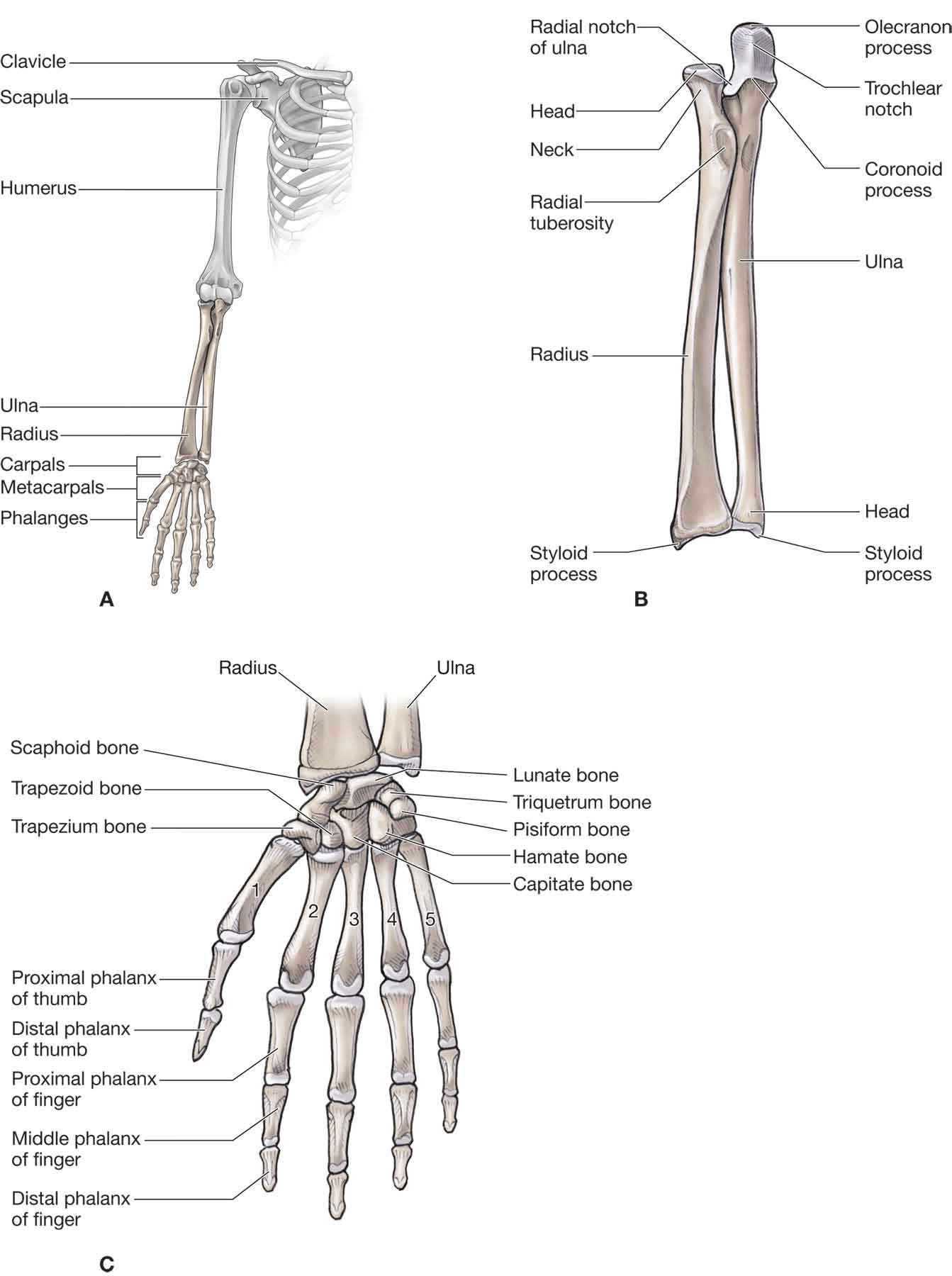
A hand is a very personal thing. It is the interface between the patient and his or her world. It is an emblem of strength, beauty, skill, sexuality, and sensibility. When it is damaged, it becomes a symbol of vulnerability of the whole patient. —Paul W. Brand (1914–2003) In a sense, the shoulder, elbow, and wrist joints (Fig. 18-1) are merely mechanical devices that contribute to the usefulness of the hand.1 The correct synchronization of these biological devices, coupled with patient motivation, produces a remarkable level of dexterity and precision. FIGURE 18-1 Arm, wrist, and hand joint structures. (Reproduced, with permission, from Chapter 29. Overview of the Upper Limb. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The carpus, or wrist, represents a highly complex anatomic structure, comprising a core structure of 8 bones; more than 20 radiocarpal, intercarpal, and carpometacarpal (CMC) joints; 26 named intercarpal ligaments; and 6 or more parts of the triangular fibrocartilage complex (TFCC).2 While these structures can be differentiated anatomically, they are functionally interrelated with movement in one joint having an effect on the motion of neighboring joints. This relationship extends as far as the elbow. The hand accounts for about 90% of upper limb function.3 The thumb, which is involved in 40–50% of hand function, is the more functionally important of the digits.3 The index and middle fingers are each involved in about 20% of hand function, and are the second most important, with the ring finger being the least important. The middle finger is the strongest finger and is important for both precision and power functions.3 The following sections describe the respective bones, joints, soft tissues, and nerves, detailing both their individual and collective functions. For simplicity’s sake, the forearm, wrist, and hand are separated into their various compartments.
CHAPTER 18
The Forearm, Wrist, and Hand
OVERVIEW
ANATOMY
Distal Radioulnar Joint
The distal radioulnar joint (DRUJ) plays a significant role in wrist and forearm function. The DRUJ is a uniaxial pivot joint that joins the distal radius and ulna and an articular disk (Fig. 18-1). The articular disk, known as the TFCC, assists in binding the distal radius and is the main stabilizer of the DRUJ (see the next section).4
At its distal end, the radius widens to form a broad, concave articular surface. The articular surface has an ulnar inclination in the frontal plane, which averages 23 degrees, and an anterior (palmar) inclination in the sagittal plane, which averages 11 degrees.5 The distal end of the ulna expands slightly laterally into a rounded head and medially into an ulnar styloid process (Fig. 18-1). The rounded head of the ulnar head contacts both the ulnar notch of the radius laterally and the TFCC distally.6 The ulnar styloid process is approximately one-half inch shorter than the radial styloid process, resulting in more ulnar deviation than radial deviation being available.6 The articular capsule, which attaches to the articular margins of the radius and ulna and to the disk enclosing the inferior radioulnar joint, is lax. Anterior (palmar) and posterior (dorsal) radioulnar ligaments strengthen the capsule anteriorly and posteriorly. Forearm supination tightens the anterior capsule and pronation tightens the posterior part, adding to the overall stability of the wrist.7
The DRUJ functions to transmit the loads from the hand to the forearm.
Triangular Fibrocartilage Complex
The TFCC essentially comprises a fibrocartilage disk interposed between the medial proximal row and the distal ulna within the medial aspect of the wrist.8 The primary function of the TFCC is to enhance joint congruity and to cushion against compressive forces. Indeed, the TFCC transmits about 20% of the axial load from the hand to the forearm.7 The broad base of the disk is attached to the medial edge of the ulnar notch of the radius, and its apex is attached to the lateral aspect of the base of the ulnar styloid process. The disk’s anterior and posterior borders are thickened.
A number of ligaments originate from the TFCC and provide support to it. These include the ulnolunate and ulnotriquetral ligaments, the ulnar collateral, and the radioulnar ligaments. Other structures that lend support to the TFCC include the following:
 The ulnocarpal ligaments.
The ulnocarpal ligaments.
 The sheath of the extensor carpi ulnaris (ECU) tendon, which is the only wrist tendon that broadly connects to the TFCC.
The sheath of the extensor carpi ulnaris (ECU) tendon, which is the only wrist tendon that broadly connects to the TFCC.
Both the superior and the inferior articular surfaces of the TFCC are smooth and concave.8 The disk separates the distal ulna from direct contact with the carpals but allows gliding between the carpals, disk, and ulna during forearm pronation and supination.8,9
The TFCC is innervated by branches of the posterior interosseous, ulnar, and posterior (dorsal) sensory ulnar nerves.9
The Wrist
The wrist comprises the distal radius and ulna, eight carpal bones, and the bases of five metacarpals (Fig. 18-1). The carpal bones lie in two transverse rows. The proximal row contains (lateral to medial) the scaphoid (navicular), lunate, triquetrum, and pisiform. The distal row holds the trapezium, trapezoid, capitate, and hamate.
Radiocarpal Joint
The radiocarpal joint, a biaxial ellipsoid joint, is formed, by the large, articular concave surface of the distal end of the radius, the proximal carpal row, and the TFCC. The lunate and triquetrum articulate with the TFCC. A radial styloid process projects distally from the lateral side of the radius. A cartilage-covered ulnar notch occupies the distal medial side of the radius.10 Posteriorly, a posterior (dorsal) (Lister) tubercle arises near the center of the radius, forming a pulley around which the extensor pollicis longus (EPL) tendon passes.9 Lister tubercle is a common site of attritional changes and potential tendon rupture.11
The Carpals
Scaphoid
The scaphoid (Fig. 18-1) is the largest of the proximal carpal row bones, and its shape resembles that of a boat or canoe (thus the old term navicular).9 The scaphoid bone links the proximal and distal carpal rows and helps provide stability to the wrist joint.
The scaphoid is tethered to the proximal carpal row by a number of strong ligamentous attachments, and two-thirds of its surface area is articular. The proximal surface of the scaphoid is convex and articulates with the radius. The medial surface is concave and articulates with the capitate.10 The articulating surface for the lunate is flat. The distal surface consists of two convex facets for articulation with the trapezium and trapezoid (the scaphotrapeziotrapezoid joint).9 The round tubercle on the inferolateral part of its anterior (palmar) surface serves as the attachment of the flexor retinaculum and the abductor pollicis brevis (APB).10 The blood vessels to this bone enter the scaphoid at or distal to the wrist. This configuration predisposes a fracture on the proximal aspect to aseptic necrosis.12 In addition, as the scaphoid plays a critical role in coordinating and stabilizing movements between the proximal and the distal rows of the carpals, damage to the intrinsic and extrinsic ligaments that support the scaphoid can result in persistent pain and dysfunction with loading activities.13–15
Lunate
The lunate (Fig. 18-1) articulates between the scaphoid and the triquetrum in the proximal carpal row. Its smooth convex proximal surface articulates with the radius and the TFCC at the lunate fossa.10 Its lateral surface contains a flat semilunar facet for the scaphoid. The medial surface articulates with the triquetrum. The distal surface is deeply concave and articulates with the edge of the hamate in adduction and the medial aspect of the capitate.10
Triquetrum
The triquetrum (Fig. 18-1) is a pyramid-shaped bone. It articulates with the pisiform on its distal anterior (palmar) surface at the pisiform–triquetral joint.10 The almost square distal–medial surface of the triquetrum articulates with the concavo–convex surface of the hamate. The ulnar collateral ligament (UCL) attaches to the medial and posterior (dorsal) surfaces of the triquetrum.10 The proximal surface of the triquetrum articulates with the TFCC in full adduction.9 The lateral surface of the triquetrum articulates with the lunate.
Pisiform
The pisiform (Fig. 18-1), as its name implies, is shaped like a “P” with a posterior (dorsal) flat articular facet for the triquetrum.10 The pisiform, formed within the tendon of the flexor carpi ulnaris (FCU), is a sesamoid bone and serves as an attachment for the flexor retinaculum, abductor digiti minimi (ADM), UCL, pisohamate ligament, and pisometacarpal ligament. The pisiform also functions to increase the flexion moment of the FCU.9
As mentioned, the pisiform articulates with the anterior (palmar) surface of the triquetral and is thus separated from the other carpal bones, all of which articulate with their neighbors. The pisiform is closely related to the ulnar artery and nerve on its radial border, the nerve being the closer.16
Trapezium
The trapezium (Fig. 18-1) has a groove on its medial anterior (palmar) surface which contains the tendon of the FCR.10 To its margins are attached two layers of the flexor retinaculum. The opponens pollicis (OP) is between the flexor pollicis brevis (FPB) distally and the APB proximally.10 The lateral surface serves as an attachment site for the radial collateral ligament and capsular ligament of the first CMC joint. The distal articulating surface of the trapezium is saddle shaped. Medially, its concave surface articulates with the trapezoid, whereas more distally its convex surface articulates with the second metacarpal base.10 Proximally, its concave surface articulates with the scaphoid.
