9 The hip
CHAPTER CONTENTS
Introduction
The hip joint is a multiaxial ball-and-socket, synovial joint that connects the head of the femur and the pelvic acetabulum. The head of the femur forms approximately two-thirds of a sphere and is covered with hyaline cartilage (Nicholls 2004). Twenty-two muscles cross the hip in order to stabilize the joint and move the femur during locomotion. It is has evolved to operate under loads exceeding three times the weight of the body, and is controlled by muscles of enormous power and extraordinary accurate coordination (Strange 1965). Any excess or unstable load may damage both soft tissue and joint structures, depending on the position of the joint at the time (Sims 1999). Many problems of the hip complex show movement dysfunctions of the joint, in combination with the lumbar spine, sacroiliac joint, neurodynamic structures, and muscular systems (Hengeveld & Banks 2005), all of which need accurate assessment before appropriate and effective interventions are chosen.
Soft tissue injuries
The hip is an integral component in load transference during upper and lower limb performance, with approximately 30% of hip pain in young adults remaining without clear diagnosis. Controversial diagnoses such as acetabular tear, femoro-acetabular impingement syndrome, instability, and osteoarthrosis (OA) are referred to (Nicholls 2004). In sport, the hip joint has been attributed to contributing between 0.5 and 14% of athletic injuries (Reid 1988; van Mechelen et al 1992) and adductor muscle-related groin pain is a common presentation in the athlete. Hölmich (2007) reviewed 207 cases of groin pain in the sporting population; 18% of all cases occurred in runners. From a clinical standpoint, sports-related groin pain can be classified into four clinical subgroups (Hölmich 2007):
High-velocity eccentric muscle contractions may injure muscles and tendons, or damage may be done by oblique, explosive forces with sudden movement bursts (Sharma & Maffulli 2005). The potential for certain muscles to be injured is greater for some than others, multijoint muscles being at greater risk because of their potential stretch over two joints. An accurate diagnosis and an assessment of the presenting muscle strain will rely on:
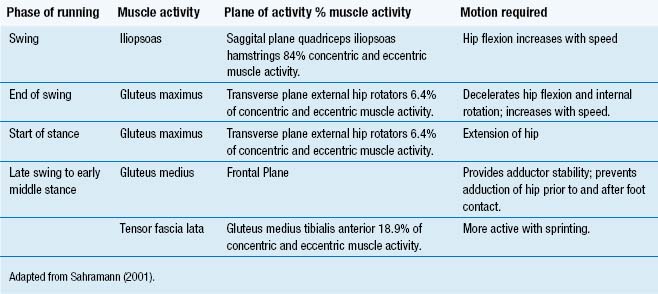
The goals of therapeutic intervention are to assist new muscle fibre growth and muscle fibre alignment, and reduce adhesion formation (Niemuth 2007). Numerous studies have documented the role of the hip muscles during running using electromyography (EMG) analysis to describe muscle activity in the swing and stance phases of running (Knuesel et al 2005; Sahraman 2001) (Table 9.1).
A common source of pain in runners is iliotibial band syndrome (ITBS), which is caused by repetitive friction of the iliotibial band sliding across the lateral femoral condyle. Fredericson et al (2000) hypothesized that weakness of the gluteus medius muscle causes overfiring and tightness of the tensor fascia lata (TFL) and ITBS, resulting in significant weakness of the hip abductors of the injured leg in injured runners.
In the acute stages of injury, gentle concentric strengthening activity is preferred, and as recovery is achieved, eccentric strengthening is particularly effective in promoting new collagen, reversing chronic degenerative tendon changes (LaStayo et al 2003), and promoting increased circulation for enhanced tenocyte and myocyte activity (Khan 1999).
Rehabilitation of proprioception is essential to avoid re-injury and return the patient to full function, especially the athlete. Repeated movements and sustained postures alter tissues that control the characteristics of movement, causing movement impairment (Sahramann 2001). Two main categories of movement impairment syndromes have been described: femoral and hip syndromes.
