Clinical decision making for the management of foot deformities in children with cerebral palsy is based on the collection and integration of data from 5 sources: the clinical history, physical examination, plain radiographs, observational gait analysis, and quantitative gait analysis (which includes kinematic/kinetic analyses, dynamic electromyography, and dynamic pedobarography). The 3 most common foot segmental malalignments in children with CP are equinus, equinoplanovalgus, and equinocavovarus. The 2 most common associated deformities are ankle valgus and hallux valgus. Foot and ankle deformities caused by dynamic overactivity and imbalance of muscles are best treated with pharmacologic or neurosurgical interventions designed to manage muscle tone and spasticity, or muscle tendon unit transfers. Deformities caused by fixed or myostatic soft tissue imbalance without fixed skeletal malalignment are best treated with muscle tendon unit lengthening surgery. Deformities characterized by structural skeletal malalignment associated with fixed or myostatic soft tissue imbalance are best treated with a combination of soft tissue and skeletal surgeries.
Foot and ankle problems are common in children with cerebral palsy (CP). In ambulatory children, the efficiency of gait may be compromised. Nonambulatory children may have problems with orthotic and shoe wear. Surgical interventions are frequently performed to address these issues. This article presents the current paradigm for clinical decision making for surgery about the foot and ankle in children with CP. This approach is built on a standardized assessment and classification of disruption of foot alignment and function in these children. Surgical treatment principles and options are considered, and preferred surgical techniques for the most common foot and ankle problems in children with CP are described.
Clinical decision making
Clinical decision making for the management of foot deformities in children with CP can be standardized by the use of a diagnostic matrix ( Table 1 ). This paradigm is based on the collection and integration of data from 5 sources: the clinical history, physical examination, plain radiographs, observational gait analysis, and quantitative gait analysis (which includes kinematic/kinetic analyses, dynamic electromyography [EMG], and dynamic pedobarography).
| Source | Information |
|---|---|
| Clinical history |
|
| Physical examination |
|
| Radiographic examination |
|
| Observational gait analysis |
|
| Quantitative gait analysis |
|
Clinical History
The most common complaints related to foot deformity in children with CP are pain with ambulation, shoe wear, or use of orthoses; tripping because of poor clearance in swing phase; and in-toeing or out-toeing.
Physical Examination
Foot segmental alignment is assessed in both weight-bearing and non–weight-bearing conditions. Manual examination is performed to determine intra- and intersegmental flexibility, active and passive range of motion, and individual muscle strength and selective control. The static standing alignment of the foot is best assessed from the front, behind, and both sides. The plantar and medial margins of the foot should be examined for the presence of inadequate or excessive skin callous formation, which indicates disrupted loading patterns or problems with shoe or orthotic wear.
Plain Radiographs
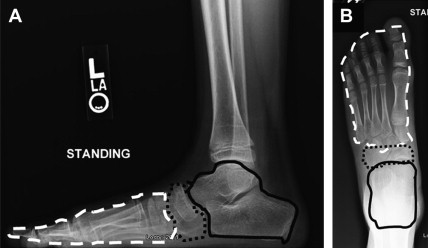
Standardized radiographic analysis of foot deformity in children with CP should include 3 weight-bearing views: standing anteroposterior (AP) and lateral views of the foot, and AP view of the ankle. Foot deformities are best identified and classified by dividing the foot into 3 segments and 2 columns, then determining the relative alignment of each segment and the relative length of each column ( Fig. 1 ). A comprehensive technique of quantitative segmental analysis of the ankle and foot, with normative values, has been developed, based on qualitative techniques derived from the foot model originally developed by Inman and colleagues. This approach uses 10 radiographic measurements to determine the alignment of the 3 segments and the lengths of the 2 columns of the ankle and foot. Individual measures of segmental alignment that are beyond 1 standard deviation from the normal mean value are considered to be abnormal and can be used to describe malalignment patterns.
Observational Gait Analysis
Ambulation is best observed from multiple viewpoints in the coronal and sagittal planes. This observation is most effectively achieved by having the child walk toward, away from, and past the examiner. The subject should be barefoot and wearing short pants, which allows for adequate visualization of the thigh, knee, lower leg, ankle, and foot. The key events of the gait cycle related to dynamic foot function that may be appreciated on observational gait analysis include foot position at initial contact (heel strike, flat foot, or toe strike), foot alignment in midstance (varus or valgus in the coronal plane; internal or external in the transverse plane, described as the foot progression angle), foot alignment at toe-off (varus or valgus in the coronal plane, dorsiflexed or plantarflexed in the sagittal plane), and foot clearance in swing phase.
Quantitative Gait Analysis
The calculation of foot and ankle kinematics and kinetics involves modeling assumptions and approximations concerning the relationship between the skin markers and the underlying skeletal anatomy. The standard ankle and foot model most commonly used in clinical gait analysis was developed in the early 1980s, uses markers at the malleoli and forefoot, and considers the foot as a single segment. It is assumed that the foot segment is rigid from the hindfoot to the forefoot. Ankle motion in the sagittal plane is calculated from the location of the foot axis relative to the tibial axis. Any movement between the 3 segments of the foot (eg, hindfoot to midfoot, midfoot to forefoot) that occurs between the malleolar and forefoot markers is captured by this simple foot model and described as ankle motion. Significant measurement artifact occurs when the normal foot segmental alignment is disrupted (eg, equinoplanovalgus foot malalignment in children with CP). This artifact creates apparent discrepancies within the diagnostic matrix between the data derived from the physical examination, observational gait analysis, and quantitative gait analysis. Failure to appreciate the causes for these apparent discrepancies may result in confusion for clinicians and compromise clinical decision making.
Technological improvements have allowed for the development of more sophisticated, multisegment foot models that more accurately approximate the complex anatomy and biomechanics of the foot. However, these models are difficult to apply to children with CP, because of small foot size (intermarker distances are reduced beyond the ranges of resolution) and deformity (segmental malalignment obscures anatomic landmarks and compromises accurate marker placement). A foot model that is useful for clinical decision making for children with CP, with respect to orthotic prescriptions, surgical planning, and postintervention outcome assessment, is currently being developed.
Dynamic EMG is most relevant in the evaluation of specific foot deformities such as equinocavovarus segmental malalignment. The use of surface and fine-wire EMG provides information on the timing of muscle activity during the gait cycle. This is most helpful in sorting out the relative activity of the tibialis anterior and posterior muscles in both stance and swing phases. This information facilitates clinical decision with respect to the selection of a particular muscle tendon unit for lengthening or transfer.
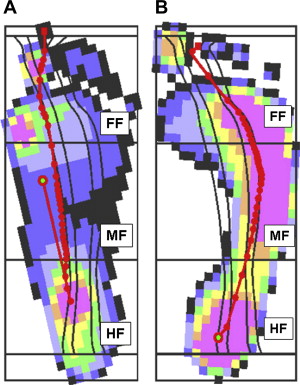
Dynamic pedobarography measures the spatial and temporal distribution of force over the plantar aspect of the foot during the stance phase of the gait cycle. Pedobarography provides quantitative information regarding dynamic foot function, consisting of foot contact patterns, pressure distribution and magnitude, and progression of the center of pressure. In children with CP, foot function during gait is disrupted by several common patterns of skeletal segmental malalignment. All 3 rockers in stance phase may be affected. This biomechanical disruption has been termed lever arm deficiency, and is best characterized by the center of pressure progression (COPP) relative to the foot. Normative values for the COPP in children have been established. Deviation in the location and duration of the COPP relative to the segments of the foot can be used to describe common abnormal loading patterns ( Fig. 2 ). Displacement of the COPP medially in a particular segment of the foot describes a valgus loading pattern, which is usually the consequence of an everted, abducted, or pronated segmental malalignment of the foot segment. Displacement of the COPP laterally in a particular segment of the foot describes a varus loading pattern, which is usually the consequence of an inverted, adducted, or supinated segmental malalignment of the foot segment. Prolonged duration of the COPP in the forefoot segment describes an equinus foot loading pattern. Prolonged duration of the COPP in the hindfoot segment describes a calcaneus loading pattern. This standardized approach to the determination of foot loading patterns can be used to characterize abnormal foot loading patterns, assist in clinical decision making, and contribute to the assessment of outcome following a variety of interventions.
Disruption of foot function in children with CP
Foot deformities in children with CP are usually the result of a dynamic imbalance between the extrinsic muscles of the lower leg that control segmental foot and ankle alignment. This imbalance may be a consequence of spasticity, disrupted motor control, and/or impaired balance function. Typically, the ankle plantar flexor muscles are overactive, and the ankle dorsiflexor muscles are ineffective. Variable imbalance patterns may be seen between the foot and ankle supination and pronation muscle groups. These motor imbalances result in 3 common coupled foot and ankle segmental malalignment patterns in children with spastic type CP. Equinus is characterized by excessive plantar flexion of the hindfoot relative to the ankle, with normal midfoot and forefoot alignment. Equinoplanovalgus is characterized by equinus deformity of the hindfoot, coupled with pronation deformities of the midfoot and forefoot. The lateral column of the foot is functionally and/or structurally shorter than the medial column. Ankle valgus and hallux valgus deformities are frequently seen in association with equinoplanovalgus foot segmental malalignment. Equinocavovarus is characterized by equinus deformity of the hindfoot, coupled with supination deformity of the midfoot and variable malalignment of the forefoot. The lateral column is functionally and/or structurally longer than the medial column. Compensatory ankle valgus deformity may be seen in association with equinocavovarus foot segmental malalignment. Other, more complex, or uncoupled segmental alignments may occur, but are less common. These common segmental malalignments of the foot and ankle are usually supple and correctible on manipulation in younger children with less severe CP. However, with increasing age and growth, the muscles develop fixed shortening or myostatic deformity, the bones develop permanent structural accommodations to the malalignment pattern, and the foot and ankle deformities become rigid and uncorrectable on manipulation.
Foot and ankle segmental malalignment may disrupt function during both the stance and swing phases of the gait cycle. In all 3 segmental malalignment patterns, heel strike at initial contact does not occur, disrupting the first or hindfoot rocker and shock absorption function in loading response. Equinus and equinocavovarus malalignment patterns disrupt the second or ankle rocker by blocking ankle dorsiflexion, compromising stability function in midstance. Equinoplanovalgus malalignment maintains the mid- and forefoot segments in an unlocked alignment, compromising stability function in midstance, which may result in excessive loading of the plantar, medial portion of the midfoot. All 3 segmental malalignments may compromise the ability of the ankle plantar flexor muscles to generate an adequate internal plantar flexion moment during third or forefoot rocker. The hindfoot malalignment associated with equinus and equinocavovarus malalignment patterns shortens the length of the plantar flexor muscles, compromising their ability to generate tension, as described by the length-tension curve for skeletal muscle. With equinoplanovalgus, the moment-generating capacity of the ankle plantarflexor muscles is further compromised by the malalignment of mid-and forefoot segments, which effectively shortens the lever arm available to this muscle group during the third or forefoot rocker. In addition, increased external tibial torsion, which may be associated with equinoplanovalgus segmental malalignment, may contribute to an external foot progression angle, further compromising the lever arm available to the ankle plantar flexor muscles in terminal stance. All 3 segmental malalignment patterns of the foot and ankle may inhibit ankle dorsiflexion in swing phase, compromising clearance in midswing and proper positioning of the foot and ankle in terminal swing.
Disruption of foot function in children with CP
Foot deformities in children with CP are usually the result of a dynamic imbalance between the extrinsic muscles of the lower leg that control segmental foot and ankle alignment. This imbalance may be a consequence of spasticity, disrupted motor control, and/or impaired balance function. Typically, the ankle plantar flexor muscles are overactive, and the ankle dorsiflexor muscles are ineffective. Variable imbalance patterns may be seen between the foot and ankle supination and pronation muscle groups. These motor imbalances result in 3 common coupled foot and ankle segmental malalignment patterns in children with spastic type CP. Equinus is characterized by excessive plantar flexion of the hindfoot relative to the ankle, with normal midfoot and forefoot alignment. Equinoplanovalgus is characterized by equinus deformity of the hindfoot, coupled with pronation deformities of the midfoot and forefoot. The lateral column of the foot is functionally and/or structurally shorter than the medial column. Ankle valgus and hallux valgus deformities are frequently seen in association with equinoplanovalgus foot segmental malalignment. Equinocavovarus is characterized by equinus deformity of the hindfoot, coupled with supination deformity of the midfoot and variable malalignment of the forefoot. The lateral column is functionally and/or structurally longer than the medial column. Compensatory ankle valgus deformity may be seen in association with equinocavovarus foot segmental malalignment. Other, more complex, or uncoupled segmental alignments may occur, but are less common. These common segmental malalignments of the foot and ankle are usually supple and correctible on manipulation in younger children with less severe CP. However, with increasing age and growth, the muscles develop fixed shortening or myostatic deformity, the bones develop permanent structural accommodations to the malalignment pattern, and the foot and ankle deformities become rigid and uncorrectable on manipulation.
Foot and ankle segmental malalignment may disrupt function during both the stance and swing phases of the gait cycle. In all 3 segmental malalignment patterns, heel strike at initial contact does not occur, disrupting the first or hindfoot rocker and shock absorption function in loading response. Equinus and equinocavovarus malalignment patterns disrupt the second or ankle rocker by blocking ankle dorsiflexion, compromising stability function in midstance. Equinoplanovalgus malalignment maintains the mid- and forefoot segments in an unlocked alignment, compromising stability function in midstance, which may result in excessive loading of the plantar, medial portion of the midfoot. All 3 segmental malalignments may compromise the ability of the ankle plantar flexor muscles to generate an adequate internal plantar flexion moment during third or forefoot rocker. The hindfoot malalignment associated with equinus and equinocavovarus malalignment patterns shortens the length of the plantar flexor muscles, compromising their ability to generate tension, as described by the length-tension curve for skeletal muscle. With equinoplanovalgus, the moment-generating capacity of the ankle plantarflexor muscles is further compromised by the malalignment of mid-and forefoot segments, which effectively shortens the lever arm available to this muscle group during the third or forefoot rocker. In addition, increased external tibial torsion, which may be associated with equinoplanovalgus segmental malalignment, may contribute to an external foot progression angle, further compromising the lever arm available to the ankle plantar flexor muscles in terminal stance. All 3 segmental malalignment patterns of the foot and ankle may inhibit ankle dorsiflexion in swing phase, compromising clearance in midswing and proper positioning of the foot and ankle in terminal swing.
Surgical treatment: principles and options
Treatment Goals
Interventions to correct foot deformities in children with CP may be selected to improve function and cosmesis. These goals may be achieved by surgeries that are designed to improve foot shape. It is presumed that improved foot shape following soft tissue and skeletal surgery can restore both the stability function of the foot during the second or ankle rocker in midstance and the skeletal lever arm function of the foot during the third or forefoot rocker in terminal stance. However, increased foot stiffness associated with many skeletal surgical procedures (eg, arthrodesis) used to improve foot shape may compromise the shock absorption function of the foot during the first or ankle rocker in loading response. Cosmetic improvements following foot surgery are related to improved visual assessment of static standing foot alignment (particularly restoration of the medial longitudinal arch and toe alignment) and improved foot progression angle during stance phase.
Pain may be associated with foot deformities in children with CP and is usually the consequence of poor alignment and instability during stance phase. Equinoplanovalgus segmental malalignment of the foot may cause excessive loading of the medial midfoot during the second or ankle rocker in midstance, leading to the development of painful callosities that may compromise orthotic and shoe wear. Equinocavovarus segmental malalignment of the foot may cause excessive loading of the lateral mid- and forefoot segments, resulting in instability during the second or ankle rocker in midstance and during the third or forefoot rocker in terminal stance, which may lead to frequent inversion injuries of the ankle and hindfoot. It is presumed that surgically improved foot shape can correct pain by improving foot loading and stability in stance phase. Younger children with CP may tolerate mild or moderate foot deformities, with little complaint of pain or sense of impairment. However, such deformities may be poorly tolerated in teenage and adult life, where the magnitude of the abnormal loading is much greater (because of increased body mass), and the cumulative effect over time results in premature degenerative changes of the joints of the foot and ankle. It is presumed that surgery to improve foot shape in childhood will improve the loading of the foot and decrease the possibility of early degenerative arthritis in adulthood.
Levels of Deformity
Foot deformities in children with CP are sequential and progressive with growth and development. These deformities may be classified into 3 levels ( Table 2 ). Level I deformities are the characterized by dynamic soft tissue imbalance. Skeletal anatomy is normal. Level II deformities are characterized by fixed or myostatic soft tissue imbalance. Skeletal segmental malalignments are flexible and correctable on manipulation. Level III deformities are characterized by structural skeletal deformities that are usually associated with fixed or myostatic soft tissue imbalance.
| Level of Deformity | Treatment Options | ||
|---|---|---|---|
| Pharmacologic/Neurosurgery | Muscle Tendon Surgeries | Skeletal Surgeries | |
| Dynamic soft tissue imbalance, no skeletal deformities |
|
|
|
| Fixed soft tissue imbalance, no skeletal deformities |
|
|
|
| Fixed soft tissue imbalance, with skeletal deformities |
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