Trapezoid
The trapezoid (Fig. 18-1) is small and irregular. The distal surface articulates with the grooved second metacarpal base. The medial surface articulates via a concave facet with the distal part of the capitate. The lateral surface of the trapezoid articulates with the trapezium, and its proximal surface articulates with the scaphoid bone.10
Capitate
The capitate (Fig. 18-1) is the most central and the largest of the carpal bones. Its distal aspect articulates with the third metacarpal base. Its lateral border articulates with the medial side of the second metacarpal base.10 The convex proximal head of the capitate articulates with the lunate and scaphoid. The medial surface of the head articulates with the lunate, and the lateral aspect of the head articulates with the scaphoid.10 Medially, the capitate articulates with the hamate.
With its central location, the capitate serves as the keystone of the proximal transverse arch. This arch is important to the prehensile activity of the hand.9,17,18
Hamate
The hamate (Fig. 18-1) is a cuneiform bone and contributes to the medial wall of the carpal tunnel. To the hook (hamulus) of the hamate is attached the flexor retinaculum. The hamate articulates with three carpal bones and two metacarpals.9 The medial surface articulates with the triquetrum and by association with the pisohamate ligament, the pisiform. The lateral surface articulates with the capitate.10 On its distal aspect, the hamate articulates with the fourth and fifth metacarpal heads.
Midcarpal Joints
The midcarpal joint lies between the two rows of carpals. It is referred to as a “compound” articulation because each row has both a concave and a convex segment. Wrist flexion, extension, and radial deviation are mainly midcarpal joint motions. Approximately 50% of the total arc of wrist flexion and extension occur at the midcarpal level with more flexion (66%) occurring than extension (34%).19
The proximal row of the carpals is convex laterally and concave medially. The scaphoid, lunate, trapezium trapezoid, and triquetrum present with a concave surface to the distal row of carpals. The scaphoid, capitate, and hamate present a convex surface to a reciprocally arranged distal row.
First CMC Joint
The thumb is the most important digit of the hand and greatly magnifies the complexity of human prehension.20,21 Functionally, the sellar (saddle-shaped) CMC joint is the most important joint of the thumb and consists of the articulation between the base of the first metacarpal and the distal aspect of the trapezium.
The articular surfaces of the trapezium and the proximal end of the first metacarpal are reciprocally shaped. Three other adjacent articulations are functionally related to this joint, which include the joints between the trapezium and the scaphoid, the trapezium and the trapezoid, and the base of the first metacarpal and the radial side of the base of the second metacarpal.20,21
Motions that can occur at this joint include flexion/extension, adduction/abduction, and opposition, the latter of which includes varying amounts of flexion, internal rotation, and anterior (palmar) adduction (see “Biomechanics”). Although the joint capsule of the first CMC joint is large and relatively loose, motions at the joint are controlled and supported by muscle actions and by at least five ligaments: anterior oblique, ulnar collateral, intermetacarpal, posterior oblique, and radial collateral. In general, most of the thumb ligaments are placed on tension with abduction, extension, and opposition.20,21
Other CMC Joints
The distal borders of the distal carpal row bones articulate with the bases of the metacarpals, thereby forming the CMC joints. The CMC articulations of the fingers permit only gliding movements. The CMC joints progress in mobility from the second to the fifth, with the second and third metacarpal joints being relatively immobile, and thus the primary stabilizing joints of the hand. The fourth and fifth CMC joints are more mobile to permit the hand to adapt to objects of different shapes during grasping.
Stability for the CMC joints is provided by the anterior (palmar) and posterior (dorsal) CMC and intermetacarpal ligaments. While the trapezoid articulates with only one metacarpal, all of the other members of the distal carpal row combine one carpal bone with two or more metacarpals.
Metacarpophalangeal Joints
The five metacarpals resemble miniature versions of the long bones of the body, with elongated shafts and expanded ends. The metacarpophalangeal (MCP) joint of the thumb is a hinge joint. Its bony configuration, which resembles the interphalangeal (IP) joints, provides it with some inherent stability. In addition, support for the joint is provided by anterior (palmar) and collateral ligaments. The MCP joint of the thumb consists of a convex surface on the head of the metacarpal and a concave surface on the base of the phalanx. The area of the articulating surface is increased by the presence of a volar plate, which allows a greater range of motion than would be available otherwise. Approximately 75–80 degrees of flexion is available at this joint. The extension movements, as well as the abduction and adduction motions, are negligible. Traction, gliding, and rotatory accessory movements are also present.
The second through fifth metacarpals articulate with the respective proximal phalanges within biaxial joints. Their widened, proximal bases articulate with the carpals and with one another in plane joints.10 Their biconvex distal heads are broader anteriorly than posteriorly, the significance of which is discussed later.
The MCP joints allow flexion–extension and medial–lateral deviation associated with a slight degree of axial rotation. The design of the MCP joint allows for great amplitude of movement, at the expense of stability.
Approximately 90 degrees of flexion is available at the second MCP, with the amount of available flexion progressively increasing toward the fifth MCP. Active extension at these joints is 25–30 degrees while 90 degrees can be obtained passively. A loss of flexion and extension at the CMC joint of the little finger reduces the amount of opposition available, resulting in dysfunction of the prehensile pattern and difficulty in making a fist.6 Approximately 20 degrees of abduction/adduction can occur in either direction at the MCP, with more being available in extension than in flexion. Abduction–adduction movements of the MCP joints are restricted in flexion and free in extension.
The joint capsules are attached to the articular margins of the metacarpals and phalanges and surround the MCP joints. The joint capsule of these joints is relatively lax and redundant but is endowed with collateral ligaments that pass posterior to the joint axis for flexion/extension of the MCP joints (Fig. 18-11). Although, these collateral ligaments are lax in extension, they become taut in approximately 70–90 degrees of flexion of the MCP joint.22
The posterior (dorsal) hood apparatus reinforces (or replaces) the posterior (dorsal) joint capsules. The fibrocartilaginous volar plates reinforce the anterior (palmar) aspects of the joints (Fig. 18-12). The volar plates attach firmly to the phalangeal bases but connect only loosely to the metacarpal heads by membranous fibers. Their posterior (dorsal) surface contributes to the joint area, whereas their anterior (palmar) surface channels the finger flexor tendons.23
The asymmetry of the metacarpal heads as well as the difference in length and direction of the collateral ligaments also explains the rotational movement of the proximal phalanx during flexion–extension and why the ulnar deviation of the digits normally is greater than the radial deviation.23 The rotary movements that occur are called conjunct rotations. The index finger has a conjunct rotation of internal rotation with abduction and flexion, whereas the ring and little finger each have a conjunct rotation of external rotation with abduction and flexion. The middle finger is not thought to have a conjunct rotation.
IP Joints
Adjacent phalanges articulate in hinge joints that allow motion in only one plane: sagittal. The congruency of the IP joint surfaces contributes greatly to IP joint stability. In addition, the IP joints are surrounded by joint capsules that are attached to the articular margins of the phalanges.
Proximal Interphalangeal Joint
The proximal interphalangeal (PIP) joint is a hinged joint capable of flexion and extension. The supporting ligaments and tendons provide the bulk of the static and dynamic stability of this joint as it travels through a normal range of 110 degrees.22,24–27 The capsule surrounding the articular surface of the joint is composed of the volar plate, lateral and accessory collateral ligaments, and extensor expansion.
The proximal IP joint is stable in all positions. The configuration of the volar plate allows it to function as a static restraint to hyperextension and to influence the mechanical advantage of the flexor tendons at the initiation of PIP joint flexion.22 The volar plate also increases the surface area. This allows for a greater range of motion than would be available otherwise.
The thick collateral ligaments (true and accessory) of the PIP joint combine with the volar plate to provide lateral stability: the collateral ligaments of the PIP joints are maximally taut at 25 degrees of finger flexion.22 For this reason, the IP joints are usually splinted in 25 degrees of flexion following surgery to prevent joint contractures. The splinting position is changed as the patient resumes function.
The flexor tendon system at the level of the PIP joint is less complex than the extensor mechanism and contributes very little to injuries about the PIP joint.22
The phalangeal bases effectively form a sellar surface, with bone projections allowing for a wide range of accessory movements to accommodate the gripping of a large array of irregular surfaces.
The motions available at these joints consist of approximately 110 degrees of flexion at the PIP joints and 90 degrees at the thumb IP joint. Extension reaches 0 degrees at the PIP joints and 25 degrees at the thumb IP joint. Traction, gliding, and accessory movements also occur at the IP joints.
Distal Interphalangeal Joints
The distal interphalangeal (DIP) joint has similar structures as the PIP joint but less stability and allows some hyperextension. The motions available at these joints consist of approximately 90 degrees of flexion and 25 degrees of extension. Traction, gliding, and accessory movements also occur at the DIP joints.
Carpal Ligaments
Excessive migration of the carpal bones is prevented by strong ligaments (Table 18-1) and by the ulnar support provided by the TFCC. The major ligaments of the wrist are depicted in Figure 18-2.
TABLE 18-1 | Ligaments of the Wrist |
Interosseous | Intrinsic Midcarpal | Extrinsic Radiocarpal/Ulnocarpal |
Distal row | Posterior (dorsal) | Posterior (dorsal) |
Trapezium trapezoid | Scaphotriquetral | Posterior (dorsal) radiocarpal |
Trapezoid capitate | Posterior (dorsal) intercarpal | |
Capitohamate | ||
Proximal row | Anterior (palmar) | Anterior (palmar) |
Scapholunate | Scaphotrapeziotrapezoid | Radioscaphocapitate |
Lunotriquetral | Scaphocapitate | Long radiolunate |
Triquetrocapitate | Short radiolunate | |
Triquetrohamate | Radioscapholunate | |
Ulnolunate Ulnotriquetral Ulnocapitate | ||
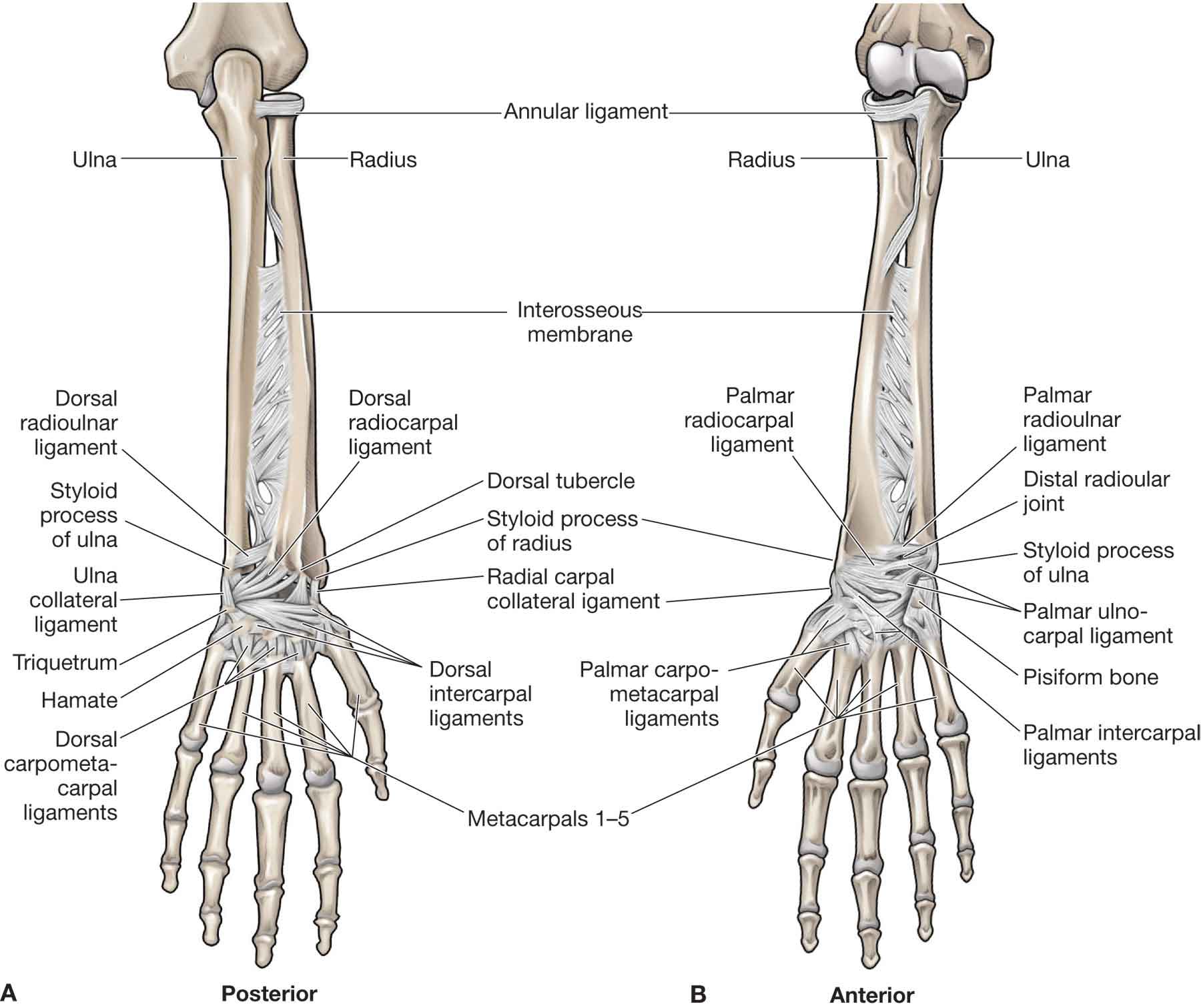
FIGURE 18-2 The major ligaments of the wrist. (Reproduced, with permission, from Chapter 32. Forearm. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The ligaments of the wrist provide support for the region. These ligaments can be divided into two types: extrinsic and intrinsic (Table 18-1). The extrinsic anterior (palmar) ligaments provide the majority of wrist stability. The intrinsic ligaments serve as rotational restraints, binding the proximal row into a unit of rotational stability.28 The proximal row of carpals has no muscle insertions. Its stability depends entirely on the capsular and interosseous ligaments between the scaphoid, lunate, and triquetrum.29 The ligaments between the proximal and the distal carpal rows provide support, centering especially on the capitate.10 The midcarpal ligaments, which are longer than the interosseous ligaments, cross the midcarpal joint and connect bones of the distal and proximal rows on both the posterior (dorsal) and the anterior (palmar) surfaces.9 No midcarpal ligaments directly attach to the lunate.
