10–15 cm apart) with the inside borders of the feet parallel (not turned out). The upper body should be vertical and the weight balanced over the midfoot. The person is asked to shift full weight onto one foot and lift the other foot just clear of the floor. In this position, the person is standing on one leg with the 2nd metatarsal aligned along the ‘neutral line’ of weight transfer (a line that is 10° lateral to the sagittal plane). The pelvis should be level and the trunk upright (vertical). There should be no lateral deviation, tilt or rotation of the trunk or pelvis. The head, sternum and pubic symphysis should be vertically aligned above the inside edge of the stance foot with the shoulders level in an upright posture (Figure 9.7). From this start position, the person then performs a single leg small knee bend (SKB) by flexing at the knee and dorsiflexing the ankle while keeping the heel on the floor. The body weight should be on the heel, not the ball, of the foot and the trunk kept vertical (as if sliding the back down a wall). Do not lean the trunk forwards. Hold the knee out over the foot to orientate the line of the femur out over the 2nd toe (on the ‘neutral line’) (Figures 9.8 and 9.9). The trunk should stay vertical (as if sliding down a wall) and the knee should move past the toes. If a plumb line were dropped from the front of the knee it should fall between 3 and 8 cm in front of the longest toe. Ideally, there should be approximately 3–8 cm of independent SKB past the toes, without any forwards lean of the trunk or posterior shift of the hips and pelvis into increased hip flexion. Initial retraining is best started with the trunk supported against a wall. The person stands with the back against a wall and the feet hip width apart (heels approximately 10–15 cm apart) with the inside borders of the feet parallel. The person is asked to stand upright with the upper body vertical and the weight balanced over the midfoot. The heels should be approximately 5–10 cm from the wall. The pelvis should be level and the trunk upright (vertical against the wall) (Figure 9.10). If control is poor, perform a SKB by sliding the trunk down the wall to a As control improves, the person is instructed to shift their weight to stand on one leg and perform a single leg SKB to the T65.3 Feedback tools to monitor retraining The person should stand upright with the upper body vertical, the weight balanced over the feet and the pelvis centred over the heels (Figure 9.12). The person is instructed to shift full weight onto one leg and, keeping the shoulders and pelvis level, slowly lift the other foot off the floor to 90° hip flexion (Figure 9.13). There should be no increase in hip flexion on the weight bearing stance leg. Movement of the buttocks backwards by more than 2 cm indicates uncontrolled hip flexion. Initial retraining is best started with the trunk supported against a wall. The person stands with the back against a wall, the feet hip width apart and the weight balanced over the feet. The heels should be approximately 5–10 cm from the wall. The pelvis should be level and the trunk upright (vertical against the wall). The person should be instructed to perform a SKB by sliding the trunk down the wall to a The person should self-monitor the hip and trunk alignment and control hip flexion UCM with a variety of feedback options (T66.3). There should be no provocation of any symptoms within the range that the hip flexion UCM can be controlled. T66.3 Feedback tools to monitor retraining The person stands with pelvis and upper back supported against the wall, the feet at least shoulder width apart and the knees slightly flexed (hip flexors unloaded and wide base of support). The heels are positioned about 15–20 cm in front of the wall (Figure 9.15). Then, they are instructed to actively lower the sternum towards the pelvis by flexing the