Foot and Ankle
24.1 Anatomy
Gail A. Shafer-Crane
William M. Falls
SKELETAL
Three bones participate in the ankle joint: the tibia and fibula of the leg, and the talus bone, a tarsal bone. The tibia widens distally, forming the medial malleolus, while the distal fibula also enlarges to form the lateral malleolus. The tibia and fibula articulate distally in the distal tibiofibular joint. The inferior surface is a deep concave, articular surface that becomes the mortise of the ankle joint. The medial and lateral malleoli are bony landmarks that are easily palpated, and provide reference points for palpation of the rest of the ankle. The wedge-shaped rounded trochlea (Latin, pulley) of the talus fits within the mortise formed by the malleoli, creating a synovial hinge joint (1,2,3,4,5,6).
Osteology of the foot includes the tarsal bones, talus, calcaneus, navicular, cuboid, three cuneiform bones, five metatarsal bones, and the phalanges. (Fig. 24.1.1). The transverse talar joint is formed by the anterior articulation of the calcaneus and cuboid bones and the talus and navicular bones. The subtalar joint is between the talus and calcaneus. The tarsometatarsal joint is between the cuneiform bones, the cuboid bone, and the metatarsals. The five metatarsals articulate with the proximal phalanges forming the metatarsophalangeal joints. The joints of the toes are the proximal and distal interphalangeal joints.
The articulations of the tarsal and metatarsal bones and their ligaments form the transverse and longitudinal arches of the foot. The cuboid and cuneiform bones and the metatarsal bases form the transverse arch. The calcaneus, talus, navicular, three cuneiforms, and medial three metatarsal bones form the medial longitudinal arch; and the calcaneus, cuboid, and lateral two metatarsals form the lateral longitudinal arch. These arches permit significant shock absorption by flattening out and springing back during loading of the foot.
The distal tibiofibular joint is felt by placing the fingers anterior to the lateral malleolus, thumb posterior, and gently pinching. The fibula can be mobilized in an oblique anterior-posterior direction. The anterior ankle joint can be felt as a depression between the tendons as they cross the ankle. The talar trochlea is palpated by applying pressure, gently, in this depression as the foot is extended. The prominence formed by the head of the second metatarsal as it articulates with the second cuneiform bone lies just lateral to the long medial extensor tendon, extensor hallucis longus, and deep to the dorsalis pedis artery. The tuberosity of the fifth metatarsal is palpated along the lateral border of the foot.
JOINTS
The distal tibiofibular joint is a fibrous joint, or syndesmosis. Very little mobility is present at this joint; however, as the foot is dorsiflexed,
the wedge-shaped talus exerts enough pressure to open this joint slightly. For this reason, the ankle joint is more stable in dorsiflexion than in volar flexion.
the wedge-shaped talus exerts enough pressure to open this joint slightly. For this reason, the ankle joint is more stable in dorsiflexion than in volar flexion.
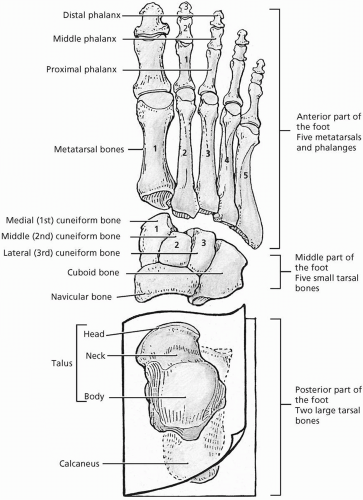 FIGURE 24.1.1. Bony anatomy of the foot. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
The interosseous membrane is a tough connective tissue sheet between the tibia and fibula. This membrane separates the leg into the anterior and posterior compartments, and then continues to become the interosseous ligament of the distal tibiofibular joint. Anterior and posterior inferior tibiofibular ligaments provide further reinforcement.
The tibiotalar joint is the mortise joint, formed by the distal tibiofibular joint as it articulates with the trochlea of the talus. Plantarflexion (extension) of the ankle is permitted as the talus rocks anteriorly, and dorsiflexion (flexion) occurs as the talar trochlea rocks posteriorly, slightly separating the distal tibiofibular joint. The posterior wall of the mortise joint is formed by a continuation of the inferior tibiofibular ligament, the transverse tibiofibular ligament (Fig. 24.1.2). Blood supply to the tibiotalar joint is from the perforating branch of the fibular artery, and from the medial and malleolar branches of the anterior and posterior tibial arteries. The deep fibular, tibial, and saphenous nerves provide innervation.
There are three articulations of the proximal tarsals. The transverse tarsal or talocalcaneonavicular is a synovial ball-and-socket joint. The subtalar and calcaneocuboid joints are plane synovial-type joints. These joints collectively permit inversion and eversion of the foot through gliding and rotational motions between the tarsals. Intertarsal ligaments are named for their proximal and distal attachments to the tarsals. The spring, or talocalcaneonavicular, ligament is an important structure because it supports the transverse arch of the foot. These joints receive their blood supply from the posterior and anterior tibial, posterior fibular, and lateral tarsal arteries. The medial and lateral plantar nerves innervate the plantar aspect of these joints, while the deep fibular nerve innervates the dorsum.