Antebrachial Fascia
The antebrachial fascia is a dense connective tissue that encases the forearm and maintains the relationships of the tendons that cross the wrist. The fascia is firmly attached to the subcutaneous border of the ulna, from which it sends a septum to the radius. This septum divides the forearm into an anterior compartment and a posterior compartment (see “Muscles of the Wrist and Forearm”).
The Extensor Retinaculum
At the point where the tendons cross the wrist, there is a ligamentous structure called a retinaculum that appears to lay over the tendons and their sheaths (Fig. 18-3). This retinaculum serves to prevent the tendons from “bowstringing” when the tendons turn a corner at the wrist.30 The extensor retinaculum extends from the lateral border of the distal radius across the posterior (dorsal) surface of the distal forearm onto the posterior surface of the distal ulna and ulnar styloid process. It then wraps part way around the ulna to attach to the triquetrum and pisiform bones. The retinaculum and the underlying bones form six tunnel-like structures called fibro-osseous compartments on the dorsum of the wrist (Fig. 18-3). The compartments, from lateral to medial, contain the tendons of
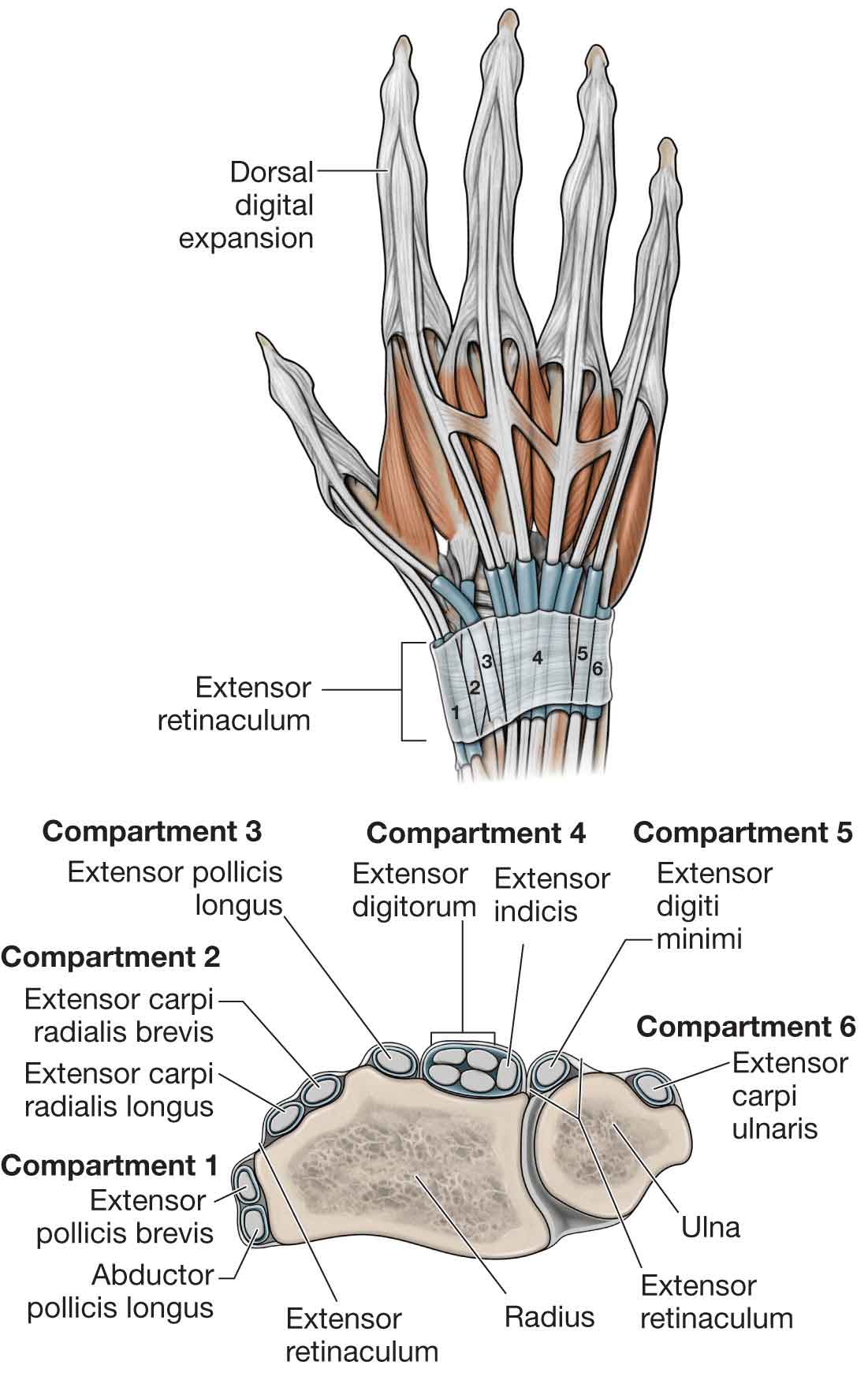
FIGURE 18-3 Extensor retinaculum and extensor tendons. (Reproduced, with permission, from Chapter 33. Hand. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
 abductor pollicis longus (APL) and extensor pollicis brevis (EPB)
abductor pollicis longus (APL) and extensor pollicis brevis (EPB)
 extensor carpi radialis longus (ECRL) and brevis (ECRB)
extensor carpi radialis longus (ECRL) and brevis (ECRB)
 EPL
EPL
 extensor digitorum (ED) (four tendons) and extensor indicis (EI) (not shown in Fig. 18-3)
extensor digitorum (ED) (four tendons) and extensor indicis (EI) (not shown in Fig. 18-3)
 extensor digiti minimi (EDM)
extensor digiti minimi (EDM)
 ECU
ECU
As these tendons pass through the compartments, they are invested with synovial sheaths.
The posterior (dorsal) compartments serve to enhance the efficiency and effectiveness of the wrist and finger extensors (see “Extensor Hood”) (Fig. 18-4). Proximal to the metacarpal heads, juncture tendineae connect the four tendons of the ED muscles, limiting their independent motion.6 For example, flexion of the middle and little fingers restricts extension of the ring finger MCP joint because the juncture tendineae pulls the ring finger extensor tendon distally. Conversely, extension of the ring finger exerts an extensor force upon its neighbors, such that they can be actively extended even if the middle and little finger extensor tendons are severed proximal to the juncture.6
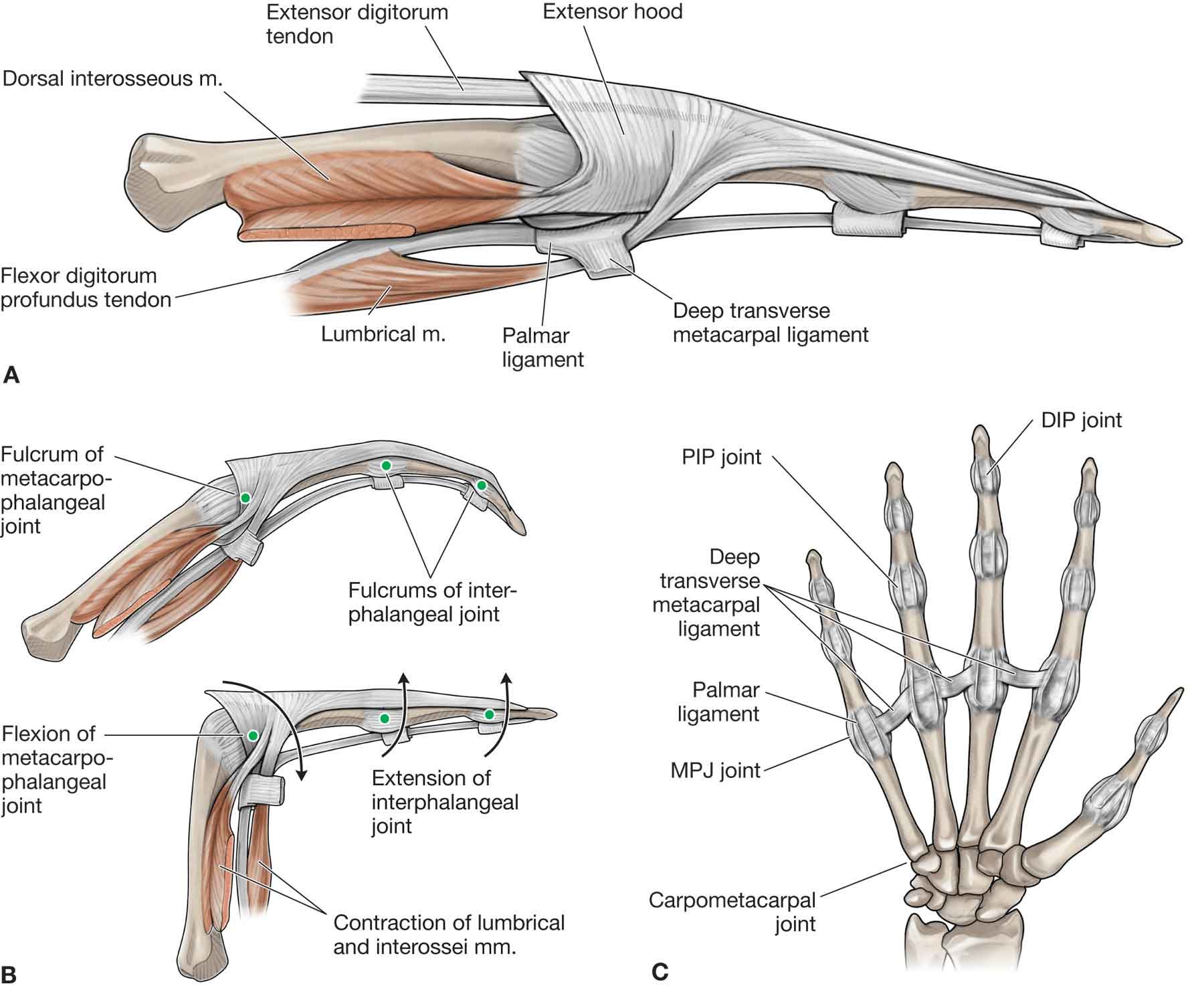
FIGURE 18-4 Extensor hood and smaller ligaments of the hand. (Reproduced, with permission, from Chapter 33. Hand. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The Flexor Retinaculum
The flexor retinaculum (transverse carpal ligament) spans the region between the pisiform, hamate, scaphoid, and trapezium, transforming the carpal arch into a tunnel, through which the median nerve and some of the tendons of the hand pass (Fig. 18-5). The proximal attachment of the retinaculum is at the tubercle of the scaphoid and the pisiform. The hook of the hamate and the tubercle of the trapezium serve as its distal attachment. The retinaculum also6:
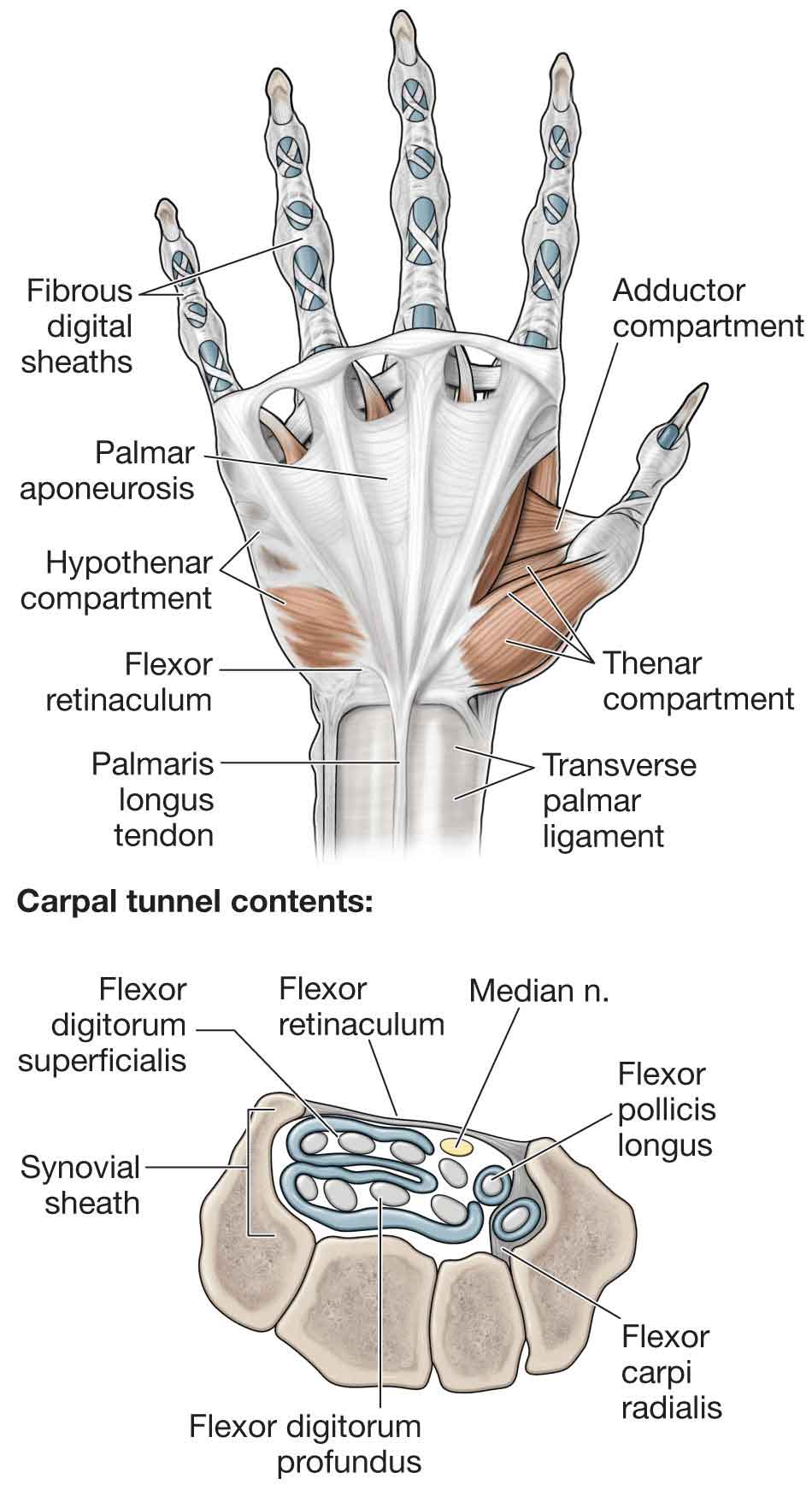
FIGURE 18-5 Flexor retinaculum and flexor tendons. (Reproduced, with permission, from Chapter 33. Hand. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
 serves as an attachment site for the thenar and hypothenar muscles
serves as an attachment site for the thenar and hypothenar muscles
 helps maintain the transverse carpal arch
helps maintain the transverse carpal arch
 acts as a restraint against bowstringing of the extrinsic flexor tendons, and
acts as a restraint against bowstringing of the extrinsic flexor tendons, and
 protects the median nerve.
protects the median nerve.
In the condition known as carpal tunnel syndrome (CTS), the median nerve is compressed in this relatively unyielding space (see “Intervention Strategies”). The structures that pass deep to the flexor retinaculum (Fig. 18-5) include
