The Elbow
18.1 Anatomy
Gail A. Shafer-Crane
William M. Falls
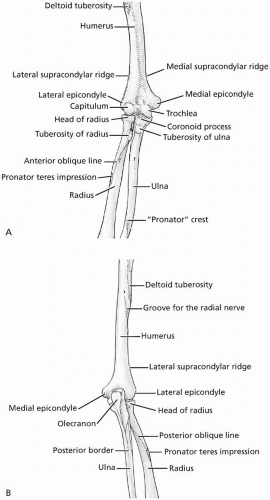
Three bones participate in the elbow joint, the humerus, radius, and ulna. The humerus widens and flattens as it approaches the elbow joint, where it articulates with the long bones of the forearm, the radius and ulna. The lateral and medial epicondyles are formed as the humerus broadens proximal to the elbow. The distal humerus is rounded into two articular surfaces, the trochlea and capitulum. The medial surface forms the cylindrical trochlea, and the lateral surface is the rounded capitulum. The ulnar notch, or groove for the ulnar nerve, is a hollow trench formed along the posterior aspect of the medial epicondyle. Flexion and extension of the elbow are permitted at the humeroulnar joint. The humeroradial joint increases elbow stability while permitting flexion and extension (Fig. 18.1.1A and B). Pronation and supination of the forearm occur at the proximal radioulnar joint (PRUJ). Anatomy of the elbow is presented in detail in major anatomic textbooks (1,2,3,4,5,6,7,8).
The most stable joint of the elbow is the humeroulnar joint. The distal humerus is a cylindrical trochlea that fits exactly into the trochlear notch of the ulna. The coronoid process of the volar ulna deepens the trochlear notch and reinforces the articulation. The olecranon process is a rectangular extension of the ulna that fits into a hollow on the posterior humerus, the olecranon fossa, during full extension of the elbow. The precise fit between these articular surfaces permits smooth extension and flexion of the elbow while preventing extreme hyperextension and dislocation. Slight hyperextension and a lateral carrying angle vary between the genders. Women tend to have up to 15 degrees of hyperextension with a carrying angle of 15 to 30 degrees. Men often do not demonstrate hyperextension of the elbow, and the carrying angle is usually from 10 to 15 degrees.
A fibrous capsule encloses this articulation. Folds form in the capsule as the attachments of the olecranon and coronoid processes stretch and slacken as the ulna rotates around the humeral trochlea. Fat pads partially fill the olecranon and coronoid fossae of the humerus.
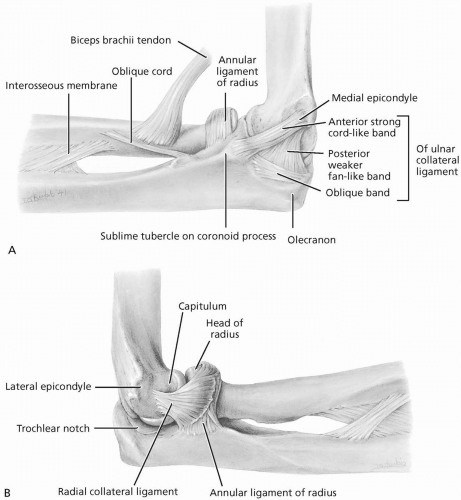
The ulnar (medial) collateral ligament forms the medial joint capsule. This broad ligament is divided into three bands: the anterior, posterior, and oblique. The anterior band is cordlike with a proximal attachment of the medial epicondyle and the distal attachment on the tubercle of the coronoid process. This is the most important medial stabilizer of the elbow. The posterior band is triangular, with the narrow, proximal attachment along the inferior medial epicondyle deep to the anterior band, and the broad distal attachment along the olecranon process. The oblique band is superficial to the distal attachment of the posterior band from the proximal olecranon to the proximal coronoid process (Fig. 18.1.2A and B).
The humeroradial joint is between the fovea of the proximal radius and the capitulum of the humerus. The humeral head rotates about the capitulum during elbow flexion and extension, providing lateral stability to the elbow. The radial head articulates with the radial notch of the
proximal ulna, and is held into this pivot joint by the annular ligament. The radial (lateral) collateral ligament is triangular with its narrow proximal attachment on the lateral epicondyle, and the broader distal attachment into the annular ligament. Some superficial fibers have attachments on the lateral ulna.
proximal ulna, and is held into this pivot joint by the annular ligament. The radial (lateral) collateral ligament is triangular with its narrow proximal attachment on the lateral epicondyle, and the broader distal attachment into the annular ligament. Some superficial fibers have attachments on the lateral ulna.