Hip syndromes
Detailed examination in order to identify and rectify movement impairment syndromes reveals a number of positive findings necessary for accurate confirmation of the diagnosis. A diagnosis of movement impairment using a variety of tests will identify the movement direction that must be corrected; these include:
The growth in the number of individuals participating in organized sport has contributed to an increase in the prevalence of hip-related injuries. Rehabilitation of the injured athlete requires knowledge of the physical and psychological demands on the patient, made by the sport and his or her expectation (Konin & Nofsinger 2007). Capsular and ligamentous injuries are not as commonly seen as musculotendinous injuries, but may arise from trauma and overuse, requiring arthroscopic diagnosis (Baber et al 1999). Amongst the acute problems encountered are:
Stress fractures develop as a result of the weakening and subsequent failure of the bone. With regard to the hip, individuals who progressively increase the duration of repetitive impact loading to the lower limb are most at risk to injury (Kahan et al 1994). Korpelainen et al (2001) found that those who were at highest risk were individuals with high longitudinal arches; leg length inequalities; excessive forefoot varus; and menstrual irregularities.
Diagnosis involves careful examination of all capsular movement patterns. Currently trial periods of non-weight-bearing for up to 3 months are advocated for patients with acute intra-articular dysfunction (Fitzgerald 1995; Ikeda et al 1988). In the acute stage the aim is to reduce weight bearing, relieve pain and inflammation, maintain range of movement, and maintain aerobic fitness. Overactivity in any of the hip muscles would increase compression forces on the joint. Both TFL and ITB overactivity demonstrate increased stress distributions in the cartilage of the superior part of the joint, which may lead to degeneration (Kummer 1993). The piriformis and obturator externus muscles may provide forces capable of producing posterior joint wear, whilst iliopsoas and rectus femoris muscles which have direct connections with the anterior capsule of the hip may demonstrate anterior joint wear (Sims 1999).
Muscle weakness or shortening as a result of an active trigger point (TrPt) in the gluteus medius may affect the hip abductor vector, causing a Trendelenberg gait, whilst fatigue may bring about a change in the muscular synergies, leading to adverse handling of repetitive impact loads (Mizrahi et al 1997). Therefore it is important to identify any musculoskeletal dysfunction and modulate pain in order to facilitate rehabilitation, and prevent further abnormal forces contributing to the more extensive pain of OA or joint changes later in life.
Osteoarthrosis
Osteoarthrosis is the most common reason for total hip and total knee replacement among adults aged over 30 years, and symptomatic hip OA occurs in approximately 3% of the UK population (Felson & Zhang 1998). Mechanical factors are of importance in the aetiology of OA; there is increasing evidence that an abnormal labrum is implicated in the early onset of OA (Ferguson et al 2003). In a normal hip, the capsule has no limiting effect other than at the end range positions; however, it has been argued that a person with capsular restriction, in attempting to walk normally, increases hip joint loads by stretching the tight capsule (Crowninshield et al 1978). Therefore, the hip is subjected to dynamic loads on impact as well as dynamic forces of equilibrium in single-leg stance; alterations in one component may affect another.
There has been limited research into the effectiveness of physiotherapy for OA hip, but in recent years, there have been an increasing number of randomized controlled trials (RCTs) evaluating the effect of exercise therapy (Hoeksma et al 2004; Tak et al 2005; van Baar et al 1998), manual therapy (Hoeksma et al 2004), acupuncture (Stener-Victorin et al 2004), and self-management (Heuts et al 2005). The effects of long-term exercise have yet to be demonstrated (Tak et al 2005; van Baar et al 1998).