 flexor digitorum superficialis (FDS),
flexor digitorum superficialis (FDS),
 flexor digitorum profundus (FDP),
flexor digitorum profundus (FDP),
 flexor pollicis longus (FPL), and
flexor pollicis longus (FPL), and
 flexor carpi radialis (FCR).
flexor carpi radialis (FCR).
The structures that pass superficial to the flexor retinaculum include
 the ulnar nerve and artery,
the ulnar nerve and artery,
 the tendon of the palmaris longus, and
the tendon of the palmaris longus, and
 the sensory branch (anterior (palmar) branch) of the median nerve.
the sensory branch (anterior (palmar) branch) of the median nerve.
Fibrous sheaths between the distal anterior (palmar) crease and the PIP joints bind the flexor tendons to the fingers. Some surgeons refer to the area where the sheaths contain two tendons as “no man’s land.”6
Carpal Tunnel
The carpal tunnel serves as a channel for the median nerve and nine flexor tendons (Fig. 18-5). The floor of the tunnel is formed by the anterior (palmar) radiocarpal ligament and the anterior (palmar) ligament complex. As mentioned previously, the roof of the tunnel is formed by the flexor retinaculum. The radial and ulnar are formed by carpal bones (hook of hamate and trapezium, respectively). The median nerve divides into a motor branch and distal sensory branches within the tunnel.
Tunnel of Guyon
The tunnel of Guyon is located superficial to the flexor retinaculum, between the hook of the hamate and the pisiform bones. The anterior (palmar) carpal ligament, palmaris brevis muscle, and the anterior (palmar) aponeurosis form its roof. Its floor is formed by the flexor retinaculum (transverse carpal ligament), pisohamate ligament, and pisometacarpal ligament.6 The tunnel functions as a passageway for the ulnar nerve and artery into the hand.
Phalanges
The 14 phalanges each consist of a base, shaft, and head (Fig. 18-1). Two shallow depressions, which correspond to the pulley-shaped heads of the adjacent phalanges, mark the concave proximal bases. Two distinct convex condyles produce the pulley-shaped configuration of the phalangeal heads.6
Anterior (Palmar) Aponeurosis
The anterior (palmar) aponeurosis, which consists of a dense fibrous structure continuous with the palmaris longus tendon and fascia covering the thenar and hypothenar muscles, is located just deep to the subcutaneous tissue (Fig. 18-5). The aponeurosis travels distally to attach to the transverse metacarpal ligaments and flexor tendon sheaths. The aponeurosis offers some protection for the ulnar artery and nerve, and digital vessels and nerves. From the central region of the palm, the aponeurosis continues toward the fingers and splits into four slips. As these slips approach the MCP joints, they split and wrap around the tendons of their respective digit. Dupuytren contracture is a fibrotic condition of the anterior (palmar) aponeurosis that results in nodule formation or scarring of the aponeurosis and which may ultimately cause finger flexion contractures (see “Intervention Strategies”).
Extensor Hood
At the level of the MCP joint, the tendon of the ED fans out to cover the posterior (dorsal) aspect of the joint in a hood-like structure (Fig. 18-4). A complex tendon that covers the posterior (dorsal) aspect of the digits is formed from a combination of the tendons of insertion from the ED, EI, and EDM. The distal portion of the hood receives the tendons of the lumbricals and interossei over the proximal phalanx. The tendons of the intrinsic muscles pass anterior (palmar) to the MCP joint axes but posterior (dorsal) to the PIP and DIP joint axes (Fig. 18-6). Between the MCP and the PIP joints, the complete, complex ED tendon (after all contributions have been received) splits into three parts: a central slip and two lateral bands6:
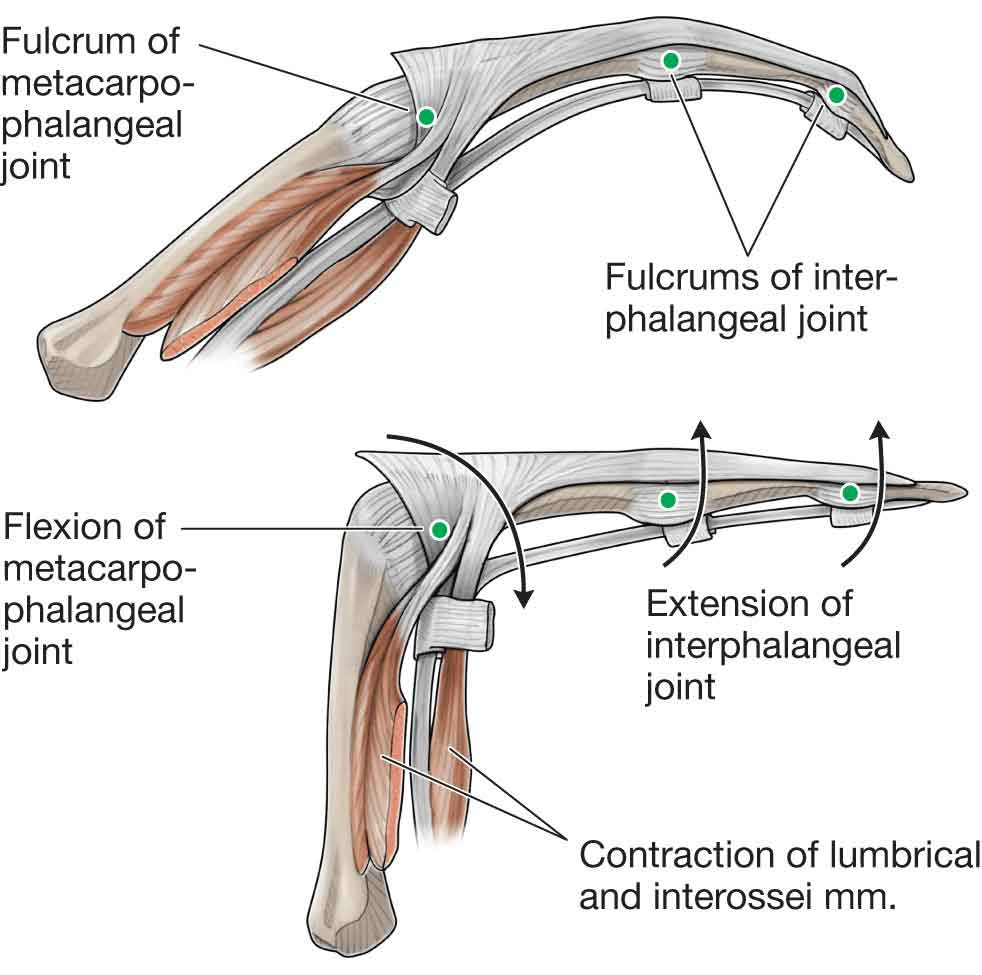
FIGURE 18-6 The tendons of the intrinsic muscles in relation to the joints. (Reproduced, with permission, from Chapter 33. Hand. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
 A central band. This band inserts into the proximal posterior (dorsal) edge of the middle phalanx.