Blood is supplied to the elbow joint by an anastomosis of branches of the brachial artery crossing the elbow. These include the brachial, superior and inferior ulnar collateral, the anterior and posterior branches of the deep brachial, and the recurrent radial arteries. The anterior and posterior interosseous arteries provide blood to the proximal radioulnar joint. The musculocutaneous (C5-C7), radial (C5-C8, T1) and ulnar (C7-C8, T1) nerves innervate the elbow joint.
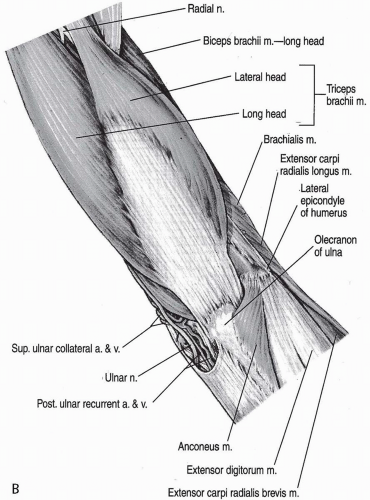
Primary flexors of the elbow include the biceps brachii, brachialis, and brachioradialis
muscles. Proximal attachment of the long head of the biceps is into the supraglenoid tubercle of the scapula, and the short head attaches into the coracoid process of the scapula. The biceps brachii is the strongest supinator of the forearm because of its distal attachment on the radial tuberosity. The brachialis arises from the distal half of the anterior humerus, and inserts upon the coronoid process and tuberosity of the ulna. The brachioradialis takes its proximal attachment from the proximal two thirds of the lateral supracondylar humeral ridge and inserts upon the lateral surface of the distal radius. The biceps brachii and brachialis are within the anterior or flexor compartments of the arm, and are innervated by the musculocutaneous nerve (C5-C6). Although an elbow flexor, the brachioradialis muscle lies within the extensor compartment, while the radial nerve (C5-C7) supplies its innervation (Fig. 18.1.3A and B).
muscles. Proximal attachment of the long head of the biceps is into the supraglenoid tubercle of the scapula, and the short head attaches into the coracoid process of the scapula. The biceps brachii is the strongest supinator of the forearm because of its distal attachment on the radial tuberosity. The brachialis arises from the distal half of the anterior humerus, and inserts upon the coronoid process and tuberosity of the ulna. The brachioradialis takes its proximal attachment from the proximal two thirds of the lateral supracondylar humeral ridge and inserts upon the lateral surface of the distal radius. The biceps brachii and brachialis are within the anterior or flexor compartments of the arm, and are innervated by the musculocutaneous nerve (C5-C6). Although an elbow flexor, the brachioradialis muscle lies within the extensor compartment, while the radial nerve (C5-C7) supplies its innervation (Fig. 18.1.3A and B).
Muscles that flex and extend the wrist and digits also act as secondary flexors and extensors of the elbow. These muscles are arranged by function within fascial compartments in the forearm. The flexor muscles arise from the medial epicondyle, and are housed within the anterior forearm compartment. The extensors occupy the posterior forearm compartment, and arise from the lateral epicondyle.
The flexor carpi radialis (FCR), palmaris longus (PL), and flexor carpi ulnaris (FCU) attach to the medial epicondyle by forming a common flexor attachment. The FCU has two heads, the humeral head arising from the medial epicondyle, and the ulnar head, which arises from the olecranon and posterior border of the ulna. The FCR, PL, and FCU with the pronator teres muscle occupy the superficial forearm compartment, and cross the elbow joint. The flexor digitorum superficialis (FDS) is the largest of the forearm muscles. It divides into two heads, the humeroradial head, which arises from the medial epicondyle, ulnar collateral ligament, and coronoid process of the ulna, and the radial head, which arises from the superior half of the anterior border of the radius. The flexor digitorum profundus (FDP) arises from the anterior surfaces of the ulna and interosseous membrane, covering the proximal three fourths, and is considered to lie in the deep anterior compartment. The flexor pollicis longus (FPL) lies parallel to the FDP, and arises from the anterior surface of the radius and anterior interosseous membrane.