 FIGURE 24.1.2. Posterior ankle joint. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
The distal tarsals articulate with the bases of the metatarsals forming tarsometatarsal joints. These plane joints are synovial with fibrous capsules formed by the dorsal, plantar, and interosseous ligaments. Limited gliding between the bones is permitted. Blood supply is from the lateral tarsal artery, which is a branch of the dorsalis pedis. The deep fibular, lateral plantar, and sural nerves provide innervation.
The bases of the metatarsals articulate with one another in the intermetatarsal joints. These are plane-type synovial joints, which permit limited gliding. The dorsal, plantar, and interosseous ligaments form the fibrous capsules. The lateral tarsal artery provides the blood supply, and the innervation is by the digital nerves.
The metatarsals are long bones that form the plantar surface of the foot. Their heads articulate with the proximal phalanges in the metatarsophalangeal joints. These plane-type synovial joints allow limited gliding. Collateral and plantar ligaments form the fibrous capsules. The lateral tarsal artery provides the blood supply. Innervation is by the digital nerves.
LIGAMENTS
The lateral ankle is stabilized by three ligaments. The anterior talofibular ligament attaches the lateral malleous to the neck of the talus. The posterior talofibular ligament attaches the malleolar fossa to the lateral tubercle of the talus. The calcaneofibular ligament is a round cord that attaches the tip of the lateral malleolus to the lateral calcaneus.
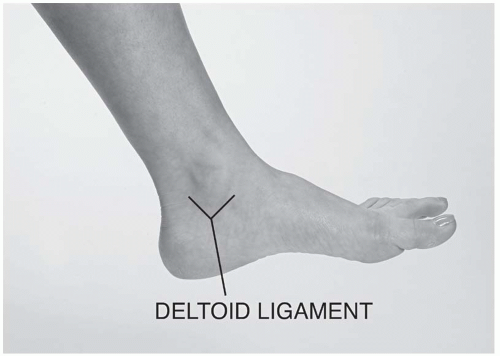
The medial deltoid ligament has three components, the tibionavicular, anterior and posterior tibiotalar, and tibiocalcaneal ligaments. The apex of this triangular ligament makes its proximal attachment at the medial malleolus, and then fans out to attach to the navicular, talus, and calcaneus tarsal bones (Fig. 24.1.3A-B). This ligament supports the ankle during eversion, acts to prevent subluxation, and assists in maintaining the medial longitudinal arch of the foot. Blood supply to the tibiotalar joint is from the malleolar branches of the fibular and anterior and posterior tibial arteries. The deep fibular and tibial nerves innervate this joint.
TOES
The bones of the toes are the proximal, middle, and distal phalangeal bones. The great toe has only two phalanges, while the others have three. The interphalangeal joints are hinge-type synovial joints that allow flexion and extension. The collateral and plantar ligaments form the fibrous capsules. The superficial fibular nerve forms the digital nerve. These provide cutaneous innervation to the skin of the dorsum of the foot, and all toes except the lateral surface of the little toe and the adjacent surfaces of the great toe and the second toe. Superficial branches of the lateral and medial plantar nerves, which are continuations of the posterior tibial nerve, supply the plantar surfaces of the toes, and intrinsic muscles of the foot.
MUSCLES
Muscles of the ankle and foot are divided into extrinsic and intrinsic muscles. The extrinsic ankle dorsiflexor and toe extensor muscles are housed in the anterior compartment of the leg. The tibialis anterior muscle makes its proximal attachment on the lateral tibial condyle and superior lateral surface of the tibia and interosseous membrane. It narrows into a long tendon that traverses the ankle beneath the extensor retinaculum to attach on the medial and inferior surfaces of the medial cuneiform and base of the first metatarsal. Innervation is the deep fibular nerve (L4-L5). The extensor digitorum longus muscle runs just lateral to the tibialis anterior. Its proximal attachment is to the lateral tibial condyle, and proximal three fourths of the interosseus membrane and fibula. Its long tendon attaches to the middle and distal phalanges of the lateral four toes. The extensor hallucis longus attaches proximally to the middle of the fibula and interosseous membrane. The long tendon attaches to the distal phalange of the great toe. The fibularis tertius is a short muscle that makes its proximal attachment to the distal fourth of the interosseous membrane and fibula, crosses the ankle beneath the extensor retinaculum, and then attaches to the dorsum of the fifth metatarsal. The deep fibular nerve (L5-S1) innervates these three muscles.
These ankle dorsiflexor and toe extensor muscles pass beneath the extensor retinacula of the ankle. These structures are thickenings of the deep fascia of the leg. The superior retinaculum is a Z-shaped structure arising from the medial tibia and medial malleolus and crossing over the extensor tendons to attach on the fibula superior to the lateral malleolus and the cuboid bone. The inferior extensor retinaculum arises from the cuboid, and then crosses from lateral to medial over the long extensor tendons to attach to the first cuneiform bone. A second component arises from the first cuneiform bone, and crosses from medial to lateral to attach to the second metatarsal. Each extensor tendon is housed within a synovial sheath formed as the tendon emerges from the muscle and extending distal to the retinacula. These fluid-filled sacs provide lubrication and fluid pressure to limit impingement by the retinacula.