A central band. This band inserts into the proximal posterior (dorsal) edge of the middle phalanx.
 The lateral bands. These bands rejoin over the middle phalanx into a terminal tendon, which inserts into the proximal posterior (dorsal) edge of the distal phalanx. Rupture of the tendon insertion into the distal phalanx produces a “mallet” finger (see “Intervention Strategies”). The lateral bands, comprised of the fibers from both extrinsic and intrinsic tendons, are prevented from dislocating posteriorly (dorsally) by the transverse retinacular ligaments, which link them to the volar plates of the PIP joints.6
The lateral bands. These bands rejoin over the middle phalanx into a terminal tendon, which inserts into the proximal posterior (dorsal) edge of the distal phalanx. Rupture of the tendon insertion into the distal phalanx produces a “mallet” finger (see “Intervention Strategies”). The lateral bands, comprised of the fibers from both extrinsic and intrinsic tendons, are prevented from dislocating posteriorly (dorsally) by the transverse retinacular ligaments, which link them to the volar plates of the PIP joints.6
The arrangement of the muscles and tendons in this expansion hood creates a cable-like system that provides a mechanism for extending the MCP and IP joints and allows the lumbrical and possibly interosseous muscles to assist in the flexion of the MCP joints.
Stretching or laxity of these supporting structures allows “bowstringing” of the lateral bands, which transmit excessive extension force to the PIP joint.6
The oblique retinacular ligament (Landsmeer ligament) assists in the extensor hood mechanism. The ligament attaches between the PIP volar plate, where it is anterior (palmar) to the PIP joint axis, and the terminal tendon, where it is posterior (dorsal) to the DIP joint axis. This relationship to the PIP and DIP joints is essentially the same as that of the intrinsic muscles (lumbricals and interosseous) to the MCP and PIP joints—when the PIP joint extends, the oblique retinacular ligament exerts a passive extensor force on the DIP joint, and when the PIP joint flexes, it allows the DIP joint to flex.31
PIP joint position also may influence DIP joint position through lateral band action. The lateral bands normally slip palmarly upon PIP joint flexion, decreasing the excursion required for full DIP joint flexion. If scar tissue tethers the lateral bands so that they do not move palmarly, then simultaneous full flexion at both the PIP and the DIP joints at the same time is not possible.6
Synovial Sheaths
Synovial sheaths can be thought of as long narrow balloons filled with synovial fluid, which wrap around a tendon so that one part of the balloon wall (visceral layer) is directly on the tendon, while the other part of the balloon wall (parietal layer) is separate.30 During wrist motions, the sheaths move longitudinally, reducing friction.
At the wrist, the tendons of both the FDS and the FDP are essentially covered by a synovial sheath and pass posterior (dorsal) (deep) to the flexor retinaculum. The FDP tendons are posterior (dorsal) to those of the FDS.
In the palm, the FDS and FDP tendons are covered for a variable distance by a synovial sheath.
At the base of the digits, both sets of tendons enter a “fibro-osseous tunnel” formed by the bones of the digit (head of the metatarsals and phalanges) and a fibrous digital tendon sheath on the anterior (palmar) surface of the digits.
Flexor Pulleys
Annular (A) and cruciate (C) pulleys restrain the flexor tendons to the metacarpals and phalanges and contribute to fibro-osseous tunnels through which the tendons travel.11 The A1 pulley arises from the MCP joint and volar plate; A2 from the proximal phalanx; A3 from the PIP joint volar plate; A4 from the middle phalanx; and A5 from the DIP joint volar plate.11 The C1 pulley originates near the head of the proximal phalanx; C2 near the base of the middle phalanx; and C3 near the head of the middle phalanx.11
The pulley system of the thumb includes the A1 arising from the MCP joint anterior (palmar) plate, A2 from the IP joint anterior (palmar) plate, and the oblique pulley from the proximal phalanx.11
Anatomic Snuffbox
The anatomic snuffbox (Fig. 18-7) is a depression on the posterior (dorsal) surface of the hand at the base of the thumb, just distal to the radius. This structure can be observed during active radial abduction of the thumb. The radial border of the snuffbox is formed by the tendons of the APL and EPB while the ulnar border is formed by the tendon of the EPL. The deep branch of the radial artery and the tendinous insertion of the ECRL are along the floor of the snuffbox. Underneath these structures, the scaphoid and trapezium bones are found.

FIGURE 18-7 Anatomic snuffbox.
MOBILE ARCH SYSTEMS
The bones and soft tissues of the hand form a number of functional arches of the hand that provide a perfect balance of force distribution in an equiangular spiral. The arches of the hand, which are all concave palmarly, serve to enhance prehensile function. This prehensile function is best illustrated by the ability of the human hand to grasp an egg. A number of arches are commonly recognized:
 The transverse arch. The proximal, relatively immobile transverse arch is formed by the anterior (palmar) concavity of the carpal bones.6 This carpal arch, deepened by the anterior (palmar) projections of the scaphoid and trapezium laterally and the pisiform and hamate medially, should correspond to the concavity of the wrist. The distal transverse arch is more mobile and is defined by the alignment of the metacarpals. This arch allows the hand to adapt to objects held in the palm.11
The transverse arch. The proximal, relatively immobile transverse arch is formed by the anterior (palmar) concavity of the carpal bones.6 This carpal arch, deepened by the anterior (palmar) projections of the scaphoid and trapezium laterally and the pisiform and hamate medially, should correspond to the concavity of the wrist. The distal transverse arch is more mobile and is defined by the alignment of the metacarpals. This arch allows the hand to adapt to objects held in the palm.11
 The metacarpal arch. This arch, formed by the metacarpal heads, is a relatively mobile transverse arch.
The metacarpal arch. This arch, formed by the metacarpal heads, is a relatively mobile transverse arch.
 The longitudinal arch. This is specifically the arch of the middle finger and the arch of the index finger. The longitudinal arch, which contributes to powerful gripping, spans the hand lengthwise, with its keystone at the MCP joints.6
The longitudinal arch. This is specifically the arch of the middle finger and the arch of the index finger. The longitudinal arch, which contributes to powerful gripping, spans the hand lengthwise, with its keystone at the MCP joints.6