thoracic spine while rolling the pelvis backwards (posterior pelvic tilt) to flatten the back onto the wall. The person should monitor that they can feel the sacrum flattened against the wall. They should then continue to flex the spine by slowly letting the head and chest drop towards the pelvis. The spine should unroll into flexion, but the pelvis and sacrum should stay firmly flattened against the wall. The person should have the ability to dissociate the hip flexion from spinal flexion as evidenced by preventing the pelvis rolling off the wall, while rolling the spine down from the wall into spinal flexion. Ideally, the person should be able to roll down into full spinal flexion and maintain the pelvis posteriorly tilted against the wall (Figure 9.16). There should be no forwards pelvic tilt off the wall (i.e. hip flexion) as the spine rolls forwards off the wall into spinal flexion. The spinal flexion must be independent of any hip flexion or movement of the pelvis. Note any uncontrolled hip flexion under spinal flexion load. This test should be performed without any feedback (self-palpation, vision, etc.) or cueing for correction. The therapist should use visual observation of the femur and pelvis to determine whether the control of hip flexion is adequate. Retraining is best started with the trunk supported against a wall, the feet at least shoulder width apart and the knees slightly flexed (hip flexors unloaded and wide base of support). If control is poor, the heels are initially positioned about 30–40 cm in front of the wall. Then they are instructed to actively lower the sternum towards the pelvis by flexing the thoracic spine while rolling the pelvis backwards (posterior pelvic tilt) to flatten the back onto the wall. The person should monitor that they can feel the sacrum flattened against the wall. Only roll the spine down off the wall through partial flexion range (Figure 9.17). Ensure that the sacrum and upper pelvis can stay firmly in contact with the wall and not roll forwards into increased hip flexion. As control improves, the person is instructed to shift their feet closer to the wall and to increase the range of spinal roll down. At the point in range that the pelvis starts to roll forwards into hip flexion the movement should stop and return to the start position. The person should self-monitor the hip and pelvis alignment and control hip flexion UCM with a variety of feedback options (T67.3). There should be no provocation of any symptoms within the range that the hip flexion UCM can be controlled. T67.3 Feedback tools to monitor retraining The person lies on one side with uppermost (top) leg extended in line with the trunk and the other (bottom leg) hip flexed to 45° and the knees flexed to 90° (Figure 9.18). The pelvis should be positioned in neutral rotation. The person is instructed to maintain the neutral pelvis position and turn the uppermost foot outwards (hip lateral rotation). Then they should slowly lift the uppermost leg vertically up and out to the side while keeping the leg and foot turned out into lateral rotation. Ideally, the top leg should be able to maintain the hip extension and turnout and lift into at least 35° (above horizontal) of hip abduction and lateral rotation (Figure 9.19) and return, without associated loss of neutral extension into any flexion of the hip. T68.1 Assessment and rating of low threshold recruitment efficiency of the Single Leg Abduction Test The unilateral hip abduction must be independent of any hip flexion. The person should self-monitor the hip alignment and control flexion UCM with a variety of feedback options (T68.3). There should be no provocation of any symptoms within the range that the rotation UCM can be controlled. T68.3 Feedback tools to monitor retraining The person sits on the end of a plinth or table, holds onto one knee and rolls backwards onto their back keeping both legs flexed. With the lower thoracic spine and sacrum flat on the table, the subject pulls one knee up towards the chest until the lumbar spine flattens onto the table, but not so far that the sacrum rolls off the table into lumbopelvic flexion. The subject uses both hands holding one knee to support this flat back position. The therapist then passively lowers the test leg down towards the table (hip extension), keeping the hip adducted to the midline and knee flexed to 90° while monitoring maintenance of the lumbopelvic position (Figures 9.20 and 9.21).