Plantarflexors of the ankle and flexors of the toes are housed in the posterior compartments
of the leg. The plantarflexors are within the superficial posterior compartment. All of these muscles are innervated by the tibial nerve (S1-S2) and insert into the posterior surface of the calcaneus bone. The gastrocnemius splits forming the inferior borders of the popliteal fossa at the knee. The medial head attaches to the popliteal surface of the femur and just superior to the medial femoral condyle. The lateral head attaches to the lateral femoral condyle. The action of the gastrocnemius depends on the position of the knee. It plantarflexes the foot during knee extension to raise the heel during ambulation and is also a secondary knee flexor. The soleus muscle lies beneath the gastrocnemius within the superficial dorsal compartment of the leg, plantarflexes the ankle, but acts independently from the knee. The plantaris muscle lies between the gastrocnemius and soleus. It is a very thin, long, triangular-shaped muscle that terminates into a very thin, cordlike tendon. Its proximal attachment is above the knee at the lateral supracondylar line of the femur and into the oblique popliteal ligament.
of the leg. The plantarflexors are within the superficial posterior compartment. All of these muscles are innervated by the tibial nerve (S1-S2) and insert into the posterior surface of the calcaneus bone. The gastrocnemius splits forming the inferior borders of the popliteal fossa at the knee. The medial head attaches to the popliteal surface of the femur and just superior to the medial femoral condyle. The lateral head attaches to the lateral femoral condyle. The action of the gastrocnemius depends on the position of the knee. It plantarflexes the foot during knee extension to raise the heel during ambulation and is also a secondary knee flexor. The soleus muscle lies beneath the gastrocnemius within the superficial dorsal compartment of the leg, plantarflexes the ankle, but acts independently from the knee. The plantaris muscle lies between the gastrocnemius and soleus. It is a very thin, long, triangular-shaped muscle that terminates into a very thin, cordlike tendon. Its proximal attachment is above the knee at the lateral supracondylar line of the femur and into the oblique popliteal ligament.
 FIGURE 24.1.3. Lateral (A) and medial (B) ligaments of the ankle. (From Stoller DW. MRI, arthroscopy, and surgical anatomy of the joints. Baltimore: Lippincott Williams & Wilkins, 1999.) |
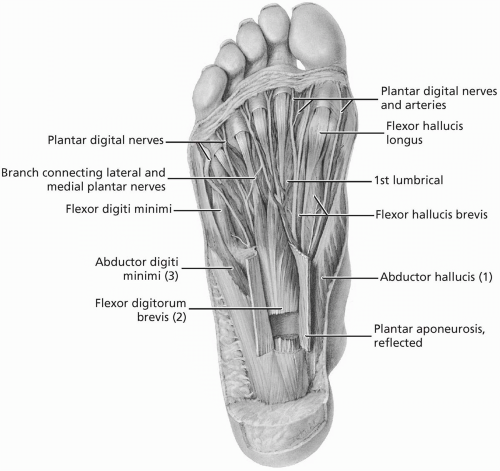
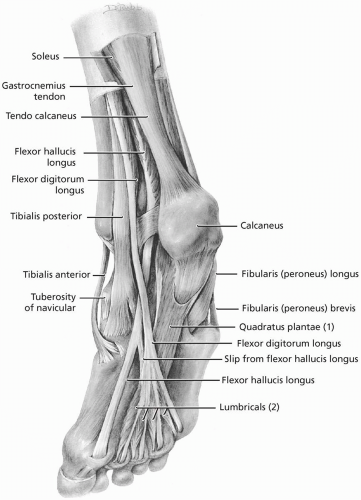 FIGURE 24.1.4. Muscles and tendons in the sole of the foot. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
The toe flexors occupy the deep posterior compartment of the leg. The flexor hallucis longus (FHL) attaches proximally to the distal two thirds of the fibula, and distally to the base of the distal phalanx of the great toe. The flexor digitorum longus (FDL) lies medial to the FHL. It attaches proximally to the middle posterior surface of the tibia distal to the attachment of the soleus, and to the fibula by a broad tendon. Its long tendon passes beneath the tendon of its medial neighbor, the tibialis posterior before entering the flexor retinaculum and inserting onto the bases of the distal phalanges of the lateral four toes. The tibial nerve (S2-S3) innervates the FHL and FDL.
The tibialis posterior is the most medial of these three deep muscles, arising from the interosseous membrane, the posterior surface of the tibia distal to the origin of the soleus muscle, and the posterior surface of the fibula. It crosses the ankle beneath the flexor retinaculum between the tendons of the FDL and FHL before inserting on the tuberosity of the navicular, cuneiform, and cuboid bones and onto the bases of the middle three metatarsals. The tibial nerve (L4-L5) innervates the tibialis posterior.