The extensor wad lies along the posterior, medial forearm. The extensor carpi radialis longus (ECRL) arises from the proximal attachment to the supracondylar ridge of the humerus. The common extensor tendon forms the proximal attachment for the muscles that arise from the lateral epicondyle. The four muscles in this group include the extensor carpi radialis brevis (ECRB), the extensor carpi ulnaris (ECU), which also attaches to the posterior border of the ulna, the extensor digitorum (ED), and the extensor digiti minimi (EDM).
The triceps and anconeus muscles extend the elbow. Proximal attachments of the triceps muscle include the long head, which attaches to the infraglenoid tubercle of the scapula; the lateral head, which attaches above the radial groove to the posterior humerus; and the medial head, which attaches to the posterior humerus distal to the radial groove. The distal attachment is to the proximal olecranon process of the ulna and the forearm fascia. The anconeus, an important valgus load stabilizer, attaches proximally to the lateral epicondyle, distally to the lateral olecranon, and superiorly to the posterior ulna. The radial nerve innervates both muscles (triceps C6-C8, anconeus C7-C8, T1).
The biceps brachii and the supinator muscles perform supination of the forearm. The supinator muscle attaches laterally to the lateral epicondyle, radial collateral and annular ligaments, and the supinator fossa and crest of the ulna, then wraps around the radius where it attaches to the posterior, lateral, and anterior proximal one third. As the supinator contracts, it “unwraps,” rotating the forearm into supination. The deep branch of the radial nerve innervates the supinator muscle (C5-C6). The extensor pollicis longus and extensor carpi radialis longus muscles act as secondary supinator muscles.
Primary pronator muscles are the pronator quadratus and pronator teres. The pronator teres is the proximal muscle, with a proximal attachment at the medial humeral epicondyle and the
coronoid process of the ulna. It then crosses the dorsum of the proximal radius to its distal attachment on the lateral radius. The median nerve (C7-C8) innervates the pronator teres. The pronator quadratus, as the name implies, is a rectangular muscle that lies across the dorsum of the distal radius and ulna. The anterior interosseous nerve, a branch of the median nerve (C8-T1), innervates the pronator quadratus.
coronoid process of the ulna. It then crosses the dorsum of the proximal radius to its distal attachment on the lateral radius. The median nerve (C7-C8) innervates the pronator teres. The pronator quadratus, as the name implies, is a rectangular muscle that lies across the dorsum of the distal radius and ulna. The anterior interosseous nerve, a branch of the median nerve (C8-T1), innervates the pronator quadratus.
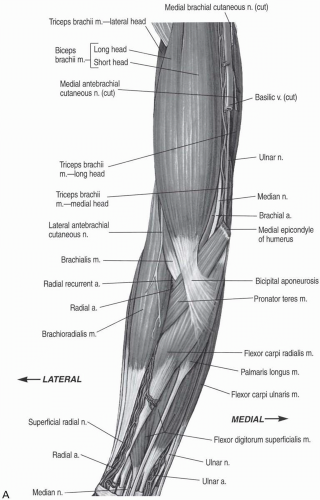 FIGURE 18.1.3. A, Muscles of the elbow, anterior view. B, Muscles of the elbow, posterior view. (From Altcheck DW, Andrews JR. The athlete’s elbow. Baltimore: Lippincott Williams & Wilkins, 2001.) |
The extrinsic finger flexor and extensor muscles, and the long wrist extensors cross the elbow and assist in elbow motion. They are organized into flexor and extensor compartments. Muscles of the extensor compartment
have proximal attachments on the lateral epicondyle or supracondylar ridge. The extensor carpi radialis brevis (ECRB), extensor digitorum (ED), extensor digiti minimi (EDM), and extensor carpi ulnaris (ECU) form a common extensor tendon that attaches to the medial epicondyle. The ECU also has a proximal attachment to the lateral proximal ulna. The extensor carpi radialis longus (ECRL) has a proximal attachment to the supracondylar ridge. The radial nerve and its branches innervate these muscles. The deep branch of the radial nerve (C7-C8) innervates the ECRB. The posterior interosseous nerve (C7-C8) provides innervation to the ED, EDM, and ECU.