Hoeksma et al (2004) focused on specific manipulations and mobilization of the joint, as well as exercise therapy involving active exercises to improve muscle function and joint motion. The treatment period was 5 weeks (nine sessions). The primary outcome was general perceived improvement (GPI) after treatment; secondary outcomes included reduced pain, and increased hip function, walking speed, range of movement (ROM), and quality of life. No major differences were found in baseline characteristics between the study groups, with 81% improvement in the manual therapy group and 50% in the exercise group. Patients in the manual therapy group had significantly better outcomes on pain, stiffness, hip function, and ROM, indicating that the effects of manual therapy, endured after 29 weeks, and that it was superior to the exercise therapy programme in patients with OA of the hip. Manual therapy techniques such as joint mobilizations, stretching, and joint traction/distraction appear to offer improvements in quality of life, function, and walking tolerance.
The European League against Rheumatism (EULAR) and the UK-based, multidisciplinary MOVE consensus group have developed recommendations for the management of OA hip based on the best available scientific evidence (Roddy et al 2004; Zhang et al 2005). The consensus is that strengthening, aerobic, and proprioceptive exercises are recommended, but the recommendations identify the need to increase research into the most effective exercise programme for OA hip with reference to compliance, effectiveness on land versus water, and individual versus group exercise (Roddy et al 2004; Zhang et al 2005).
In a survey of current practice for the management of OA hip in Republic of Ireland, French (2007) found limited evidence for a number of physiotherapy interventions, recommending that the role of education and self-management should be investigated further. Despite manual therapy being virtually unresearched, it was used by 96% of respondents in this survey.
Puett and Griffin (1994) reviewed 15 controlled trials on non-medicinal and non-invasive therapies for hip and knee OA, and concluded that exercises reduced pain and improved function, but the optimal exercise regime has not been determined.
Active and passive ROM has been considered an important part of rehabilitation for patients with OA as a means of regaining joint mobility and function (Biloxi 1998; Prentice 1992). Deyle et al (2000) evaluated the effectiveness of manual therapy and exercise therapy in OA knee. The treatment involved eight clinical visits, which produced a 52% improvement in function, stiffness, and pain, as measured by the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and a 12% improvement in walk test scores. Falconer et al (1992) found improvements in motion (11%), pain (33%), and gait speed (11%) over 4–6 weeks after 12 sessions of exercise combined with manual therapy for patients with clinically diagnosed OA knee.
Proprioceptive deficits contribute to functional instability, which could ultimately lead to further microtrauma and re-injury (Lephart et al 1997). Thus, incorporating a proprioceptive element into a physical therapy programme is suggested for joint disorders. Sensorimotor training to promote proprioceptive acuity and muscle contraction for patients with lower limb OA has been advocated since 1990 particularly for the re-education of the proprioceptors (Sharma et al 1997; Vad et al 2002). A therapeutic exercise programme incorporating sensory input to facilitate dynamic joint stabilization may retrain altered afferent pathways to enhance the proprioception of joint movement and improve a patient’s function. However, until now, there has been no standard training protocol available. Closed-chain exercise has been shown to give a better result with respect to facilitating proprioceptors than open-chain exercise (Beard et al 1994; Fitzgerald 1997). The exercises should be performed in various positions throughout the full ROM since the different afferent responses have been observed in different joint positions (Lephart et al 1997).
Acupuncture intervention
Treatment for OA is largely symptomatic, including analgesics, non- steroidal anti-inflammatory drugs (NSAIDs), glucosamine, topical analgesics such as capsaicin cream, and exercise, behavioural interventions, and surgical treatment (Felson et al 2000). No drug treatment is without risks and adverse effects; thus, non-pharmacological interventions are attractive.
Kwon et al (2006) conducted a systematic review and meta-analysis of acupuncture for peripheral joint OA, suggesting on the basis of best-evidence synthesis that the data evidence for manual acupuncture could be classified as fairly strong. Manual acupuncture appeared to reduce pain compared to waiting list controls and sham acupuncture, thus suggesting analgesic effects beyond a placebo response. Electroacupuncture (EA) was found to be superior to NSAID on the visual analogue scale (VAS) and WOMAC outcomes.
Stener-Victorin et al (2004) evaluated 45 patients, aged between 42 and 86 years who had radiographic changes consistent with OA of the hip. Those with pain related to motion load and ache were selected. The subjects were randomly allocated to EA, hydrotherapy, both in combination with patient education, or patient education alone. The outcome measures were the Disability Rating Index, the Global Self Rating, and the VAS. Assessments were taken before the intervention and immediately after the last treatment, and later, at 1, 3, and 6 months. Electroacupuncture and hydrotherapy, both in combination with patient education, induce long-lasting effects, as shown by reduced pain and ache, and by increased functional activity and quality of life, as demonstrated by differences in pre- and post-treatment assessments. Pain related to motion and pain on load was reduced up to 3 months after the last treatment in the hydrotherapy group and up to 6 months in the EA group. Ache during the day was significantly improved in both the EA and hydrotherapy groups up to 3 months after the last treatment. Ache during the night was reduced in the hydrotherapy and EA groups up to 3 and 6 months after the last treatment, respectively. Disability in functional activities was improved in the EA and hydrotherapy groups up to 6 months after the last treatment. Quality of life was also improved in EA and hydrotherapy groups up to 3 months after the last treatment. There were no changes in the education group alone. In conclusion, EA and hydrotherapy, both in combination with patient education, induce long-lasting effects, reduced pain and increased functional activity and quality of life, as demonstrated by differences in the pre- and post-treatment assessments.
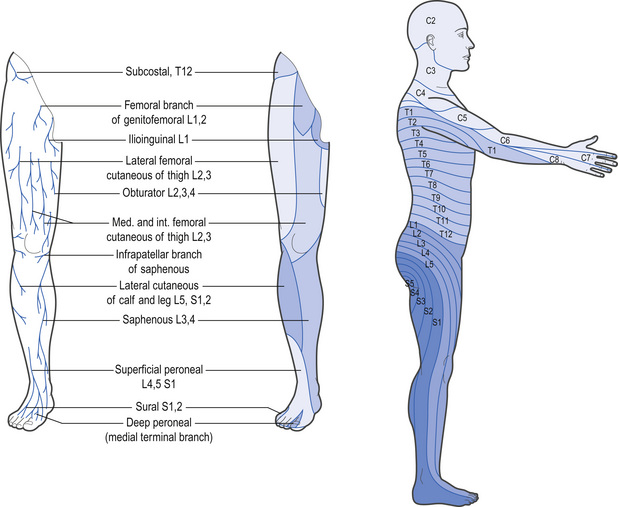
The principle aims of acupuncture are to modulate pain and inflammation; improve circulation to the hip joint; and maintain muscle length and strength. Initially treatment should be aimed at segmental (Table 9.2) inhibition and pain-gate mechanisms whilst aiding blood flow and stimulating an anti-inflammatory response. Local segmental points on the Bladder channel will facilitate segmental dorsal horn inhibition, whilst distal points corresponding to the dermatome involvement (Fig. 9.1) will encourage a descending inhibitory response. Here a choice of points may be available, depending on the pain pattern.
Table 9.2 Segmental innervation and acupuncture points
| Segmental innervation | Segmental acupuncture points | Dermatome points |
|---|---|---|
| Anterior hip joint capsule is innervated by sensory articular branches from the femoral nerve L2 L3 | BL23 BL24 HJJ @ L2/L3 GV4 @ L2 ST30 + ST31 | GB31 ST34 SP12 LIV11 |
| Anteromedial innervation is determined by the articular branches of the obturator nerve | LIV11 LIV10 SP11 SP10 | SP11 SP10 |
| Posterior hip joint and capsule. The sciatic nerve | BL25 BL26 | GB30 GV3 HJJ@ L5/S1 |
| Posteromedial section of the hip joint capsule is innervated by articular branches of the anterior rectus femoral nerve | BL25 BL26 | BL53 BL54 |
| Posterolateral section of the hip joint capsule innervated by superior gluteal nerve | BL26 BL27 | KID10 BL36 BL37 |
| S1-S3 sciatic nerve | BL27 BL28 BL29 | BL36 BL37 BL40 BL60 BL62 |
Notes: BL, Bladder; HJJ, Huatuojiaji; GV, Governor Vessel; ST, Stomach; LIV, Liver; SP, Spleen; KID, Kidney.