The tarsal tunnel is an arch formed by the medial malleolus and calcaneus bones as its floor, and the flexor retinaculum as its roof. The long tendons of the FDL, tibialis posterior, and FHL traverse the ankle with the posterior tibial artery and the tibial nerve. The tendons within this compartment are housed within synovial sheaths.
Two muscles, the fibularis (peroneus) longus and brevis, evert the foot and weakly plantarflex the ankle. They are extrinsic muscles housed within the lateral compartment of the leg. Their proximal attachments are the head and superior and inferior two thirds of the lateral fibula, respectively. The fibular nerve (L5-S2) innervates these extrinsic muscles.
The intrinsic muscles of the foot make their proximal and distal attachments distal to the ankle. The plantar surface of the foot is organized in four layers (Fig. 24.1.4). The intrinsic muscles and the tendons of the extrinsic muscles are interwoven through these layers. Synovial sheaths encase the flexor and extensor tendons of the toes. Sesamoid bones are carried in the flexor tendons of the great toe.
Innervation of the sole of the foot is by the medial and lateral plantar nerves, which branch into deep and superficial branches. Their terminal branches, the plantar digital nerves, supply the toes.
The skin of the plantar surface of the foot is very thick. Just deep to the skin is a tough, thick layer of plantar fascia. The plantar aponeurosis is a deeper layer of connective tissue with longitudinal fibers running from the medial calcaneus to the distal phalanges.
REFERENCES
1. Basmajian JV, Slonecker CE. Grant’s method of anatomy, 11th ed. Baltimore: Williams & Wilkins, 1989.
2. Clemente CD. Gray’s anatomy of the human body. American, 30th ed. Philadelphia: Lea & Febiger, 1985.
3. Moore KL, Agur AM. Essential clinical anatomy. Baltimore: Williams & Wilkins, 1996.
4. Rosse C, Gaddum-Rosse P. Hollinshead’s textbook of anatomy, 5th ed. Philadelphia: Lippincott-Raven, 1997.
5. Williams PL, Warwick R, Dyson M, Bannister LH. Gray’s Anatomy, British 37th ed. London: Churchill Livingstone, 1989.
6. Woodburne RT, Burkel WE. Essentials of human anatomy, 9th ed. New York: Oxford University Press, 1994.
24.2 Physical Examination
Steven J. Karageanes
FOOTWEAR
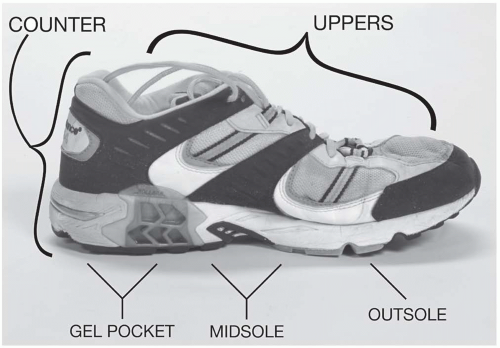
Any athlete who has a foot and ankle problem should always bring his or her footwear into the examination as well. Shoe defects are recognized as a common source of foot injury (1). Overall wear should be initially assessed, and though many guides exist for how long an athlete can use a shoe, each situation must be evaluated individually. Injury prevention starts with assessing the type and quality of shoes (2). Heavy runners will typically wear down a shoe faster than a lighter runner, but a basketball player may not wear shoes as hard as a competitive tennis player. Shoes can lose more than 40% of their shock-absorbing capacity after 250 to 500 miles. The rule of thumb is to change shoes every 6 months. This will vary with the sport and usage, so knowing the essentials of footwear will help a clinician to
determine the appropriate type of shoe and when to replace it.
determine the appropriate type of shoe and when to replace it.
Uppers
Uppers consist of the material attached to the sole that encloses the foot. The material is typically much thinner than cross-training shoes to allow for evaporation of sweat and a lighter shoe. Look at the medial portion and see if the athlete’s foot hangs over the sole. A curved (adductus) foot in a straight shoe may not fit properly and lead to problems. An overpronating foot will compress the arch and break it down faster. This problem is worse in a curved shoe, so most overpronators do best in a straight shoe with motion control and firm midsole support (Fig. 24.2.1). Conversely, a straight foot in a curved shoe may have excess bulging off the lateral aspect, leading to more pressure on the little toe and fifth metatarsophalangeal (MTP) joint. Look for abnormal friction or peel-away from the sole everywhere. Excessive wear on an upper may indicate contact with the opposite foot, which can result from a narrow base, crossing over of the other foot, an uncompensated equinus contracture, or hamstring restriction.
Counter
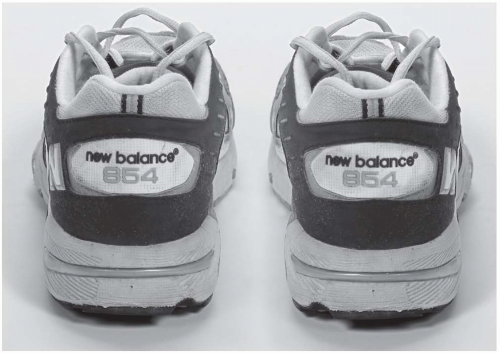
The counter is the hindfoot of the shoe. It attaches to the uppers and embeds its base into the rear of the sole. Unlike the uppers, the counter is stiff and designed to limit mobility. Look for the alignment or tilt and note if it tilts medially (pronation) or laterally (supination). Note any wear on the inside of the counter, which can be caused by excessive heel motion in a shoe too big (Fig. 24.2.2).