 The oblique arches. These arches are formed by the thumb in opposition to the other fingers.
The oblique arches. These arches are formed by the thumb in opposition to the other fingers.
Muscles of the Wrist and Forearm
The muscles of the forearm, wrist, and hand (Table 18-2) (Figs. 18-8 to 18-10) can be subdivided into 19 intrinsic muscles and 24 extrinsic muscles. The intrinsic muscles are located entirely within the hand; they arise and insert within the hand. The extrinsic muscles, whose muscle bellies lie proximal to the wrist, originate in the forearm and insert within the hand.4 The flexors, which are located in the anterior compartment, flex the wrist and digits while the extensors, located in the posterior compartment, extend the wrist and the digits.
TABLE 18-2 | Muscles of the Wrist and Hand: Their Actions and Nerve Supply |
Action | Muscles | Nerve Supply |
Wrist extension | Extensor carpi radialis longus Extensor carpi radialis brevis Extensor carpi ulnaris | Radial Posterior interosseous Posterior interosseous |
Wrist flexion | Flexor carpi radialis Flexor carpi ulnaris | Median Ulnar |
Ulnar deviation of wrist | Flexor carpi ulnaris Extensor carpi ulnaris | Ulnar Posterior interosseous |
Radial deviation of wrist | Flexor carpi radialis Extensor carpi radialis longus Abductor pollicis longus Extensor pollicis brevis | Median Radial Posterior interosseous Posterior interosseous |
Finger extension | Extensor digitorum communis Extensor indicis Extensor digiti minimi | Posterior interosseous Posterior interosseous Posterior interosseous |
Finger flexion | Flexor digitorum profundus | Anterior interosseous, lateral two digits Ulnar, medial two digits Median |
Flexor digitorum superficialis | Median | |
Lumbricals | First and second: median Third and fourth: ulnar | |
Interossei | Ulnar | |
Flexor digiti minimi | Ulnar | |
Abduction of fingers | Posterior (dorsal) interossei Abductor digiti minimi | Ulnar Ulnar |
Adduction of fingers | Anterior (palmar) interossei | Ulnar |
Thumb extension | Extensor pollicis longus Extensor pollicis brevis Abductor pollicis longus | Posterior interosseous Posterior interosseous Posterior interosseous |
Thumb flexion | Flexor pollicis brevis | Superficial head: median Deep head: ulnar |
Flexor pollicis longus | Anterior interosseous | |
Opponens pollicis | Median | |
Abduction of thumb | Abductor pollicis longus Abductor pollicis brevis | Posterior interosseous Median |
Adduction of thumb | Adductor pollicis | Ulnar |
Opposition of thumb and little finger | Opponens pollicis Flexor pollicis brevis Abductor pollicis brevis Opponens digiti minimi | Median Superficial head: median Median Ulnar |
ECU, Extensor carpi ulnaris; EPL, extensor pollicis longus; APB, abductor pollicis brevis; FCU, flexor carpi ulnaris; ADM, abductor digiti minimi; OP, opponens pollicis; FPB, flexor pollicis brevis; EPB, extensor pollicis brevis; ECRL, extensor carpi radialis longus; ECRB, extensor carpi radialis brevis; EDC, extensor digitorum communis; EDM, extensor digiti minimi; AP, Adductor Pollicis; FDM, flexor digiti minimi; ODM, Opponens Digiti Minimi. | ||
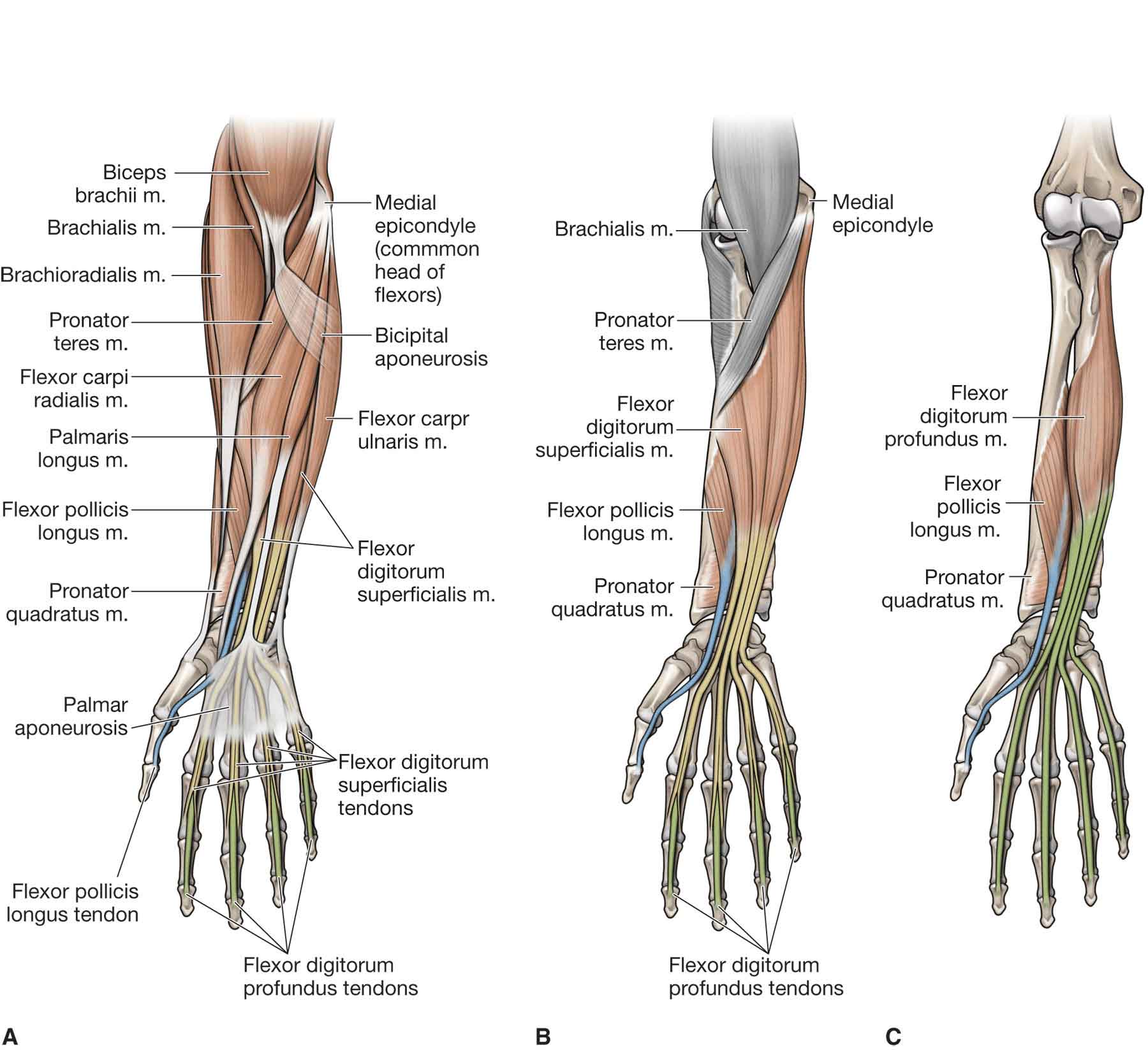
FIGURE 18-8 Muscles of the forearm, wrist, and hand. (Reproduced, with permission, from Chapter 32. Forearm. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
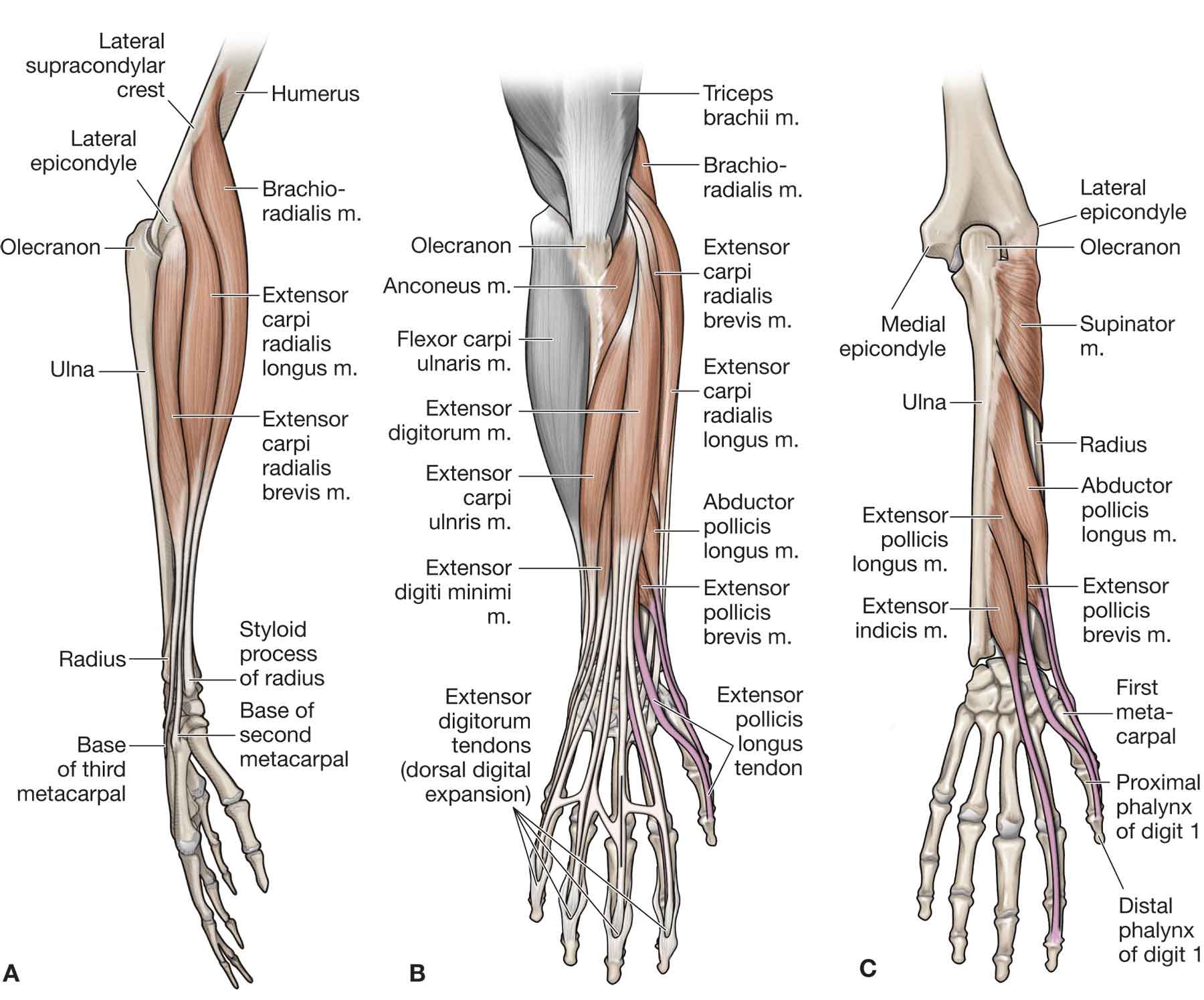
FIGURE 18-9 Muscles of the forearm, wrist, and hand. (Reproduced, with permission, from Chapter 32. Forearm. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
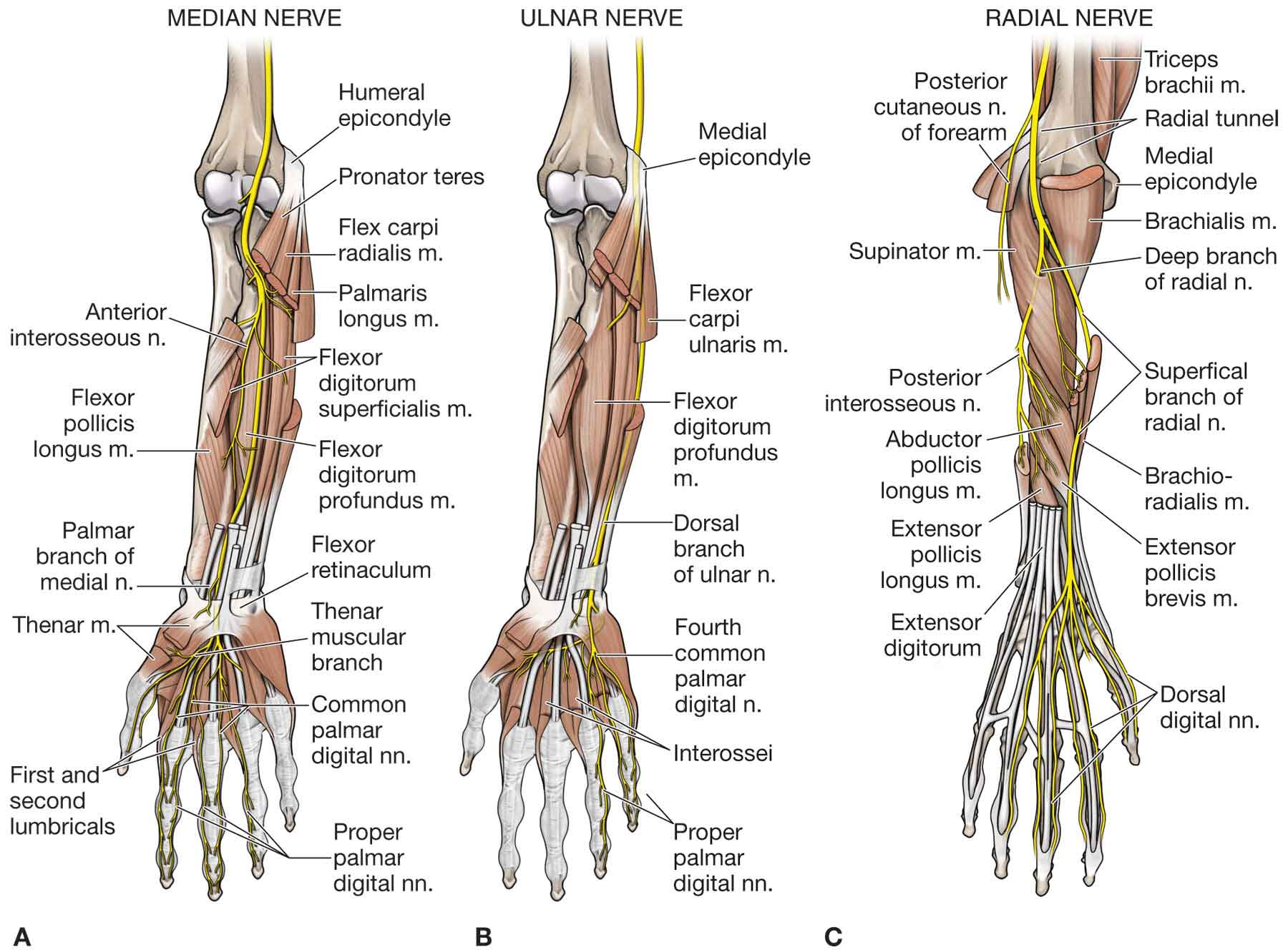
FIGURE 18-10 Muscles and nerve supply of the forearm, wrist, and hand. (Reproduced, with permission, from Chapter 32. Forearm. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The design of the extrinsic and intrinsic muscle groups provides for a large number of muscles to act on the hand without excessive bulkiness. The extrinsic tendons enhance wrist stability by balancing flexor and extensor forces and compressing the carpals.
The amount of tendon excursion determines the available range of motion at a joint. To calculate the amount of tendon excursion needed to produce a certain number of degrees of joint motion involves an appreciation of geometry. A circle’s radius equals approximately 1 radian (57.29 degrees). The mathematical radius, which is equivalent to the moment arm, represents the amount of tendon excursion required to move the joint through 1 radian.32 For example, if a joint’s moment arm is 10 mm, the tendon must glide 10 mm to move the joint 60 degrees (approximately 1 radian) or 5 mm to move the joint 30 degrees (1/2 radian).11
Anterior Compartment of the Forearm
Superficial Muscles
Pronator Teres. The pronator teres is described in Chapter 17.
Flexor Carpi Radialis. The FCR originates from the medial humeral epicondyle as part of the common flexor tendon. It inserts on the anterior surface and base of the second metacarpal, possibly providing a slip to the third metacarpal. The FCR is innervated by the median nerve and functions to flex and radially deviate the wrist.
Palmaris Longus. The inconsistent palmaris longus arises from the medial humeral epicondyle as part of the common flexor tendon and inserts on the transverse carpal ligament and anterior (palmar) aponeurosis. It receives its innervation from the median nerve. The function of the palmaris longus is to flex the wrist, and it may play a role in thumb abduction in some people.18
Flexor Carpi Ulnaris. The FCU arises from two heads. The humeral head arises from the medial humeral epicondyle as part of the common flexor tendon, while the ulnar head arises from the proximal portion of the subcutaneous border of the ulna. The FCU inserts directly onto the pisiform, the hamate via the pisohamate ligament, and onto the anterior surface of the base of the fifth metacarpal, via the pisometacarpal ligament. The FCU is innervated by the ulnar nerve and functions to flex and ulnarly deviate the wrist.
Intermediate Muscle
Flexor Digitorum Superficialis. The FDS has a three-headed origin. The humeral head arises from the medial humeral epicondyle as part of the common flexor tendon. The ulnar head arises from the coronoid process of the ulna. The radial head arises from the oblique line of the radius. The FDS inserts on the middle phalanx of the medial four digits via a split, “sling” tendon. This muscle is innervated by the median nerve and serves to flex the proximal and middle IP joints of the medial four digits and assist with elbow flexion and wrist flexion. The FDS possesses tendons that are capable of relatively independent action at each finger.
Deep Muscles
Flexor Pollicis Longus. The FPL has its origin on the ventral surface of the radius, medial border of the coronoid process of the ulna, and the adjacent interosseous membrane. It inserts on the distal phalanx of the thumb. The FPL is innervated by the anterior interosseous branch of the median nerve, and it functions to flex the thumb.
Flexor Digitorum Profundus. The FDP arises from the medial and anterior (ventral) surfaces of the proximal ulna, the adjacent interosseous membrane, and the deep fascia of the forearm. The FDP inserts on the base of the distal phalanges of the medial four digits. The FDP has a dual nerve supply: the medial two heads are supplied by the ulnar nerve while the lateral two heads are supplied by the anterior interosseous branch of the median nerve. The FDP functions to flex the DIP joints after the FDS flexes the second phalanges and assists with flexion of the wrist. The tendons of the FDS and FDP are held against the phalanges by a fibrous sheath. At strategic locations along the sheath, the previously mentioned five dense annular pulleys (designated A1, A2, A3, A4, and A5) and three thinner cruciform pulleys (designated C1, C2, and C3) prevent tendon bowstringing.33
Unlike the FDS tendons, the FDP tendons cannot act independently. To isolate the PIP joint flexor function of these two muscles, a clinician holds the adjoining finger(s) in extension while the patient attempts to flex the finger being tested. This anchors the profundus muscle of the finger being tested distally and allows the superficialis muscle to act alone at the PIP joint.
Tendinous connections between the FDP and the FPL are a common anatomic anomaly, which have been linked to a condition causing chronic forearm pain, called Linburg syndrome,34 although the association is by no means conclusive.35
Pronator Quadratus. The pronator quadratus arises from the anterior (ventral) surface and distal quarter of the ulna and inserts on the anterior (ventral) surface and distal quarter of the radius. The muscle functions to pronate the forearm, and it is innervated by the anterior interosseous branch of the median nerve. The pronator quadratus is well-designed biomechanically as an effective torque producer and a stabilizer of the DRUJ—its line of force is oriented almost perpendicular to the forearm’s axis of rotation.36
Posterior Compartment of the Forearm
Superficial Muscles
Extensor Carpi Radialis Longus. The ECRL takes its origin at the supracondylar ridge of the humerus about 4–5 cm proximal to the epicondyle, and the thickest part of the muscle is proximal to the elbow joint. The ECRL inserts on the base of the second metacarpal and functions to extend and radially deviate the wrist. It also plays a role in elbow flexion, losing a part of its wrist action when the elbow is flexed.23
Extensor Carpi Radialis Brevis. The ECRB arises from the common extensor tendon on the lateral epicondyle of the humerus (see Chapter 17) and from the radial collateral ligament. It inserts on the posterior surface of the base of the third metacarpal bone and receives its nerve supply from the posterior interosseous branch of the radial nerve. The muscle stretches across the radial head during forearm pronation, resulting in increased tensile stress when the forearm is pronated, the wrist is flexed, and the elbow is extended. The more medial location of the ECRB compared to the ECRL makes it the primary wrist extensor, but it has also a slight action of radial deviation.
ED and EDM. The ED arises from the lateral humeral epicondyle, part of the common extensor tendon while the EDM arises from a muscular slip from the ulnar aspect of the ED muscle. The ED inserts on the lateral and posterior (dorsal) aspect of the medial four digits, while the EDM inserts on the proximal phalanx of the fifth digit. Both muscles are innervated by the posterior interosseous branch of the radial nerve. While the ED functions to extend the medial four digits, the EDM extends the fifth digit.
Extensor Carpi Ulnaris. The ECU arises from the common extensor tendon on the lateral epicondyle of the humerus and the posterior border of the ulna. It inserts on the medial side of the base of the fifth metacarpal bone. It is innervated by the posterior interosseous branch of the radial nerve. The ECU is an extensor of the wrist in supination and primarily causes ulnar deviation of the wrist in pronation, working in synergy with the FCU to prevent radial deviation during pronation.23
Extension of the wrist is dependent on three muscles:
 ECRL
ECRL
 ECRB
ECRB
 ECU
ECU
The ECRB and ECRL are commonly considered to be similar muscles, but in fact they differ in many respects and have very different moment arms of extension.37 The ECRB, because of its origin on the epicondyle, is not affected by the position of the elbow, so that all of its action is on the wrist, making it the most effective extensor of the wrist (because it has the greatest tension and the most favorable moment arm).23 Taken together, both ECR tendons comprise about 10% of the muscle mass of the forearm and 76% of the muscle mass of the extensors of the wrist.38 The ECRL has longer muscular fibers, mostly at the level of the elbow. The ECRL only becomes a wrist extensor after radial deviation is balanced against the ulnar forces of the ECU.
The ECU, the antagonist of the EPL, has the weakest moment of extension, which becomes zero when the wrist is in complete pronation.
Deep Muscles
Abductor Pollicis Longus. The APL arises from the posterior (dorsal) surface of the proximal portion of the radius, ulna, and interosseous membrane and inserts on the anterior (ventral) surface of the base of the first metacarpal. The APL is innervated by the posterior interosseous branch of the radial nerve and functions in the abduction, extension, and external rotation of the first metacarpal.
Extensor Pollicis Brevis. The EPB arises from the posterior (dorsal) surface of the radius and interosseous membrane, just distal to the origin of the APL. It inserts on the posterior (dorsal) surface of the proximal phalanx of the thumb via the extensor expansion. The EPB is innervated by the posterior interosseous branch of the radial nerve and functions to extend the proximal phalanx of the thumb.
Extensor Pollicis Longus. The EPL arises from the posterior (dorsal) surface of the midportion of the ulna and interosseous membrane. It inserts on the posterior (dorsal) surface of the distal phalanx of the thumb via the extensor expansion. The EPL is innervated by the posterior interosseous branch of the radial nerve. It functions in the extension of the distal phalanx of the thumb and is thus involved in the extension of the middle phalanx and the MCP joint of the thumb.
Extensor Indicis. The EI arises from the posterior (dorsal) surface of the ulna, distal to the other deep muscles, and inserts on the extensor expansion of the index finger. It is innervated by the posterior interosseous branch of the radial nerve and is involved in the extension of the proximal phalanx of the index finger.
Muscles of the Hand
The muscles of the hand (Fig. 18-11) are those that originate and insert within the hand and are responsible for fine finger movements.
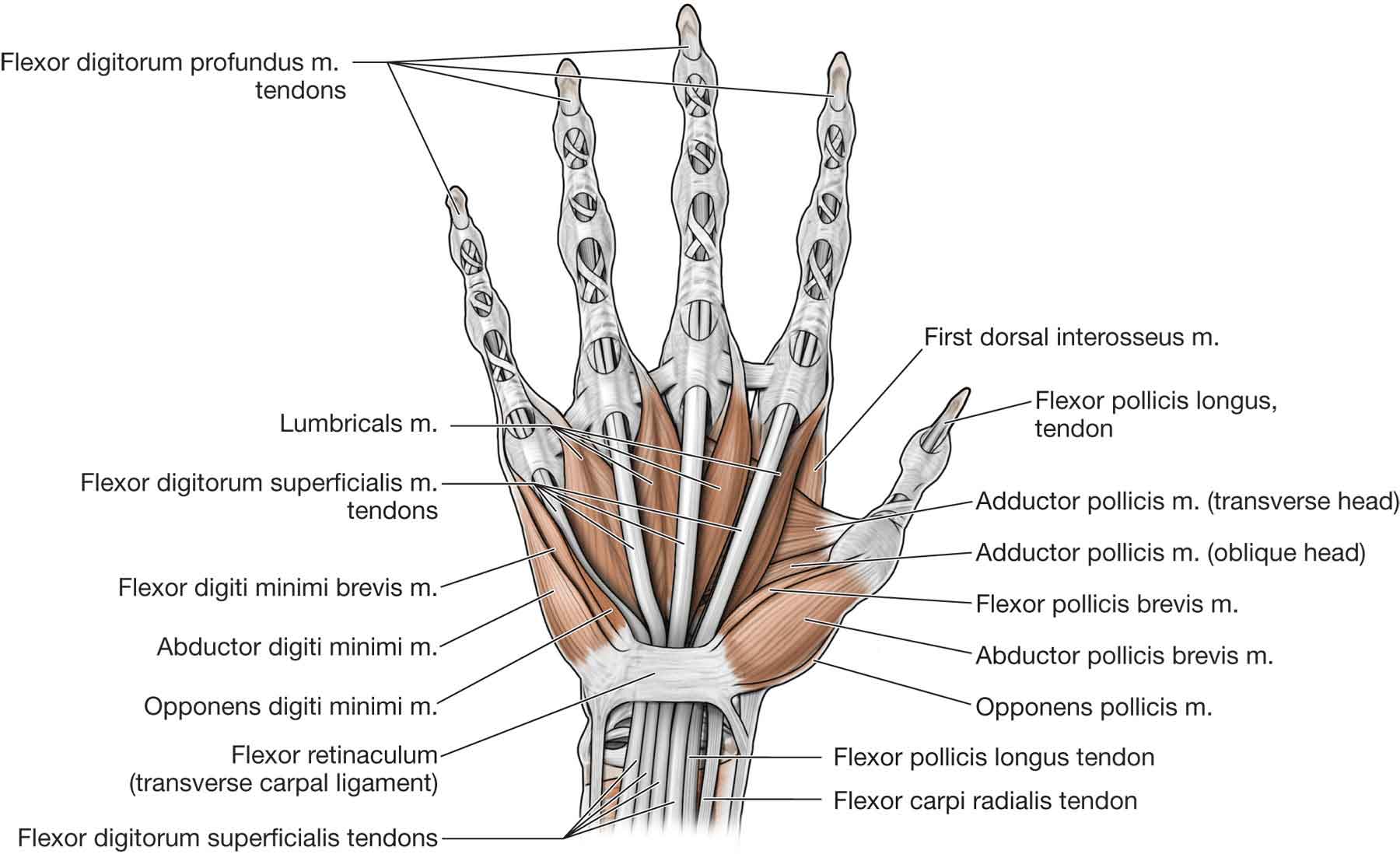
FIGURE 18-11 Muscles of the hand. (Reproduced, with permission, from Chapter 33. Hand. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Short Muscles of the Thumb
Abductor Pollicis Brevis. The APB arises from the flexor retinaculum and the trapezium bone and inserts on the radial aspect of the proximal phalanx of the thumb. It is innervated by the median nerve and functions to abduct the first metacarpal and proximal phalanx of the thumb.
Flexor Pollicis Brevis. The FPB arises from two heads. The superficial head arises from the flexor retinaculum and the trapezium bone while the deep head arises from the floor of the carpal canal. The FPB inserts on the base of the proximal phalanx of the thumb. The superficial head receives its innervation from the median nerve while the deep head is innervated by the ulnar nerve. The FPB functions to flex the proximal phalanx of the thumb.
Opponens Pollicis. The OP arises from the flexor retinaculum and the trapezium bone and inserts along the radial surface of the first metacarpal. The OP is innervated by the median nerve and functions to flex, rotate, and slightly abduct the first metacarpal across the palm to allow for the opposition with each of the other digits.
Adductor Pollicis. The adductor pollicis (AP) arises from two heads. The transverse head originates from the ventral surface of the shaft of the third metacarpal, while the oblique head originates from the trapezium, trapezoid, and capitate bones, and the base of the second and third metacarpal bone. The AP inserts on the ulnar side of the base of the proximal phalanx of the thumb and is innervated by the deep branch of the ulnar nerve. The AP functions to adduct the thumb and aids in thumb opposition.
Short Muscles of the Fifth Digit
Abductor Digiti Minimi. The ADM arises from the pisiform bone and the tendon of the FCU. It inserts on the ulnar aspect of the base of the proximal phalanx of the fifth digit, together with the flexor digiti minimi (FDM) brevis. It is innervated by the deep branch of the ulnar nerve and functions to abduct the fifth digit.
Flexor Digiti Minimi. The FDM originates from the flexor retinaculum and the hook of the hamate bone. It inserts on the ulnar aspect of the base of the proximal phalanx of the fifth digit, together with the ADM. It is innervated by the deep branch of the ulnar nerve and functions to flex the proximal phalanx of the fifth digit.