have proximal attachments on the lateral epicondyle or supracondylar ridge. The extensor carpi radialis brevis (ECRB), extensor digitorum (ED), extensor digiti minimi (EDM), and extensor carpi ulnaris (ECU) form a common extensor tendon that attaches to the medial epicondyle. The ECU also has a proximal attachment to the lateral proximal ulna. The extensor carpi radialis longus (ECRL) has a proximal attachment to the supracondylar ridge. The radial nerve and its branches innervate these muscles. The deep branch of the radial nerve (C7-C8) innervates the ECRB. The posterior interosseous nerve (C7-C8) provides innervation to the ED, EDM, and ECU.
The flexor/pronator compartment has deep and superficial divisions. The deep muscles, flexor digitorum profundus, flexor pollicis longus, and pronator quadratus do not cross the elbow joint. The superficial muscles, pronator teres (PT), flexor carpi radialis (FCR), palmaris longus (PL), flexor carpi ulnaris (FCU), and flexor digitorum superficialis (FDS) attach in part through a common flexor tendon to the medial epicondyle. The median nerve innervates the PT, FCR (C6-C7), FDS (C7-C8, T1), and palmaris longus (C7-C8). The ulnar nerve innervates the FCU (C7-C8).
Several bursae are located in association with the tendons at the elbow. The three olecranon bursae have clinical significance because of the frequency of inflammation or infection of these structures. The infratendinous olecranon bursa is sometimes present in the triceps tendon as it inserts into the olecranon process. The subtendinous bursa is located between the triceps tendon and the olecranon process, and the subcutaneous bursa may be found superficial to the triceps tendon in the subcutaneous connective tissue (1).
Major structures that cross the volar elbow are located within the cubital fossa. This is a triangular space bounded proximally by the horizontal flexion skin crease, medially by the pronator teres muscles, and medially by the brachioradialis muscle. Following the boundaries are the major veins of the arm, the basilic medially and the cephalic laterally. The intermediate cubital vein runs medial to lateral connecting the basilic and cephalic veins along the distal border of the cubital fossa. The supinator and brachialis muscles form the deepest part of the fossa. The deep and superficial branches of the radial nerve are located with these deep structures. The brachial fascia and the bicipital aponeurosis enclose the fossa superficially. The brachial artery forms its terminal branches within the cubital fossa. The biceps brachii tendon passes through the cubital fossa on its way to insert on the radial tuberosity, and the median nerve is located just medial to the biceps brachii tendon.
REFERENCES
1. Basmajian JV, Slonecker CE. Grant’s method of anatomy, 11th ed. Baltimore: Williams & Wilkins, 1989.
2. Clemente CD. Gray’s anatomy of the human body, American 30th ed. Philadephia: Lea & Febiger, 1985.
3. Moore KL, Agur AM. Essential clinical anatomy. Baltimore: Williams & Wilkins, 1996.
4. Moore KL, Dalley AF II. Clinically oriented anatomy, 4th ed. Philadelphia: Lippincott Williams & Wilkins, 1999:1164.
5. Netter FH. Atlas of human anatomy. Summit, NJ: CIBA-Geigy Corporation, 1995.
6. Rosse C, Gaddum-Rosse P. Hollinshead’s textbook of anatomy, 5th ed. Philadelphia: Lippincott-Raven, 1997.
7. Williams PL, Warwick R, Dyson M, Bannister LH. Gray’s anatomy, British 37th ed. London: Churchill Livingstone, 1989.
8. Woodburne RT, Burkel WE. Essentials of human anatomy, 9th ed. New York: Oxford Univeristy Press, 1994.
18.2 Physical Examination
Nancy White
When it comes to athletics, the elbow is best seen and not heard. It is a crucial link in transmitting force from the shoulder to the hand and it puts the hand in position to act and perform. Though injuries are relatively rare in athletics, breakdown of elbow function can disrupt the kinetic chain and quickly lead to subsequent injury and disability. The flexion-extension and rotatory components of the elbow allow for the appropriate positional placement of the hand.
An adequate clinical history includes assessing acute versus chronic pain, events surrounding the pain (i.e., throwing or racquet use), history of catching or locking, and history of paresthesias. Throwing athletes should be able to identify at which phase of throwing the elbow pain occurs. Referral pain is common to and from the elbow, so a keen eye along the kinetic chain is crucial.
OBSERVATION
Examination of the elbow begins with inspection of both elbows. Appropriate dress to allow for full view of both elbows is essential. Note any discrepancy in muscular definition, atrophy, surgical scars, or abnormal angulation at the elbow.
Initial evaluation of the elbow should also include presence or absence of swelling. Generalized effusion could signal a supracondylar fracture, or radial or olecranon fracture or dislocation. Focal swelling over the olecranon generally resembles a goose egg and represents olecranon bursitis. In this case, monitor for any signs of erythema or calor, which represent a secondary infection.
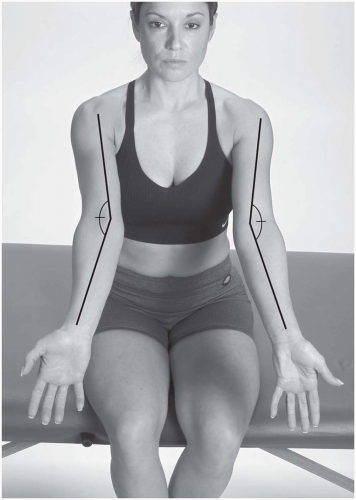
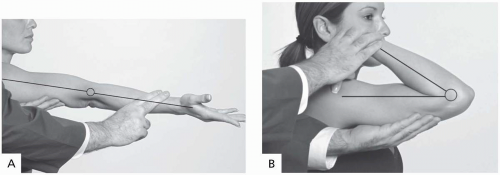
Alignment and mobility should be examined in the anteroposterior (AP) and lateral planes. In the AP view with the elbow extended, the carrying angle can be visualized. This is the valgus angle between the shaft of the humerus and the center line of the forearm (Fig. 18.2.1). Normal carrying angle is between 5 and 10 degrees and is usually 5 degrees greater in women than in men (2). Note any discrepancy in the carrying angle between the two elbows. Fractures of the distal humerus can alter the carrying angle.
Another way to examine alignment is to note the position of the epicondyles and the olecranon tip. At 90 degrees of flexion, the epicondyles should be equidistant to the tip of the olecranon. If not, a fracture or dislocation should be suspected in the face of an acute injury.
From the lateral position, note the alignment of the olecranon with the humeral shaft. Posterior and posterolateral dislocations result in an obvious deformity, due to the location of the olecranon process posterior to the humeral shaft.
PALPATION
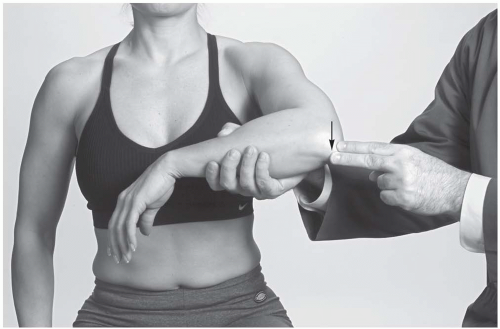
In the medial elbow compartment, the primary bony structure is the medial epicondyle (Fig. 18.2.2). Pain over the bony prominence, especially in conjunction with resisted wrist flexion and pronation, is indicative of medial epicondylitis. If pain is present in a young athlete, the examiner should consider a growth plate injury.
The medial collateral ligament is the most important stabilizer of the elbow, and its stability should be evaluated in every elbow examination. Palpate its epicondylar and ulnar attachments, noting tenderness, thickness, irregularity, and bogginess (Fig. 18.2.3). The anterior bundle is important to palpate, as it resists valgus load in throwing. Normal ligaments are never tender, so pain in this region warrants further investigation. The flexor carpi ulnaris lies superficial to the ulnar collateral ligament, so do not assume immediately that pain here is a torn medial collateral ligament.
Proximal to the medial epicondyle is the supracondylar region of the distal humerus. Tenderness in this area should alert the examiner to consider a fracture, especially in the face of a traumatic history.