Check the counter itself. It should be firm and minimally mobile. A mobile counter is a sign of a cheap shoe with excessive subtalar and talar motion. Particularly in runners, shoes need to minimize talar motion and exhibit more control of the talus; otherwise, the eccentric load on the Achilles tendon, posterior tibialis, and peroneus muscles will increase, leading to mechanical fatigue and breakdown.
The portion of the outsole under the counter is usually constructed with a gel pocket or air cushion inside the sole. This should be given special attention during the examination. Defects in this structure, such as pad rupture, deflation, or fracturing, can alter talar mechanics during heel strike and lead to multiple problems. Make sure each pocket is inflated evenly by comparing the two shoes side by side. Push down on the counter to watch the pocket compress. Any significant asymmetry should be a signal to replace the shoes. Rock the shoe on the counter back and forth, noting any excessive or asymmetrical roll (1).
Insole
This removable portion of the shoe is extremely variable and interchangeable. The quality of insoles has improved over the years for shoes that demand more shock absorption and support. However, a broken-down insole does little for the athlete, and its condition should be evaluated at the time of any foot and ankle injury. Note the elastic energy-absorbing properties of the forefoot and hindfoot, as well as the medial support along the arch. Many times, a shoe that claims to be motion control has only a built-up medial insole that breaks down after mild wear.
Examination of the insole can shed light on foot mechanics. Look at the impression on the sole and see how centered it is. A lateral impression implies a foot too rectus (straight) for the shoe, while a medial impression suggests an adductus (curved) foot. Note abnormal wear patterns, specifically at the MTP joints. The deepest impression should be near the first MTP, through which almost 60% of the body weight is transferred. Deeper impressions elsewhere may indicate abnormal weight distribution from poor foot biomechanics or other structural problems (equinus, pes cavus or planus).
Midsole
The midsole is between the forefoot and the counter/hindfoot. Its primary job is to provide stability and cushion. Take the shoe with one hand on the counter and the other on the forefoot. Twist the shoe forefoot clockwise, hindfoot counterclockwise and then the other way and look for excessive motion. A strong midsole should be stiff and resist twisting. A weak midsole, by design or breakdown, causes the counter to excessively invert and evert.
The material that makes up the midsole affects stability and shock absorption. A denser midsole gives stability and support, while a lowerdensity midsole absorbs more shock. Again, the athlete should define his or her needs, and then choose the shoe and the material appropriately. Some shoes are made with little midfoot support, so athletes should be educated about what they need from shoes. The wrong shoe can lead to needless injury.
Outsole
The outsole is the tread of the shoe that holds the athlete to the ground (Fig. 24.2.3). Many types of outsoles exist, so the athlete needs to choose the appropriate one for the playing surface. For instance, waffle patterns on the outsole work better on softer surfaces, so this type of shoe on a harder surface like concrete would wear down much faster. The types of material used in outsoles differ as well. Carbon outsoles are harder and more durable, while “blown” rubber is softer and more giving, yet less durable.
Note the type of outsole the athlete wears and consider the desired activities.
Note the type of outsole the athlete wears and consider the desired activities.
Look for wear on the outsole, including the pattern, amount, and its distribution. Specific areas of wear may lead to problems. For instance, heel wear is typically seen lateral to the midline. This is not abnormal, but if the heel wear is excessive, the counter may evert too much during gait, destabilizing the ankle and stressing the supportive soft tissue. Excess toe wear can be seen on the outsoles of sprinters, but it may also correlate with a possible equinus contracture.
Wear patterns can identify flaws in biomechanics. A worn lateral outsole indicates that the foot stays inverted and supinated during gait. It may also indicate a narrow base, where the feet are too close during gait, or hindfoot varus. On the other hand, excessive medial outsole wear comes from a heavy pronator with a widened base of gait. The medial shoe will typically collapse quicker, leading to abnormal wear. Asymmetrical wear between the left and right shoes may indicate a leg-length discrepancy.
The outsole itself may be the primary source of injury. The waffle tread on some insoles may have a prominent stud located under a sesamoid or a sensitive part of the foot, focusing enough pressure to inflame the foot. Structural flaws can form from even minimal use or may be present at purchase.
FOOT AND ANKLE OBSERVATION
Look first at the athlete’s posture while standing and perform a static assessment. Note asymmetries in size, swelling, skin coloring, and shape. Make sure the bony and tendon landmarks are visible and within normal limits.
Look for any skin lesions, such as tinea pedis, nevi, and onychomycosis. Discoloration at the distal toes may indicate ill-fitting shoes. If the athlete is diabetic, the foot must always be examined at every physician visit and checked for discolored lesions and circulation.
Alignment is crucial. Note deviations in the toes and contact points among them. “Hammer toes” can be painful and affect performance, so early detection is helpful. Hallux adductus, especially in the first MTP, leads to bunion formation. Note the callus pattern, for it indicates weight distribution. Skin changes along the medial first MTP joint may signify a friction point and the beginning of a bunion.
Note the hindfoot and its position in reference to the forefoot. The heel may move into valgus or varus upon stance. The arch may be high (cavus) with a rigid supinated foot, or low (planus) with a flexible pronated foot. The forefoot may be rectus (straight) or adductus (curved), which can play a factor in injury if the athlete wears wrong-fitting shoes.
To observe pronation, have the athlete walk away and toward you without socks, shoes, and long pants. Look for depression or collapsing of the arch, rotation of the talus, and shifting of the calcaneus into valgus or varus alignment. More discussion on gait analysis can be found in Chapter 25.
PALPATION
Note the bony landmarks and assess for tissue texture changes and tenderness. Progress systematically, from distal to proximal, or vice versa. Structures to always include in the palpatory examination are the medial and lateral malleoli, calcaneus, fifth metatarsal base, first MTP joint, and the medial plantar fascia insertion on the calcaneus.
In the forefoot, palpate the MTP joints and the distal interphalangeal and proximal interphalangeal joints, noting swelling and tenderness. Palpate along the shafts of the metatarsals and their interspaces. Fullness and tenderness between the third and fourth metatarsal shafts may indicate Morton’s neuroma.
Midfoot sprains can be debilitating and lead to long-term consequences, so palpate the first and second metatarso-cuneiform joints, noting swelling, bogginess, and tenderness on both the dorsal and plantar sides. Moving more proximally, palpate the calcaneocuboid and talonavicular joints. Also find the tarsal navicular tubercle, as the posterior tibialis tendon inserts there.
Note the sinus tarsi location and check for tenderness (Fig. 24.2.4). Sinus tarsi syndrome can be overlooked if the examination is incomplete. Areas of possible impingement are the region anterolateral to the lateral malleolus and the anteromedial talus region (Fig. 24.2.5). Palpate these areas for tenderness or tissue changes.
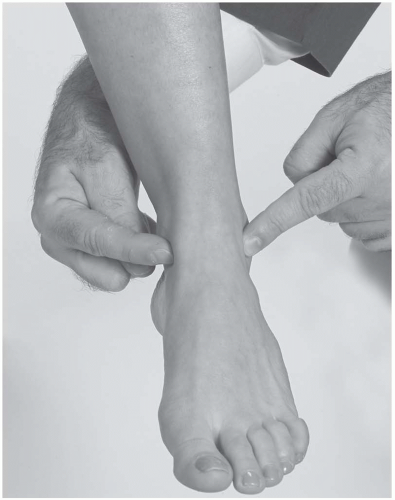
Palpate the lateral (anterior and posterior talofibular, calcaneofibular) (Fig. 24.2.6) and medial deltoid ligaments of the ankle (Fig. 24.2.7). Note any tissue bogginess or swelling, remembering that normal ligaments are not tender to palpation. Move your fingers
toward the anterior aspect and check the syndesmosis, medial to lateral, distal to proximal.
toward the anterior aspect and check the syndesmosis, medial to lateral, distal to proximal.
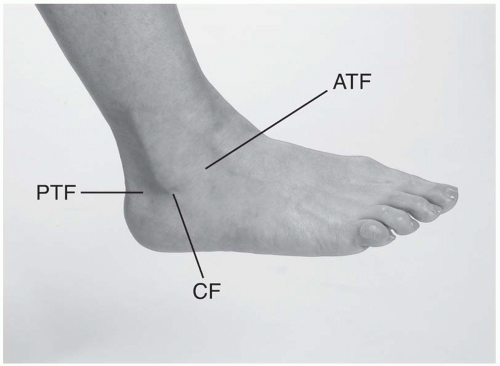 FIGURE 24.2.6. Lateral ligaments of the ankle. ATF, anterior talofibular; PTF, posterior talofibular; CF, calcaneofibular. |
Feel along the tendons and their sheaths, specifically the Achilles, peroneal, and posterior tibialis tendons. Note swelling, defects, and tenderness. Pay close attention to the tarsal tunnel and its structures.
RANGE OF MOTION
Active range of motion (ROM). Active ROM is assessed with athlete sitting on the table with the legs hanging over side. The examiner asks the athlete to move the foot into plantarflexion, dorsiflexion, inversion, and eversion.
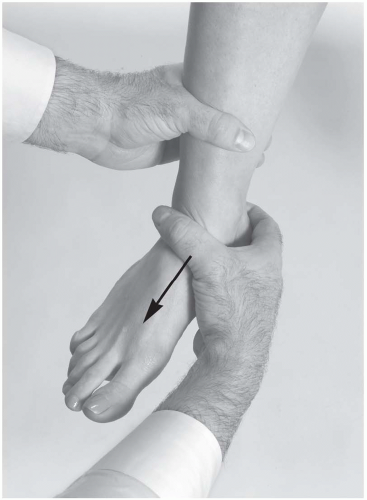
Passive range of motion (Table 24.2.1). Passive ROM is assessed with athlete sitting and the ankles relaxed. The same motions as above are checked (Fig. 24.2.8A to D). The examiner stabilizes the distal tibia with one hand while the other hand maneuvers the foot.
Equinus contracture. The ankle cannot achieve neutral dorsiflexion, so the foot stays more in some degree of plantarflexion. This triggers a cascade of biomechanical decompensation. Causes include neurogenic (cerebral palsy, neurapraxia), gastrocnemius or soleus injury, prolonged immobilization in plantarflexion, and surgical repair of the Achilles.
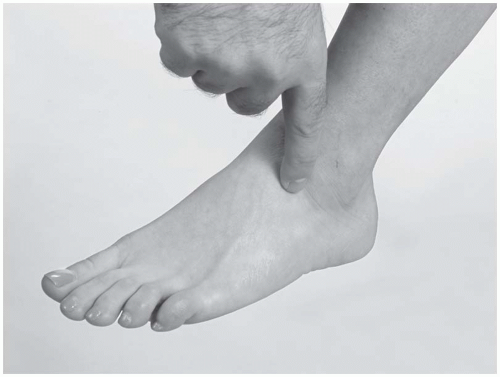
Subtalar motion. The athlete lies prone with the knee flexed to 135 degrees. The foot is brought into dorsiflexion, then moved through inversion and eversion. Overall motion at the joint is approximately only 10 to 20 degrees (Fig. 24.2.9).
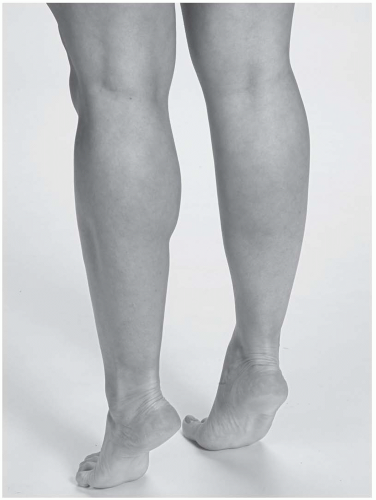
Inversion of the subtalar joint. The athlete stands and rises on his or her heels. The heel will promptly invert, the longitudinal arch will rise, and the leg will rotate externally if the foot is functioning normally (Fig. 24.2.10).
Eversion of the subtalar joint. The athlete stands as the examiner observes him or her from behind to evaluate the tilt of the calcaneus. The calcaneus should slant to one side. If the calcaneus tilts inward, this is considered hindfoot valgus. The tarsal navicular is dorsiflexed and abducted on the head of the talus. The forefoot is supinated in relationship to the hindfoot.
TABLE 24.2.1. AVERAGE PASSIVE RANGES OF MOTION FOR ANKLE | ||||
|---|---|---|---|---|
|
NEUROVASCULAR EXAMINATIONS
Pulses. The examiner uses the pad of the index finger to palpate the dorsalis pedis and posterior tibial pulses. The dorsalis pedis is on the dorsal side of the foot around the anterior talar neck, while the posterior tibial artery is found in the tarsal tunnel.
Muscle Strength
Anterior tibialis (deep peroneal nerve, L4, L5). With the athlete supine or sitting, the examiner resists ankle dorsiflexion while stabilizing the distal leg.
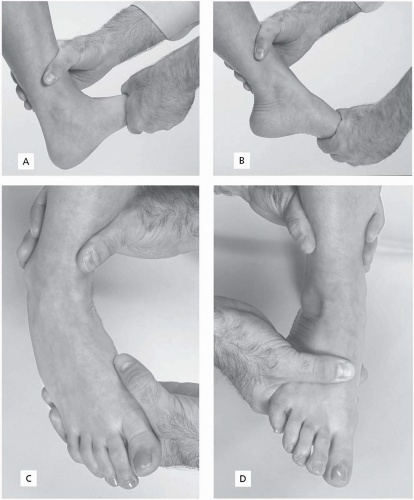 FIGURE 24.2.8. Passive range of motion. A, Dorsiflexion; B, plantarflexion; C, inversion; D, eversion. |
Note: The following tests can be done with the athlete sitting up on the edge of a table.
3. Soleus (tibial nerve, S1, S2). With the athlete sitting on the edge of a table with the leg hanging, plantarflexion is again tested against the examiner’s resistance.
4. Posterior tibialis
For gross muscle function, have the athlete walk on his or her toes around the room. Any deficiency should be visible, either by pain, inability to stay up, or exaggerated pronation.
While the athlete is sitting, bring the foot into eversion or neutral and resist inversion.
5. Peroneus longus and brevus (superficial peroneal nerve, S1). With the foot hanging from a table, the foot is brought into inversion and the athlete everts against the examiner’s resistance.
6. Flexor hallucis longus (tibial nerve, L5). The examiner resists first MTP plantar flexion with one hand while securing the calcaneus with the other.
7. Extensor hallucis longus (deep peroneal nerve, L5). The examiner resists first MTP dorsiflexion with one hand while securing the calcaneus with the other.
8. Extensor digitorum longus. (deep peroneal nerve, L5). The examiner controls the calcaneus with one hand and resists dorsiflexion of the second through fifth digits.
9. Flexor digitorum longus (tibial nerve, L5). The examiner controls the calcaneus with one hand and resists plantar flexion of the second through fifth digits.
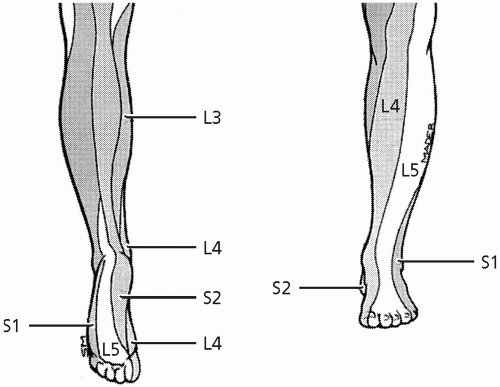
Sensorium
L4: medial side of the foot extending to the medial first MTP joint.
L5: dorsum of the foot from the great toe to the fourth toe.
S1: lateral foot and dorsum of the fifth toe.
Reflexes
Achilles (S1). While the athlete sits on a table edge, the examiner holds the forefoot and gently dorsiflexes the foot. The other hand uses a reflex hammer to tap the midportion of the Achilles tendon gently.
If the ankle or tendon is too tender to tap, bring the foot into dorsiflexion with the examiner’s finger pads pushing against the MTPs
on the plantar side, then strike the fingers. This is best done with the athlete prone.
on the plantar side, then strike the fingers. This is best done with the athlete prone.
Stability
Anterior Drawer Test. The athlete sits on the edge of a table while the examiner, facing the athlete, controls the distal leg with a stabilizing hand. The mobilizing hand grasps the calcaneus posteriorly, while the thumb is placed over the anterior talus (in some cases, the thumb can be free if the examiner is comfortable controlling the calcaneus posteriorly). The examiner translates the calcaneus and talus in an anterior direction, noting laxity, end point, and pain (Fig. 24.2.12).
Positive test: Excessive anterior laxity and soft end point, particularly compared with the opposite ankle.
Indicates: Disruption of the anterior talofibular ligament.
Talar Tilt Test. The athlete and the examiner are in the same position as for the anterior drawer, but the mobilizing hand holds the calcaneus from the inferior direction, one finger on the lateral talus to monitor motion. The ankle has 10 to 20 degrees of plantarflexion. The examiner then inverts the talus to its end point of motion. The examiner must be careful not to invert the foot, as subtalar motion will be assessed (Fig. 24.2.13).
Additional Tests. Bilateral mortise view radiographs can be taken with the talus stressed in inversion. The tilt angle is measured and compared.
Positive test. Excessive tilt, particularly compared with opposite foot, more than 2-mm difference in tilt on radiographs.
Indicates. Anterior talofibular (ATF) and calcaneofibular (CF) ligament disruption.
Note: Increases in talar tilt usually occur with both ATF and CF disruption. When the ankle is injured in dorsiflexion, the ATF ruptures primarily, and the CF secondarily. Isolated CF injuries rarely cause increased talar laxity.
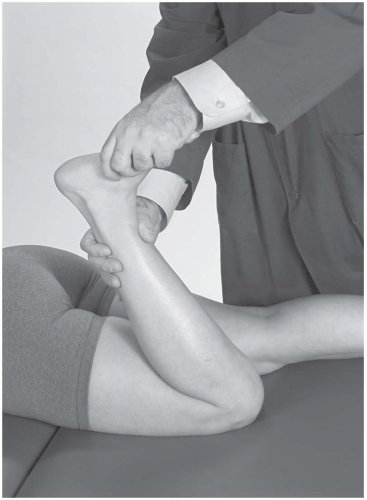
Eversion Test. The examiner holds the athlete in the same position as for the talar tilt test. With the proximal hand stabilizing the tibia, the opposite hand holds the midfoot from the plantar aspect and everts up to the anatomic barrier (Fig. 24.2.14).
Positive test: Pain with end range of motion into eversion, increased laxity compared with the opposite side; results should be correlated with palpation of the medial ankle.
Indicates: Medial deltoid ligament injury or disruption.
External Rotation Stress Test. With the foot and leg held in the same position as for the talar tilt test, the examiner externally rotates the foot against a stabilized lower leg. The idea is to force the talus to rotate as well, stressing the tibiofibular joint (4).
Positive test: Pain along the syndesmosis or medial ankle.
Indicates: Syndesmotic injury or disruption, injury to the deep fibers of the medial deltoid ligament.
Peroneal Tendon Stability Test. The examiner holds the athlete’s foot with one hand, while the opposite hand gently palpates the peroneal tendons just posterior to the lateral malleolus. The examiner moves the foot into end-range inversion, then asks the athlete to evert against
resistance. The other hand monitors the peroneal tendon (Fig. 24.2.15).
resistance. The other hand monitors the peroneal tendon (Fig. 24.2.15).
 FIGURE 24.2.14. Eversion test.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|