Deep branches of the ulnar artery and nerve enter the thenar mass and course into the deep region of the hand by passing between the ADM and the FDM.
Opponens Digiti Minimi. The opponens digiti minimi (ODM) arises from the flexor retinaculum and the hook of the hamate bone and inserts on the ulnar border of the shaft of the fifth metacarpal bone. It is innervated by the deep branch of the ulnar nerve and functions to provide a small amount of flexion and external rotation of the fifth digit.
Interosseous Muscles of the Hand
The interossei muscles of the hand are divided by anatomy and function into anterior (palmar) and posterior (dorsal) interossei.
Anterior (Palmar) Interossei
The three anterior (palmar) interossei have a variety of origins and insertions. The first interosseous originates from the ulnar surface of the second metacarpal bone and inserts on the ulnar side of the proximal phalanx of the second digit. The second anterior (palmar) interosseous arises from the radial side of the fourth metacarpal bone and inserts on the radial side of the proximal phalanx of the fourth digit. The third anterior (palmar) interosseous originates from the radial side of the fifth metacarpal bone and inserts on the radial side of the proximal phalanx of the fifth digit. The anterior (palmar) interossei are innervated by the deep branch of the ulnar nerve, and each muscle functions to adduct the digit to which it is attached toward the middle digit. The anterior (palmar) interossei also function to extend the distal and then the middle phalanges.
Posterior (Dorsal) Interossei
The four posterior (dorsal) interossei have a similarly varied origin and insertion as their anterior (palmar) counterparts. The posterior (dorsal) interossei originate via two heads from adjacent sides of the metacarpal bones. The first posterior (dorsal) interosseous muscle inserts into the radial side of the proximal phalanx of the second digit. The second inserts into the radial side of the proximal phalanx of the third digit. The third inserts into the ulnar side of the proximal phalanx of the third digit and the fourth inserts into the ulnar side of the proximal phalanx of the fourth digit. The posterior (dorsal) interossei receive their innervation from the deep branch of the ulnar nerve. The posterior (dorsal) interossei abduct the index, middle and ring fingers from the midline of the hand.
Lumbricals
The lumbrical muscles are usually four small intrinsic muscles of the hand that originate from the FDP tendons and insert into the posterior (dorsal) hood apparatus. Occasionally, more than four lumbricals are found in one hand.39
During contraction, they pull the FDP tendons distally, thus possessing the unique ability to relax their own antagonist.6 They function to perform the motion of IP joint extension with the MCP joint held in extension and can assist in MCP flexion.23
The lumbrical muscles also serve an important role in the proprioception of the hand, providing feedback about the position and movement of the hand and finger joints.6
In instances of lumbrical spasm or contracture, attempts to flex the fingers via the profundus result in transmission of force through the lumbricals into the extensor apparatus, producing extension rather than flexion.6 A “lumbrical plus” deformity occurs if there is excessive lumbrical force, or if there is imbalance of opposing forces, which produces exaggerated lumbrical action (i.e., MCP joint flexion and IP joint extension).6
The lumbricals have dual innervation. Lumbricals I and II are innervated typically by the median nerve while the third and fourth lumbricals are innervated by the ulnar nerve.
Neurology
The three peripheral nerves that supply the skin and muscles of the wrist and hand include the median, ulnar, and radial nerves (Fig. 18-12).
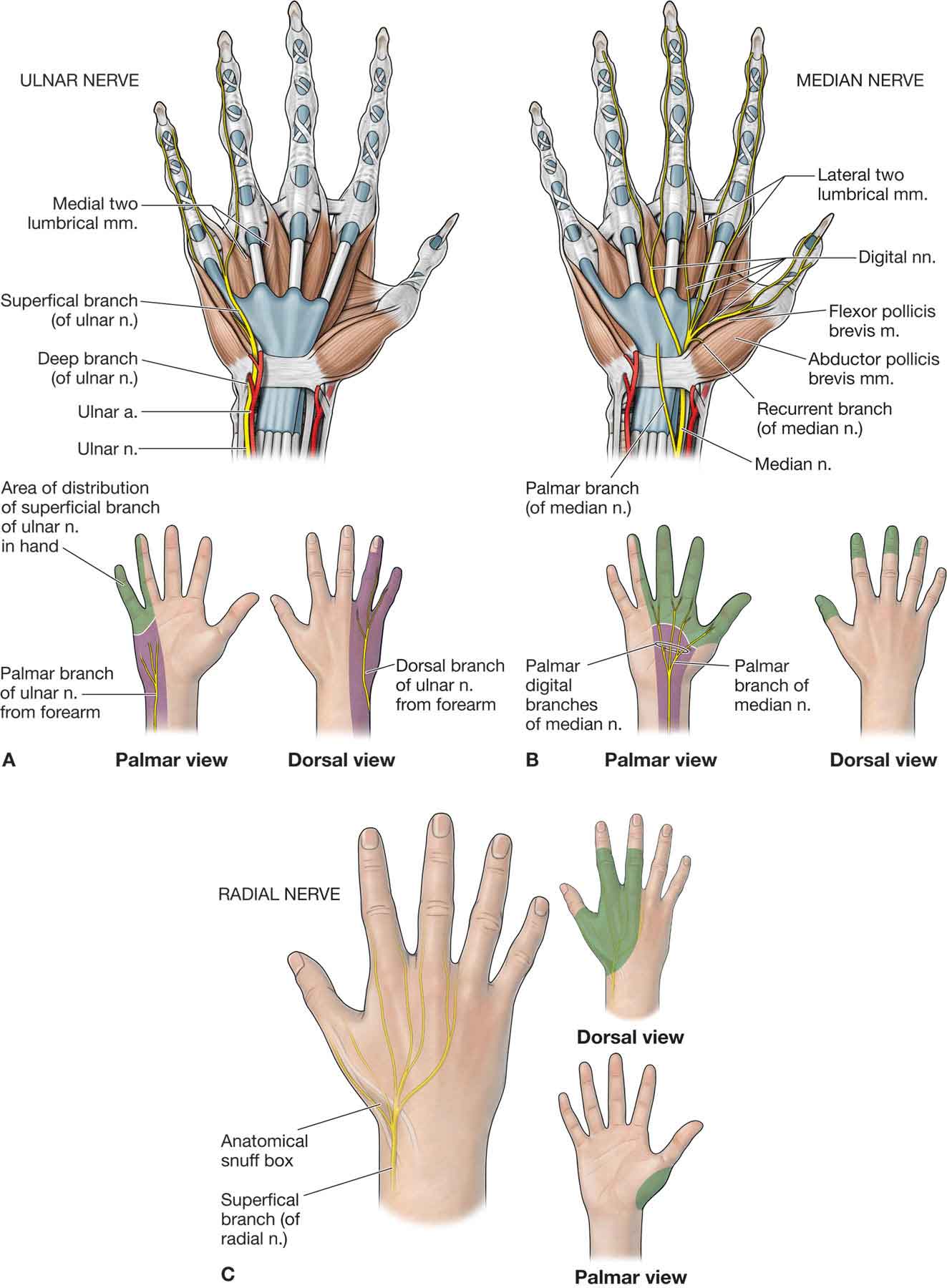
FIGURE 18-12 Nerves of the hand. (Reproduced, with permission, from Chapter 33. Hand. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Median Nerve
The median nerve enters the forearm by coursing anteriorly through the medial aspect of the cubital fossa and passing deep to the lacertus fibrosis, between the heads of the pronator teres muscle. Below the elbow, muscular branches leave the nerve and innervate the FCR, palmaris longus, and pronator teres muscles. The anterior interosseous branch innervates the pronator quadratus, FPL, and the FDP to the index finger and middle fingers and sometimes the ring finger.
Approximately 8 cm proximal to the wrist, the median nerve gives off a sensory branch, the anterior (palmar) cutaneous nerve that passes superficial to the flexor retinaculum and remains outside the carpal tunnel. This nerve innervates the skin of the central aspect of the palm, over the thenar eminence. The rest of the median nerve passes distally to the wrist, where it enters the carpal tunnel, which passes deep to the flexor retinaculum.
The nerve enters the hand through the carpal tunnel, deep to the tendon of the palmaris longus and in between the tendons of the FPL and FDS (the more radial of the two). From this point, the nerve divides into two branches: a motor branch which passes posterior (dorsal) to the flexor retinaculum and a sensory branch.
Motor Branch. This short branch enters the thenar eminence, where it usually supplies the APB and OP muscles, the FPB (occasionally), and the first and second lumbrical muscles.
Sensory Branch. The sensory anterior (palmar) digital branch innervates the anterior (palmar) surface and posterior (dorsal) aspect of the distal phalanges of the thumb, second and third fingers, and the radial half of the forefinger.
A number of median nerve entrapment syndromes exist (refer to “Peripheral Nerve Entrapment”), each with their own clinical features and functional implications. For example, entrapment of the median nerve in the carpal tunnel may result in numbness, pain, or paresthesia of the fingers and thumb and may severely hinder a patient’s ability to perform precision maneuvers due to loss of critical sensory and motor function in the thumb, index, and middle fingers.
Ulnar Nerve
The ulnar nerve has been referred to as the nerve of fine movements of the hand. The ulnar nerve originates from the inferior roots of the brachial plexus (C8–T1). Two branches of the ulnar nerve arise in the midforearm:
 The anterior (palmar) cutaneous branch. The anterior (palmar) cutaneous branch supplies a portion of the skin over the hypothenar eminence.
The anterior (palmar) cutaneous branch. The anterior (palmar) cutaneous branch supplies a portion of the skin over the hypothenar eminence.
 The posterior (dorsal) cutaneous branch. About 8–10 cm proximal to the ulnar styloid process, the posterior (dorsal) cutaneous branch of the ulnar nerve splits from the main trunk. The posterior (dorsal) cutaneous branch terminates into two posterior (dorsal) digital branches that supply sensation to the posterior (dorsal) and ulnar aspect of the middle phalanx of the ring and little fingers.40
The posterior (dorsal) cutaneous branch. About 8–10 cm proximal to the ulnar styloid process, the posterior (dorsal) cutaneous branch of the ulnar nerve splits from the main trunk. The posterior (dorsal) cutaneous branch terminates into two posterior (dorsal) digital branches that supply sensation to the posterior (dorsal) and ulnar aspect of the middle phalanx of the ring and little fingers.40
Before reaching the wrist, the ulnar nerve branches to innervate the FDP and the FCU.
At the wrist, the ulnar nerve emerges just lateral to the tendon of the FCU as it passes superficial to the flexor retinaculum. The ulnar nerve passes into the hand via the tunnel of Guyon, where it divides into its superficial and deep, terminal branches. The deep (motor) branch supplies the FDM, ADM, ODM, AP, palmaris brevis, third and fourth lumbricals, deep head of the FPB, and the interossei. The superficial branch, which is primarily sensory with the exception of its innervation to the palmaris brevis, divides into three branches.40 The first of these three branches is a sensory branch to the ulnar aspect of the little finger, and the second is a sensory branch to the central ulnar anterior (palmar) area. The third branch often referred to as the common digital nerve, innervates the fourth intermetacarpal space. The common digital nerve further divides into two proper digital nerves supplying the ulnar portion of the ring finger and the radial portion of the little finger.40
A number of ulnar nerve entrapment syndromes exist (refer to “Peripheral Nerve Entrapment”), each with their own clinical features and functional implications.
Radial Nerve
As the radial nerve enters the cubital fossa, it typically splits into a superficial and deep branch. The superficial branch typically courses distally along the lateral border of the forearm under cover of the brachioradialis muscle and tendon. At the wrist, this branch divides into four to five digital branches, which provide cutaneous and articular innervation. The cutaneous innervation includes the lateral two-thirds of the dorsum of the hand and the posterior (dorsal) lateral 2½ fingers to the proximal phalanx.
All of the motor branches of the radial nerve are located in the forearm. The deep branch (posterior interosseous nerve) typically penetrates the anterior (ventral) surface of, and passes through the supinator muscle. It reaches the deep region of the posterior forearm by passing through the arcade of Fröhse. The nerve courses subcutaneously from the midportion of the forearm to an area adjacent to the styloid process of the radius and terminates on the posterior aspect of the wrist.