With the enormous muscle bulk running over the hip joint, the myofascial element should not be ignored. Resolution of associated trigger points will often reduce pain and facilitate muscle imbalance re-education; pain and abnormal function may often be attributed to myofascial trigger points (MTrPts). If the patient presents with both myofascial and articular dysfunction rehabilitation is generally steady and progressive (Whyte-Ferguson & Gerwin 2005). Myofascial involvement commonly involves the following muscles:
The exact aetiology and pathophysiology of MTrPts remain unknown. The MTrPts have been described as having a characteristic EMG pattern termed spontaneous electrical activity (SEA) (Chen et al 2001). This SEA is characterized by continuous low-level EMG activity with superimposed large-amplitude spikes (Simmons et al 1995). Some EMG studies have recorded SEA active MTrPts in both humans (Hubbard & Berkoff 1993) and rabbits (Chen et al 2001). Contemporary opinion is that SEA is the result of acetylcholine leakage from the motor end-plate. The magnitude of this leakage is at a sufficient level to create a mini depolarization of the postsynaptic junction and result in the contraction of a small number of muscle fibres rather that the whole muscle (Huguenin et al 2005). Continued acetylcholine release and subsequent muscle contraction are thought to reduce the oxygen supply to the muscle, and consequently, an ischaemic environment ensues in which there is insufficient adenosine triphosphate (ATP) available to initiate release of the actin-myosin complex.
Chen et al (2001) found that the SEA in rabbit MTrPts could be reduced with needling. In comparison to controlled needling, needling of the active TrPt in the rabbit resulted in significantly lower normalized SEA in 7 out of 9 rabbits. Although this study primarily provides evidence for the efficacy of MTrPt needling in reducing SEA, it remains unknown whether reducing SEA is required to achieve pain relief. The study by Chen et al (2001) did not measure pressure-pain threshold pre- or post-treatment. To date, there is insufficient evidence to support or refute a reduction in SEA in MTrPt acupuncture.
In addition to a peripheral effect on the motor end-plate, MTrPt injection has been shown to activate diffuse noxious inhibitory control (DNIC). Fine et al (1988) investigated the effects of administering the opioid antagonist naloxone in MTrPt injections. The study found that MTrPt injections were effective in improving ROM and pressure-pain scores. The administration of 10 mg naloxone significantly reversed the effects of the MTrPt injections. The findings of this study would suggest that central opioid activation is an underlying mechanism in the pain relief obtained from MTrPt injections.
Activation of DNIC and the subsequent release of opioids has been shown to reduce nociceptive transmission to higher centres at the spinal cord level (Fine et al 1988). It is possible that the reason why some studies fail to demonstrate a difference between placebo and MTrPt is that the placebo needling is of sufficient level of stimulus to activate DNIC. Furthermore, the clinical improvement from manual, soft tissue MTrPt therapy may also share the same pathway for its analgesic effects with acupuncture. Clinically, it is relevant to consider what level of stimulus is effective in activating DNIC and achieving pain relief in subjects with MTrPt, rather than debating whether the stimulus is a placebo or a real treatment (Smith & Crowther 2002).
The sympathetic nervous system (SNS) has also been implicated in MTrPts. In an animal model Chen et al (1998) demonstrated that phentolomine reduced the SEA in rabbit MTrPts when compared with a control injection of saline. Although direct extrapolation of this finding to human subjects is limited, the study provides some preliminary data that suggest that sympathetic activity may contribute to myofascial MTrPt pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree