20.1 Anatomy
William M. Falls
Gail A. Shafer-Crane
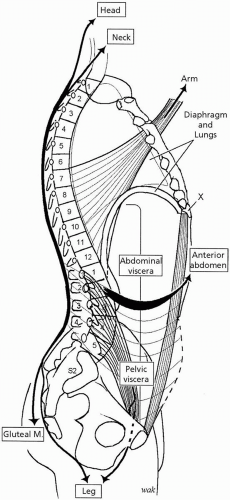
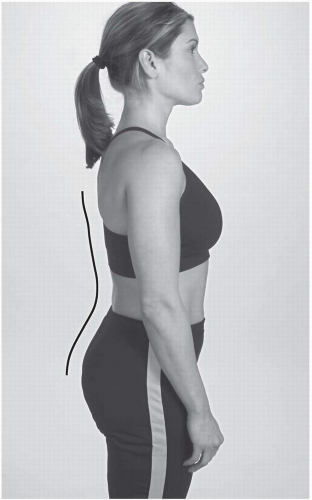
The thoracic spine, which consists of the 12 thoracic vertebrae, contains the thoracic and upper lumbar portions of the spinal cord and associated nerve roots whose branches supply the back and the anterolateral thoracic and abdominal walls in a segmental fashion from the neck to the pelvis. This region of the vertebral column serves as an attachment for the ribs and transmits the weight of the body to the lumbosacral spine. The thoracic spine is concave anteriorly. Anatomy of the thoracic spine is presented in detail in major anatomic textbooks (
1,
2,
3,
4,
5,
6).
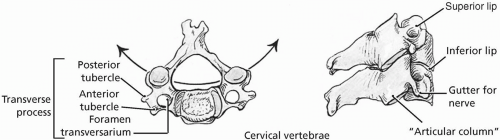
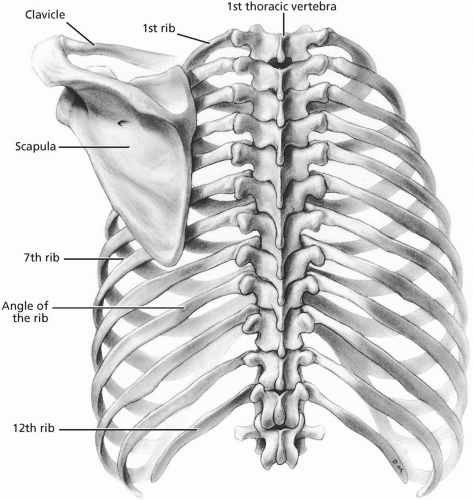
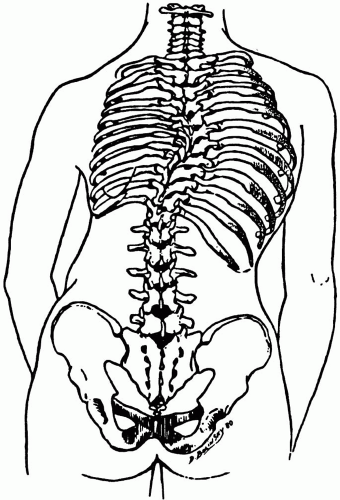
The distinguishing feature of all 12 thoracic vertebrae is that they articulate with at least one pair of ribs (
Fig. 20.1.1). Typical thoracic vertebrae (T2-T9) articulate with two pairs of ribs; the head of the rib contacts a facet on the superior margin of one vertebral body and a similar facet on the inferior margin of the vertebral body above. In addition, there is a facet on the transverse processes of thoracic vertebrae T1-T10.
Bodies of thoracic vertebrae increase in size from T1 to T12 and display highly convex anterior surfaces, which protrude deeply into the thoracic cavity. This protrusion is exaggerated by the direction of the transverse processes, which project posteriorly and superiorly as well as laterally. The pedicles attach to the superior ends of the vertebral bodies thereby creating deep inferior vertebral notches, which accommodate the spinal nerve roots. The laminae are broad and those of the superior vertebra overlap those of the vertebra lying immediately inferior.
The long and slender spinous processes point inferiorly and overlap the vertebra lying inferiorly. The spinous processes of the lower thoracic vertebrae resemble those of lumbar vertebrae; they are shorter, stouter, and project more posteriorly. The superior and inferior articular processes are situated anterior to the transverse process and their facets are oriented in the coronal plane. The superior facet faces posteriorly and laterally, while the inferior facet faces anteriorly and medially (
Fig. 20.1.2). There is an abrupt transition in the orientation of the articular processes at the level of T12 where the inferior articular process becomes oriented to match those of the lumbar vertebrae with an anterolaterally directed facet.
There are 12 pairs of ribs, which articulate with the thoracic vertebrae through their heads and short necks. The head of a typical rib has a superior and inferior facet divided by a crest for articulation with the bodies of two adjacent thoracic vertebrae. The superior border of the narrower neck also displays a crest for the attachment of ligaments. The neck terminates laterally in an articulating tubercle, which bears an oval, convex facet for articulation with the transverse process of the similarly numbered thoracic vertebrae. Lateral to the facet is a rough area for attachment of a ligament. The tubercle marks the junction of the neck and the body of the rib, which turns sharply forward at the angle and slants inferiorly and forward. The head of the first rib is different from the others in that it only has a single facet for articulation with the facet on the superior margin of the body of the T1 vertebra.
The thoracic spine is composed of two types of joints, which work together to provide mobility for the spine. These include facet joints (zygapophyseal joints) and intervertebral body joints (intervertebral discs). The facet joints are synovial joints between the articular processes of adjacent vertebrae. A thin, loose articular capsule surrounds each joint. The facet joints permit gliding movements between the vertebrae, and the shape of the articular surfaces limits the range of motion possible. Branches arising from the posterior primary rami of spinal nerves innervate these joints.
The intervertebral discs are fibrocartilaginous joints, designed for weight bearing and strength, situated between the bodies of adjacent vertebrae. Each intervertebral disc consists of an outer anulus fibrosus, composed of concentric lamellae of fibrocartilage, which surrounds a gelatinous nucleus pulposus. The anuli insert into the rounded rims on the articular surfaces of adjacent vertebral bodies. Branches arising from the anterior primary rami of spinal nerves innervate the intervertebral discs. The intervertebral discs are avascular structures, that receive their blood supply by diffusion from the vertebral bodies. Mobility of the thoracic spine, especially in its superior and middle regions is limited mainly due to the ribs and rib cage as well as the narrowness of the intervertebral discs. Rotation takes place primarily in the thoracic spine, with flexion, extension, and lateral bending being extremely limited.
Ligaments reinforce and stabilize the facet joints and the intervertebral discs. The anterior longitudinal ligament is a broad, thick band attaching to anterior and anterolateral surfaces of the vertebral bodies and intervertebral discs. It limits extension of the vertebral column. The posterior longitudinal ligament runs within the vertebral canal and attaches to the posterior surfaces of the vertebral bodies and the intervertebral discs. In the thoracic region it narrows over the surfaces of the vertebral bodies and expands over the intervertebral discs. The posterior longitudinal ligament checks flexion of the vertebral column. The strong, highly elastic, flattened ligamenta flava attach to the laminae of adjacent vertebrae. These ligaments help to preserve the normal curvature of the vertebral column and straighten the vertebral column after it has been flexed. Short interspinous ligaments and a strong cordlike supraspinous ligament join adjacent spinous processes. The intertransverse ligaments connect adjacent transverse processes and are insignificant in the thoracic spine.
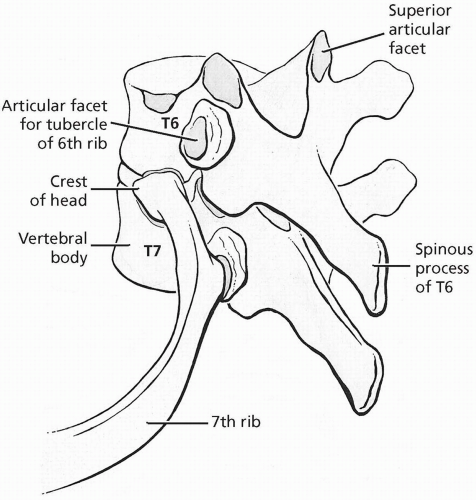
The ribs articulate with the thoracic spine at two synovial joints: the costovertebral and costotransverse joints. At the costovertebral joint, the head of a rib articulates with two vertebral bodies (
Fig. 20.1.3). A ligament attaching the crest of the head to the intervertebral disc divides the joint cavity. The articular capsule is thickened anteriorly by the radiate ligament, which anchors the head of the rib to the intervertebral disc and to the thoracic vertebral bodies superior and inferior to the disc. The costotransverse joint is between the articulating tubercle on the rib and the transverse process of the vertebra. The joint has a small cavity and is strengthened by three costotransverse ligaments. These extend between the crest on the rib neck and the transverse process superior to the rib (superior costotransverse ligament), between the posterior aspect of the rib neck and its own transverse process (costotransverse ligament), and between the tip of the transverse process and the rough part of the articulating tubercle (lateral costotransverse ligament). These joints are responsible for the pump-handle and bucket-handle movements of the ribs. Both joints receive their arterial supply from branches of the posterior intercostal arteries and are innervated by branches of the posterior primary rami of the thoracic spinal nerves.
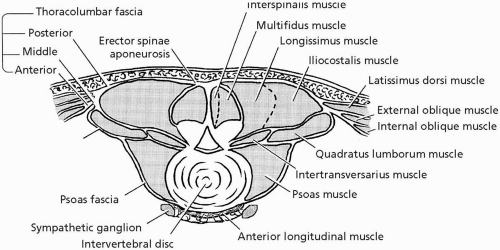
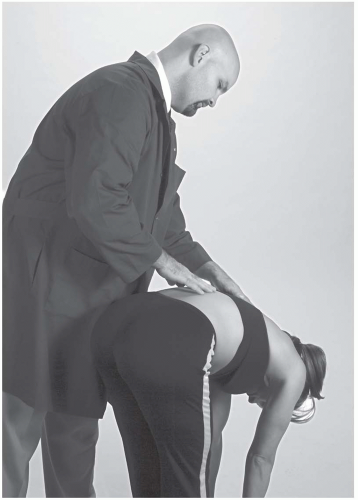
The control and strength of movements in the thoracic spine, as well as in other regions of the spine, are dependent on muscles. Muscles help to stabilize the spine and control the effects of gravity. The extensor muscles are the one major functional group of the thoracic spine. This group is also capable of rotating and side bending the spine. Flexor muscles located on the anterior aspect of the spine in other regions are absent in the thoracic spine. The extensor muscles (deep back muscles) span the
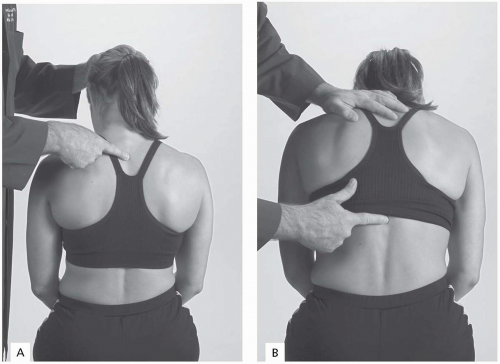
entire back from the skull to the sacrum and in the thoracic region are situated posterior to the laminae and transverse processes between the spinous processes medially and the angle of the ribs laterally. They are innervated segmentally by the posterior primary rami of the thoracic spinal nerves. These muscles consist of two groups: erector spinae and transversospinalis. The muscles are enclosed in the thin thoracic portion of the thoracolumbar fascia, which attaches to the spinous processes of the thoracic vertebrae and the angles of the ribs and separates the muscles from overlying superficial muscles. The erector spinae muscles (
Fig. 20.1.4) are responsible for restoring the spine to the erect posture after flexion and also act to control flexion of the spine against gravity. The transversospinalis muscles act primarily to rotate the spine.
The erector spinae and transversospinalis muscles are arranged in three layers: superficial, intermediate, and deep. In the thoracic spine, the superficial layer consists of three vertically running columns of muscles. The most lateral column is the iliocostalis, which runs along the angles of the ribs. Portions of all three subdivisions of the iliocostalis—lumborum, thoracis, and cervicis—can be found in the thoracic spine. The intermediate column is the longissimus, which is associated with the transverse processes. In the thoracic spine, the thoracis and part of the cervicis subdivisions of the thoracis muscle can be found. The medial column is the spinalis, which is associated with the spinous processes. The thoracis subdivision of the spinalis muscle is well developed and is always present. The intermediate layer is composed of two subgroups of the transversospinalis muscles. As the name of this muscle group implies, the transversospinalis muscles arise from transverse processes and insert into spinous processes.
In the thoracic spine the intermediate layer is composed of the thoracis and cervicis portions of the semispinalis muscle and deep to them, the multifidus muscles. The semispinalis muscles span up to six vertebrae, while the multifidus muscles span two to four vertebrae. The deep layer is composed of segmental muscles: interspinous, intertransverse, and rotator groups.
All of these groups are better developed in the cervical and lumbar spine than they are in the thoracic spine. The rotators typically span one to two vertebrae. In the thoracic spine the deep back muscles and the overlying thoracolumbar fascia are covered by other muscles, which are not innervated by the posterior primary rami of the thoracic spinal nerves and which attach the upper limb to the vertebral column. These include the trapezius, latissimus dorsi, and deep to the trapezius, the rhomboids.
Blood supply to the thoracic spine, associated muscles, nerve roots, and spinal cord is derived from 12 pairs of posterior intercostal arteries arising from the costocervical trunk of the subclavian artery (posterior intercostals 1 and 2) and the thoracic aorta (posterior intercostals 3 to 12), which enter and course in the intercostal spaces on the anterolateral thoracic wall. Near its origin each posterior intercostal artery gives off a posterior branch that passes posteriorly with the posterior primary rami of the corresponding thoracic spinal nerve. This branch supplies the back muscles and overlying skin as well as the thoracic spine and contributes to supply the nerve roots, the spinal cord and its coverings, and the thoracic vertebrae through a spinal branch that enters through the intervertebral foramen.
The spinal cord and its coverings (meninges) are located in the vertebral canal of the thoracic spine. The thoracic spine contains the thoracic and upper lumbar spinal cord segments along with their anterior and posterior nerve roots. Thoracic spinal nerves (12 pairs) are formed just outside the intervertebral foramen by the union of the anterior and posterior roots. In the thoracic spine, the spinal nerves are formed below the vertebra they correspond to in number. Thus, the T1 spinal nerve is formed just outside the intervertebral foramen between the T1 and T2 vertebrae. After the spinal nerve is formed, it divides almost immediately into anterior and posterior primary rami. The posterior primary rami innervate segmentally skin and muscles of the back as well as the zygapophyseal joints of the thoracic spine. The anterior primary rami enter the intercostal spaces and become the intercostal nerves innervating segmentally skin and muscles of the anterolateral thoracic and abdominal walls. Situated on the anterior aspect of the necks of the ribs, on each side of the thoracic spine, are the thoracic sympathetic trunks consisting of 11 to 12 ganglia linked together. Each ganglion is connected to an intercostal nerve by two branches. The last ganglion may be connected to both the eleventh and twelfth intercostal nerves.
Arising from the ganglia of the thoracic sympathetic trunks are three splanchnic nerves (greater, lesser, and least), which descend toward the diaphragm on the anterior aspects of the thoracic vertebral bodies.
REFERENCES
1. Basmajian JV, Slonecker CE. Grant’s method of anatomy, 11th ed. Baltimore: Williams & Wilkins, 1989.
2. Clemente CD. Gray’s anatomy of the human body, Amercian 30th ed. Philadelphia: Lea & Febiger, 1985.
3. Moore KL, Agur AM. Essential clinical anatomy. Baltimore: Williams & Wilkins, 1996.
4. Rosse C, Gaddum-Rosse P. Hollinshead’s textbook of anatomy, 5th ed. Philadelphia: Lippincott-Raven, 1997.
5. Williams PL, Warwick R, Dyson M, Bannister LH. gray’s anatomy, British 37th ed. London: Churchill Livingstone, 1989.
6. Woodburne RT, Burkel WE. Essentials of human anatomy, 9th ed. New York: Oxford University Press, 1994.