The hip
 squat test
squat test
Introduction
Changes in muscle function around the hip
UCM at the hip
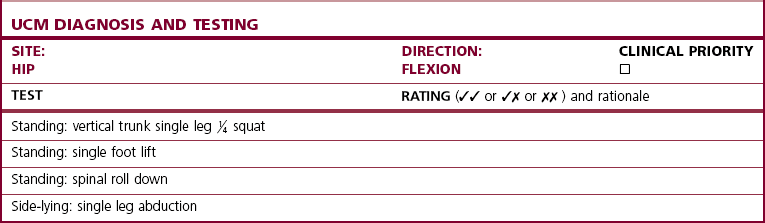
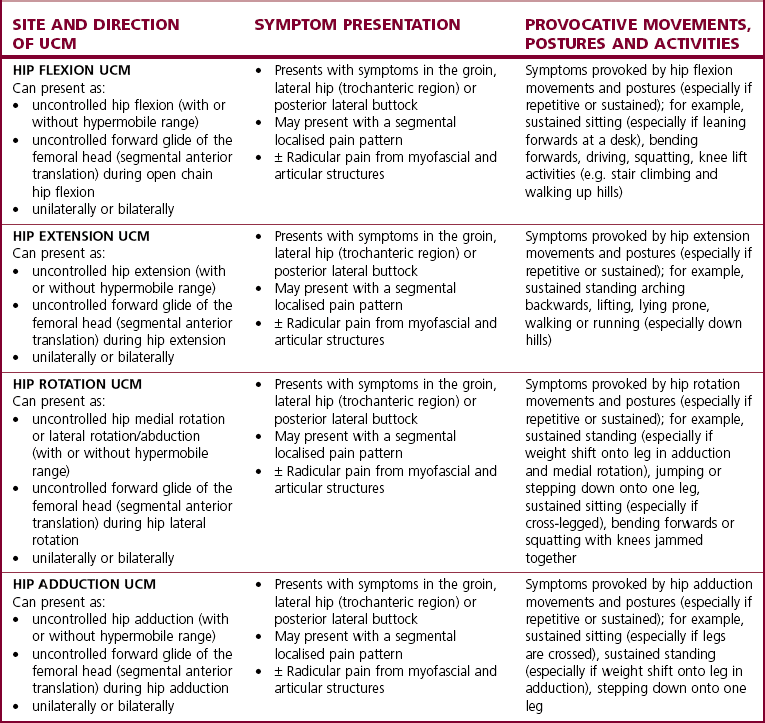
Diagnosis of the site and direction of ucm in the hip
Identifying site and direction of UCM at the hip
Segmental translatatory and global range-specific uncontrolled motion
Segmental translatatory UCM
Global range-specific UCM
Examples
Hip lateral rotation/abduction UCM
Observation and analysis of sagittal hip flexion and bending
Description of ideal pattern of forwards bending
Movement faults associated with hip UCM in forwards bending
Relative stiffness (restrictions)
Relative flexibility (potential UCM)
Description of ideal pattern of backward rocking (hands and knees 4 point kneeling)
Movement faults associated with hip UCM in backward rocking
Relative stiffness (restrictions)
Relative flexibility (potential UCM)
Description of ideal pattern of small knee bend (SKB)
Sagittal movement faults associated with hip UCM in the SKB
Relative flexibility (potential UCM)
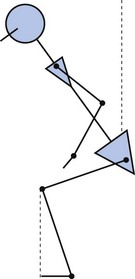
Hip and lower quadrant sagittal alignment evaluation
Ideal sagittal alignment
Dysfunction
Hip flexion control tests and flexion control rehabilitation
Hip flexion control tests
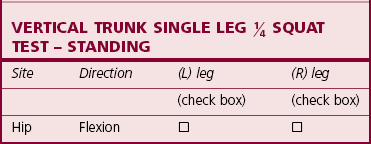
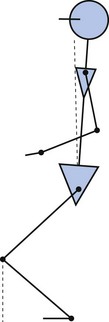
T65 Standing: vertical trunk single leg
 squat test(tests for hip flexion UCM)
squat test(tests for hip flexion UCM)
Test procedure
Rating and diagnosis of hip flexion UCM
Correction
 squat position. The person should keep the back on the wall and weight balanced equally on both feet. Only slide down the wall as far as the trunk can stay on the wall and do not lean forwards into increased hip flexion.
squat position. The person should keep the back on the wall and weight balanced equally on both feet. Only slide down the wall as far as the trunk can stay on the wall and do not lean forwards into increased hip flexion.
 squat position. Keep the trunk vertical on the wall and the knee should move past the toes. Only slide down the wall as far as the trunk can stay on the wall and do not lean forwards into increased hip flexion (Figure 9.11). At the point in range that the trunk starts to lean forwards into hip flexion or the knee moves medially to allow compensation at the foot and ankle, the movement should stop and return to the start position. The person should self-monitor the hip and trunk alignment and control hip flexion UCM with a variety of feedback options (T65.3). There should be no provocation of any symptoms within the range that the hip flexion UCM can be controlled.
squat position. Keep the trunk vertical on the wall and the knee should move past the toes. Only slide down the wall as far as the trunk can stay on the wall and do not lean forwards into increased hip flexion (Figure 9.11). At the point in range that the trunk starts to lean forwards into hip flexion or the knee moves medially to allow compensation at the foot and ankle, the movement should stop and return to the start position. The person should self-monitor the hip and trunk alignment and control hip flexion UCM with a variety of feedback options (T65.3). There should be no provocation of any symptoms within the range that the hip flexion UCM can be controlled.
FEEDBACK TOOL
PROCESS
Self-palpation
Palpation monitoring of joint position
Visual observation
Observe in a mirror or directly watch the movement
Adhesive tape
Skin tension for tactile feedback
Cueing and verbal correction
Listen to feedback from another observer
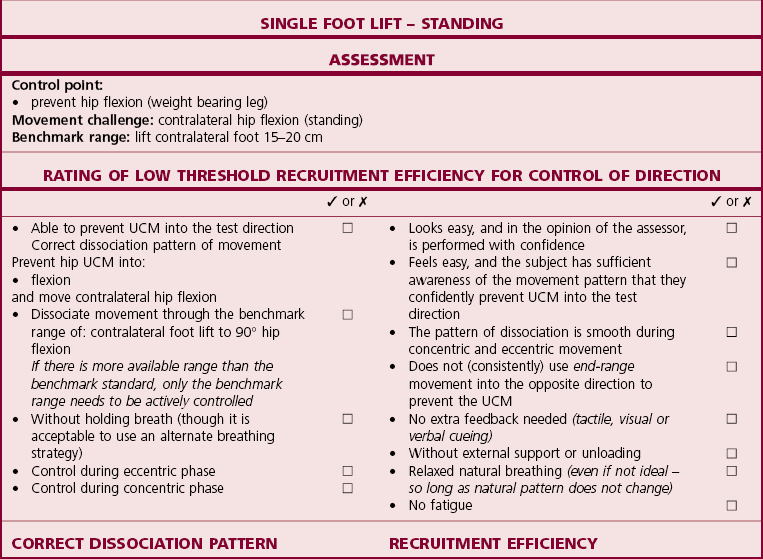
T66 Standing: single foot lift test(tests for hip flexion UCM)
Test procedure
Rating and diagnosis of hip flexion UCM
Correction
 squat position with weight balanced equally on both feet. This is followed by a shift of full weight onto one leg, allowing the pelvis and shoulders to move laterally to keep body weight centred over the weight bearing foot. The shoulders and pelvis should stay level. The person should then slowly lift the other foot 15–20 cm off the floor (as if stepping up onto a step) (Figure 9.14). There should be no increase in hip flexion on the weight bearing stance leg. Only lift the foot as far as the trunk can stay on the wall and do not lean forwards into increased hip flexion.
squat position with weight balanced equally on both feet. This is followed by a shift of full weight onto one leg, allowing the pelvis and shoulders to move laterally to keep body weight centred over the weight bearing foot. The shoulders and pelvis should stay level. The person should then slowly lift the other foot 15–20 cm off the floor (as if stepping up onto a step) (Figure 9.14). There should be no increase in hip flexion on the weight bearing stance leg. Only lift the foot as far as the trunk can stay on the wall and do not lean forwards into increased hip flexion.
FEEDBACK TOOL
PROCESS
Self-palpation
Palpation monitoring of joint position
Visual observation
Observe in a mirror or directly watch the movement
Adhesive tape
Skin tension for tactile feedback
Cueing and verbal correction
Listen to feedback from another observer
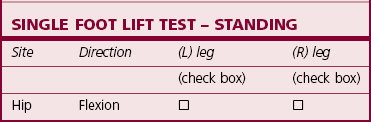
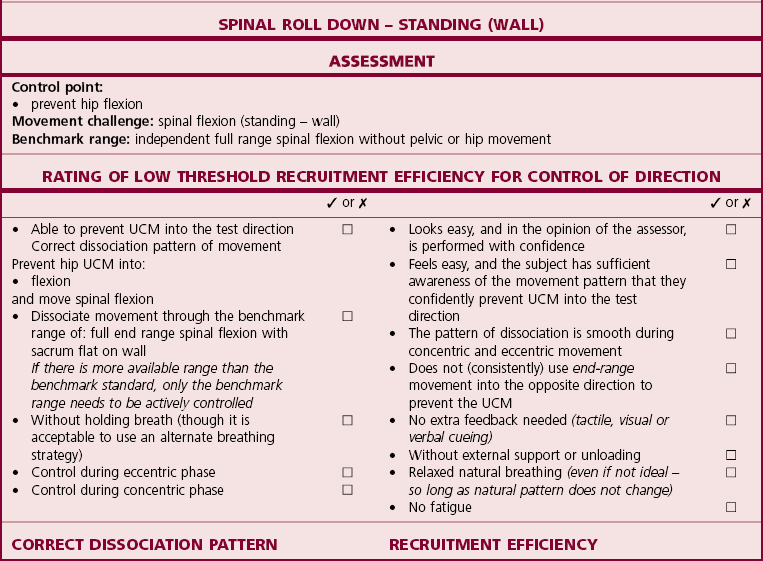
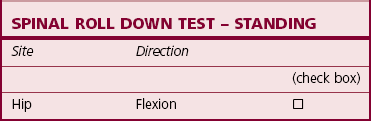
T67 Standing: spinal roll down test(tests for hip flexion UCM)
Test procedure
Rating and diagnosis of hip flexion UCM
Correction
FEEDBACK TOOL
PROCESS
Self-palpation
Palpation monitoring of joint position
Visual observation
Observe in a mirror or directly watch the movement
Adhesive tape
Skin tension for tactile feedback
Cueing and verbal correction
Listen to feedback from another observer
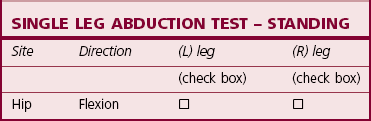
T68 Side-lying: single leg abduction test(tests for hip flexion UCM)
Test procedure
Rating and diagnosis of hip flexion UCM
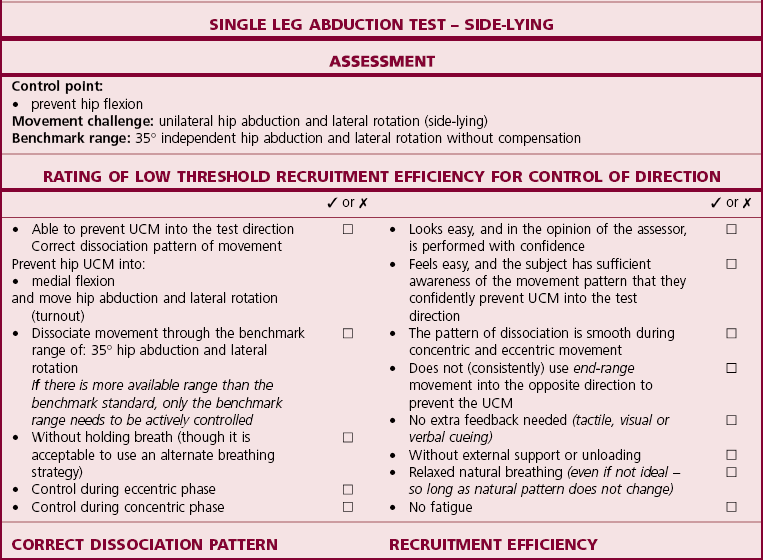
Correction
FEEDBACK TOOL
PROCESS
Self-palpation
Palpation monitoring of joint position
Visual observation
Observe in a mirror or directly watch the movement
Adhesive tape
Skin tension for tactile feedback
Hip extension control
Movement faults associated with hip extension
Modified Thomas test
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







 squat – small knee bend (SKB) by flexing the knee and dorsiflexing the ankle while in single leg standing.
squat – small knee bend (SKB) by flexing the knee and dorsiflexing the ankle while in single leg standing.
 squat test
squat test
 squat test side view
squat test side view
 squat test front view
squat test front view squat test, the hip demonstrates UCM into flexion (the trunk leans forwards and the hips move backwards into excessive hip flexion) before the knee reaches 3–8 cm past the toes. Under weight bearing knee flexion and ankle dorsiflexion, the hip has UCM into flexion relative to the knee and ankle. Hip flexion control is poor if the subject is unable to prevent or resist the excessive hip flexion.
squat test, the hip demonstrates UCM into flexion (the trunk leans forwards and the hips move backwards into excessive hip flexion) before the knee reaches 3–8 cm past the toes. Under weight bearing knee flexion and ankle dorsiflexion, the hip has UCM into flexion relative to the knee and ankle. Hip flexion control is poor if the subject is unable to prevent or resist the excessive hip flexion. Squat Test
Squat Test
 Squat Test
Squat Test