The ulnar nerve can be palpated at the medial epicondyle and followed distally and anteriorly along the wrist flexor muscle bellies. If pain is
elicited with gentle palpation of the nerve, the examiner should consider a nerve irritation injury.
elicited with gentle palpation of the nerve, the examiner should consider a nerve irritation injury.
In the lateral aspect, the radial nerve crosses the lateral supracondylar line as it traverses from the posterior to anterior compartments. Tenderness of the medial aspect of the extensor muscle bellies (3-4 cm distal and medial to the lateral epicondyle) may indicate radial nerve entrapment (radial tunnel syndrome).
The radial head is palpated posterior and medial to the wrist extensor muscle bellies and just distal to the lateral epicondyle (Fig. 18.2.4). Palpation, along with rotation, aids in the diagnosis of radial head subluxation or proximal radius injuries.
In the posterior compartment of the elbow, palpation of the olecranon bursa is relatively easy, as it overlies the distal triceps tendon and olecranon (Fig. 18.2.5). Note any swelling, pain, or thickening of the bursa or bony fragments, particularly after a traumatic injury. The tip of the olecranon is best noted with the elbow flexed beyond 60 degrees. The fossa, just superior to the olecranon tip, is also best palpated with the elbow in the flexed position. Note any pain, crepitus with flexion or extension, or bony fragments that would require further radiographic studies to evaluate for bony impingement.
The primary structure in the volar compartment of the elbow is the distal biceps tendon, which inserts onto the proximal radius. Note any pain in this area, which is common for overhead throwing athletes who sustain either acute trauma or overuse injury. Also palpate the brachial artery and compare it with the contralateral elbow.
RANGE OF MOTION
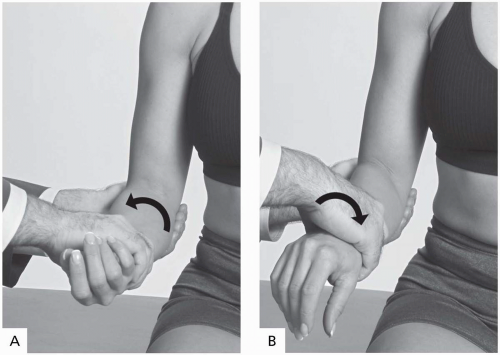
Active motion should be examined first. Full extension is 0 degrees of flexion, and full flexion is approximately 140 to 150 degrees. Flexion and extension are primarily a function of the humeral-ulnar component of the elbow joint (Fig. 18.2.6A and B). Pronation and supination are primarily a function of the proximal radialulnar articulation (2). It is easiest to evaluate pronation and supination with the elbow flexed to 90 degrees. Neutral position is with the thumb up. From here, normal pronation is 90 degrees palm down, while supination is 90 degrees palm up (Fig. 18.2.7A and B).
Restriction or pain in motion should be evaluated further. Restricted motion may signal arthropathy, loose bodies, or muscular restriction. In particular, limited extension should signal the examiner to look for possible posterior humeral-ulnar joint arthropathy or posterior joint loose bodies. Loss of extension may also result from restriction of the distal biceps tendon. Athletes such as baseball pitchers may develop flexor contractures, yet have no loss of function or skill. (1)
TABLE 18.2.1. PASSIVE RANGE OF MOTION FOR THE ELBOW | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Similarly, limited flexion may represent anterior humeral-ulnar joint pathology or capsulitis. Any loss of motion should first be investigated with appropriate imaging. Normal ranges of elbow passive motion are listed in Table 18.2.1 (3).
NEUROVASCULAR EXAMINATION
Motor Strength
The muscles of the elbow are listed in Table 18.2.2. The primary motions for motor testing are elbow extension and flexion, and wrist pronation and supination. Testing is on a +5 scale. Testing biceps strength is best done with the forearm in full supination, while brachialis strength can be best assessed with the forearm in full pronation (1).
Sensory
The lateral epicondyle is in the C5 dermatome. The radial forearm, thumb, and index fingers are in the C6 dermatome. The C7 dermatome can be checked by testing the sensation of the long finger. The ring and fifth fingers, along with the hypothenar eminence, are innervated by the C8 sensory nerve. The ulnar forearm and medial epicondyle are innervated by T1. The sensory nerve for the proximal arm near the axilla is T2.
TABLE 18.2.2. MUSCLES OF THE ELBOW | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree