5 The elbow
CHAPTER CONTENTS
Introduction
Epidemiological studies have reported that incidence of elbow pain in the general population is between 8 and 12% (Korthals-de Bos et al 2004). The elbow has proved to be the poor relation in terms of academic investigation as, other than in tennis elbow (TE), there is a paucity of literature regarding evidence-based management of elbow pathology. In considering the role of manual therapy in the treatment of elbow pathology, the therapist must often rely on what is understood regarding the pathophysiology of common elbow conditions, rather than evidence-based treatment strategies; these continue to remain elusive in the majority of elbow conditions. This may reflect the relatively low incidence of elbow pathology in comparison to conditions affecting the spine, knee, and shoulder, and the natural history of many elbow conditions. Elbow fractures account for only 7% of all fractures and reports suggest that half of all cases of cubital tunnel syndrome and ulnar neuropathy will resolve spontaneously (Walker-Bone et al 2004). However, the socioeconomic implications of conditions such as TE cannot be underestimated, and an emphasis must be placed on the importance of both understanding and optimizing the role of the manual therapist in managing this type of condition. Whilst there is currently limited evidence to support the efficacy of manual therapy in most elbow pathologies, modern advances in pain science and an increased understanding of the physiological effects of manual therapy techniques will guide future research.
Tennis elbow or lateral epicondylalgia (LE) is the second most frequently diagnosed musculoskeletal disorder of the neck and upper limb in a primary care setting, with an annual incidence of 4 to 7 cases per 1000 patients in general practice (Smidt et al 2003). Whilst over 40 different conservative treatment approaches have been described in the literature, the medical fraternity still tends to adopt a wait-and-see policy (Smidt et al 2002). This results from the failure of methodologically rigorous trials to demonstrate any long-term benefit of conservative interventions (Smidt et al 2003). There is, however, good evidence to support a short-term benefit from conservative interventions (Bisset et al 2005); from both a physiotherapist and patient perspective, this is significant in terms of return to function and reducing the socioeconomic impact of this challenging condition. The lack of consensus regarding nomenclature in LE reflects our increasing understanding regarding the underlying pathophysiological processes. Authors have reported the absence of inflammatory mediators in patients with LE (Alfredson et al 2000), thus emphasizing the importance of moving away from misleading terminology, such as LE, and questioning the role of anti-inflammatory modalities. Furthermore, the appreciation that a key aspect of this condition is an underlying tendinopathy in the common extensor tendon suggests that terms such as lateral epicondyle tendinopathy may be more appropriate (Coombes et al 2009). However, it is clear from what we currently understand regarding LE pathophysiology in terms of local tendon pathology, abnormalities in the pain system (peripheral and central), and impairments in the motor system (local and global) that the modern manual therapist is well placed to implement effective treatment strategies.
Manual therapy for the relief of pain
High levels of pain and functional disability have been reported in patients with LE and are the principal reasons that they seek treatment (Alizadehkhaiyat et al 2007a). Clinical trials commonly measure pain-free grip strength and pressure-pain thresholds as markers of improvement in pain levels in this patient group. Pain-free grip has been shown to be a valid and sensitive marker in measuring outcome in patients with LE, and correlates well with patients’ perceived outcome (Pienimaki et al 2002). Active trigger points have been well described in the forearm muscles of patients with LE and are believed to be indicative of peripheral sensitization; however, the presence of latent trigger points in the unaffected side of patients with unilateral LE is also suggestive of central sensitization processes (Fernández-Carnero et al 2008a).
The link between the cervical and thoracic spine and LE remains controversial. Authors have suggested that the pain associated with LE may relate to altered neuronal afferent input to the spine (Fernández-Carnero et al 2008b). It is difficult to elucidate the true nature of this relationship because many studies of LE exclude patients with significant cervical spine signs; however, investigations of study methodologies often reveal that this exclusion is based on reported symptomology rather than objective findings. In their study of patients with LE and a control group, Berglund et al (2008) reported that 70% of subjects with lateral elbow pain indicated pain in the cervical or thoracic spine, as compared to 16% in the control group. These patients also had a significantly increased frequency of pain response to the neurodynamic test of the radial nerve (p < 0.001). The above authors concluded that the cervical and thoracic spine should be included in the assessment of patients with lateral elbow pain.
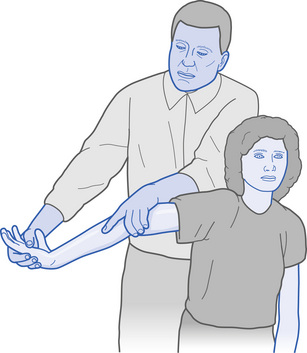
The role of manual therapy techniques directed to the cervical spine in order to address pain in patients with LE remains unclear. Studies commonly fail to control for the natural history of the disorder and therefore compromise extrapolation of meaningful results. However, several studies have reported that mobilization techniques applied to the cervical spine in patients with LE produce a significant hypoalgesic effect and a concomitant sympathoexcitatory response at the elbow when compared to placebo or control groups (Vicenzino et al 2007). A pilot study by Vicenzino et al (1996) showed that patients treated with mobilization of the cervical spine, versus local elbow treatment, showed superior results in terms of pain-free grip strength and Disabilities of the Arm, Shoulder and Head (DASH) (Gummesson et al 2003) scores. A retrospective review by Cleland et al (2004) suggested that patients who received cervicothoracic mobilization, in addition to local treatment, require significantly fewer visits to achieve similar success rates in terms of pain relief and pain-free grip strength. In terms of specific manual therapy techniques, the cervical lateral glide technique has been shown to achieve significant improvements in pressure-pain threshold and an increase in pain-free grip strength, as well as the production of a sympathoexcitatory response across sudomotor, cutaneous, and vasomotor functions (Fig. 5.1). To date, this has only been demonstrated immediately after application of the technique (Vicenzino et al 2001).
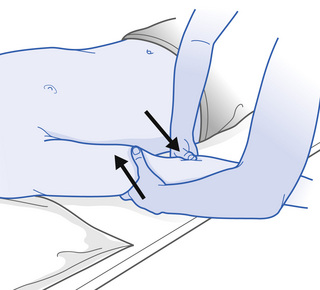
The role of locally directed manual therapy techniques, such as mobilizations with movement (MWM) (see Fig 5.1), in the management of LE have been explored in several studies (Abbott et al 2001; Paungmali et al 2003). To perform the MWM technique, the therapist identifies a pain-provoking activity, which commonly involves the patient clenching their fist. This is then repeated while the therapist performs a laterally directed glide to the elbow. The direction in which the lateral glide is applied and the force with which it is applied are important in maximizing the hypoalgesic effect. Studies reporting the efficacy of this technique stress the importance of the procedure being performed as part of a home exercise programme between treatments (Bissett et al 2006a). A single MWM treatment has been shown to result in an immediate increase in pain-free grip strength. An initial reduction in pressure-pain thresholds over the lateral epicondyle and evidence of sympathetic excitation have also been reported. There is good evidence that MWM combined with an exercise programme has superior short-term effects in terms of pain, as measured by a visual analogue scale (VAS) versus exercise alone (Vicenzino et al 2007). This treatment approach (i.e. a combination of MWM and exercise) appears to be more effective than corticosteroid injection and crucially, wait-and-see over a 12-month period. In Bisset et al’s (2006a) study, pain-free grip was optimally improved over the entire year; patients were apparently more satisfied and reported fewer recurrences. This was the first study to demonstrate a significant difference in longer term outcomes using a combination of exercise and manual therapy.
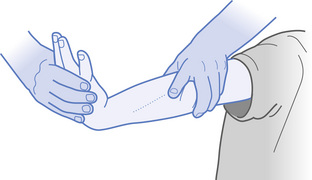
Whilst MWM combined with exercise has been the most researched manual therapy technique in LE, Cyriax (1945) claimed substantial success in treating TE using deep transverse friction (DTF) in combination with Mill’s manipulation (Verhaar et al 1995) (Figs 5.2 and 5.3).
Cyriax (1945) stressed that in order to be considered a Cyriax intervention, the two components must be used together in the correct order and that patients must follow the protocol three times a week for 4 weeks. Despite this clear stipulation, only one study has been reported in which true Cyriax physiotherapy was used in the management of TE. Verhaar et al (1995) compared the effects of corticosteroid injections with Cyriax physiotherapy in treating patients with this condition. The results showed that the corticosteroid injection was significantly more effective on the outcome measures (i.e. pain, function, grip strength, and global assessment) than Cyriax physiotherapy at the end of the treatment, but at the follow-up one year after the end of treatment, there were no significant differences between the two treatment groups. Other studies have only examined the efficacy of one aspect of the Cyriax approach and have failed to demonstrate any significant treatment effect.
Current evidence suggests that manual therapy techniques such as cervical lateral glide and MWM have short-term efficacy in improving pain-free grip strength and pressure-pain threshold (Vicenzino et al 2007). There is limited evidence that manual therapy combined with exercise may have better long-term outcomes than injection or exercise alone. Vicenzino et al (2007) suggested that manual therapists should consider whether patients have greater deficits in pain-free grip measurements or pressure-pain threshold, during patient assessment. Those patients with greater deficits in pain-free grip strength may be the most appropriate candidates for MWM techniques directed at the elbow, since this is where they have been shown to have their greatest effect. Conversely, the above authors suggested that subjects with greater pressure-pain threshold deficits, relative to pain-free grip force deficits, should be treated with techniques directed at the cervical spine. Whilst this proposed classification system is based on current evidence, it requires further validation, but it does emphasize the importance of a thorough assessment that includes the cervical and thoracic spine, together with specific local palpation and testing in LE.
Manual therapy to improve joint movement
Consideration of the role of manual therapy in the management of the post-traumatic elbow has been hindered historically by the long-held belief that inappropriate mobilization can predispose the joint to the development of heterotrophic ossification (HO). A review of the literature advocating that passive mobilization should not be performed reveals that most opinion has been based on animal studies that employed forcible passive mobilization (Casavant & Hastings 2006); this is not reflective of manual therapy techniques performed by therapists on this type of patient. Furthermore, much of the literature is anecdotal, purely based on expert opinion, or lacks methodological rigour. In reality, there are several papers that advocate the use of passive range of movement (PROM) exercises. Crucially, these have demonstrated that, in fact, there is no significant difference between groups that are mobilized and those that are not in terms of HO formation. Furthermore, those patients with demonstrated HO do not show a worsening or increase in formation if subjected to a passive mobilization regime (Casavant & Hastings 2006; Issak & Egol 2006). Consequently, patients at risk of developing post-traumatic stiffness should have appropriate physiotherapy intervention incorporating relevant mobilization techniques. However, more work is required to identify the optimal strategies for mobilization in this patient group.
Reduction in shoulder external rotation range of movement (ROM) has been reported in patients with LE. Abbot (2001) showed that MWM applied to the elbow results in an increase in the external rotation ROM at the shoulder. The above author suggested that this observation indicates that MWM cause a neurophysiologically mediated decrease in resting muscle tone. This observation further emphasizes the importance of a thorough assessment incorporating the shoulder joint in patients with LE.
Manual therapy to normalize muscle function
The main histopathological feature demonstrated in LE is that of a tendinopathy involving the common wrist extensor origin (Fedorczyk 2006). Microscopic and histology studies have identified angiofibroblastic hyperplasia and a consistent absence of inflammatory cells. These findings are consistent with those demonstrated in achilles and patellar tendinopathies. Manual therapists have long recognized the role of mechanical load in affecting the synthesis and degradation of collagen and influencing tendon remodelling (Mackay et al 2008). Eccentric loading programmes are well described in achilles and patellar tendinopathies (Woodley et al 2007). Despite this, the limited evidence available suggests that eccentric exercise is no better than other standard physiotherapy treatments for chronic lateral epicondylar tendinopathy (or LE) (Croisier et al 2007; Manias & Stasinopoulos 2006; Svernlov & Adolfson 2001). Pathological changes have been demonstrated in both the deep and anterior fibres of the extensor carpi radialis brevis (ECRB) tendon insertion; the ECRB enthesis has extensive attachments to the lateral epicondyle, intramuscular septum, and lateral collateral ligament that are believed to help the dissipation of stress. Tensile, compressive, and shear forces will be specific to the structure and function of this tendon–fibre arrangement, and therefore may necessitate a specific loading approach.
Pain-free grip strength is reduced in LE by an average of 43 to 64% when compared to the unaffected side (Coombes et al 2009). Flexor and extensor deficits have been observed in the wrist and hand of patients with LE when compared to healthy controls (Alizadehkhaiyat et al 2007b). However, metacarpophalangeal extensor strength is not affected. This may reflect a compensation strategy where patients maintain or increase finger extension strength to compensate for the weakness observed in the wrist extensors. As previously discussed there is some limited evidence that a combination of manual therapy directed to the elbow (MWM) and exercise results in short-term improvements in pain-free grip strength.
Electromyographic (EMG) studies have demonstrated a global weakness in the upper limb of patients suffering from LE that affects not only the wrist flexors and extensors, but also the shoulder abductors and external rotators. It is not currently clear whether this is causative or results from the underlying LE. Nevertheless, this does emphasize the importance of addressing global upper limb function in the rehabilitation of patients with LE. Alizadehkhaiyat et al (2009) demonstrated that, even in those patients who reported resolution of symptoms, EMG and strength measurements indicated incomplete functional recovery. The above authors found significant ongoing deficits in global upper limb strength compared to controls. There was no difference between symptomatic LE and those patients with recovered LE. Currently, there is a little evidence regarding the significance of the global upper limb dysfunction and whether it plays a role in recurrence. However, when advising the therapist to employ evidence-based approach to rehabilitation it is important to consider the relevance of global upper limb strength in optimizing muscle function.
Manual therapy and motor retraining
Investigators have suggested that the greater prevalence of LE in novice tennis players than in expert players may reflect the novice’s use of faulty mechanics for certain strokes. Wrist kinematic and EMG data have shown that novice players eccentrically contract their wrist extensor muscles throughout the stroke (Kelley et al 1994). Furthermore, studies have suggested that recreational tennis players transmit more shock impact from their racket to the elbow joint, and use larger wrist flexor and extensor EMG activities during the follow-through phase of the backhand stroke. This is of relevance as follow-through control has been proposed as a critical factor for reduction of shock transmission. Specific differences in ECRB activation levels have been demonstrated in tennis players with LE, compared to asymptomatic players. It is significant that similar abnormal patterns of activation in the common flexor muscles have been observed in golfers with medial epicondylalgia symptoms (Glazebrook et al 1994). Understanding these abnormalities in motor strategies may help us to elucidate predisposing factors for the development of LE and also examine key factors in other at risk populations. To date, however, there is a lack of evidence to demonstrate either how best to address these abnormalities or, crucially, whether addressing them results in symptoms relief. Nevertheless, Alizadehkhaiyat et al (2009) have demonstrated reduced ECRB activity in patients with LE during isometric wrist extension and gripping tasks, which appears to resolve in subjects who have recovered LE. Whether this change in muscle activation results from the resolution of pain or other factors has not been elucidated in this patient group.
Bisset et al (2006b) described the presence of bilateral sensorimotor deficits in patients with LE compared to healthy controls. These deficits remained relatively unchanged despite treatment intervention (Bisset et al 2009). The treatment strategies employed in this later study did not specifically address sensorimotor deficits; however, patients reported improvements in pain-pressure threshold and pain-free grip strength despite the lack of improvement in sensorimotor function. In view of what we understand regarding the influence of sensorimotor deficits on muscle timing, this is commensurate with the alterations observed in motor control in this patient group. However, it is currently not clear what role this plays in the pathophysiology of LE.
Conclusion
It is clear from the literature that there is some limited evidence to support the use of manual therapy combined with exercise to improve pain-free grip strength and pain-pressure threshold in the short term in patients undergoing treatment for LE. Whilst studies have investigated the use of different exercise approaches there is little evidence to support the superiority of one over another. Furthermore, most researchers have failed to investigate the role of therapeutic exercise alone compared to a control or no intervention. However, there is increasing evidence that current strategies may not acknowledge what is understood regarding sensorimotor deficits and global upper limb dysfunction. In an effort to ensure best practice, it is crucial that manual therapists are familiar with the current evidence regarding the pathophysiology of LE and complete a thorough assessment addressing the key areas discussed to facilitate the implementation of appropriate management strategies. The paucity of evidence to guide the management of other elbow pathologies highlights key areas for future research.
5.1 Acupuncture and elbow dysfunction
The hypothesis that Lateral Epicondylagia (LE) may be the result of a chronic tissue injury with sympathetic involvement is accepted on the basis that healing failed to proceed through the orderly and timely process outlined by Keast and Orsted (1998), failing to produce anatomical integrity and occupational capabilities (Kitchen & Young 2002). In addition, the fourth decade of life predisposes tendon injury through degenerative processes (Hong et al 2004; Khan et al 2002). Occupational strain (Walker-Bone & Cooper 2005) and repetitive upper extremity use are causative factors associated with inadequate tissue healing and chronic states (Pascarelli & Hsu 2001; Waugh et al 2004).
Pain is an inhibitory mechanism, preventing normal function (Chilton 1997; Pomeranz 1996; Trinh et al 2004); therefore, attaining some relief from the primary symptom (pain), secondary improvements in function are plausible. Many physical therapies have been employed both in isolation and in combination in the management of chronic LE including, exercise, manipulation and mobilizations, orthotics and taping, laser, and extracorporeal shock wave therapy. The most recent systematic reviews (Bisset et al 2005; Buchbinder et al 2006) suggest a lack of evidence for the long-term benefit of physical interventions over that of a placebo group.
It has been estimated that there is an average of 12 weeks absenteeism in 30% of those affected by LE (Beller et al 2005). This highlights the importance of selecting the most effective means to manage pain effectively. A review of the current limited available literature and recent trials demonstrates that there is contradictory supporting evidence for the use of acupuncture in the treatment of LE. Brattberg (1983) compared the efficacy of acupuncture versus steroid injections in the treatment of this condition, indicating 62% of patients reported a positive outcome of no pain or much improved pain levels after acupuncture intervention in comparison to 31% who received steroid injections. However, it is unclear from the results how many steroid injections were administered, or what type of steroid was used. Brattberg’s (1983) acupuncture group also appeared to have had a longer duration of symptoms prior to treatment, which may well have influenced their response and expectations of treatment.
Molsberger and Hille (1994) studied the immediate analgesic effect of acupuncture with placebo acupuncture for LE in 48 patients. After treatment, 79% of the acupuncture group reported pain relief of at least 50%, but only 25% of the placebo group. This may support the use of acupuncture for an immediate analgesic effect; however, the sample used by the above authors were volunteers, and 50% had expressed a positive expected outcome for acupuncture prior to the study. The main outcome measurement in this study was a subjective measurement of pain; therefore, coupled with the possible influence of bias from treatment expectations, limitations in bias were demonstrated. The acupuncture group were also asked to have carried out elbow movements during treatment, whereas the placebo group were not. It is unclear what these movements were and whether this has an extra influence over the placebo group.
Fink et al (2002a) measured the clinical effectiveness of acupuncture for chronic LE by comparing real acupuncture versus sham. An initial significant reduction in pain was noted for the real acupuncture group and an increase in function over a longer duration was also highlighted in these patients. It is also of interest that both groups had a mixture of subjects with repetitive and non-strenuous occupations, and both subgroups had similar improvements. This provides further limited support for acupuncture again for initial pain relief, but with some longer term functional improvement. It also indicates its effective use in patients, regardless of the daily level of activities of the involved upper limb. The initial pain improvements could be attributed to the nature of the course of the condition or the prolonged sessions of treatment.
Following a systematic review, Trinh et al (2004) concluded that acupuncture has a role in the management of pain but mainly in the short-term relief of lateral elbow pain. However, a Cochrane review by Green et al (2002) stated that acupuncture was limited in its effects with no relief lasting longer than 24 hours after treatment. Nevertheless, these findings still indicate acupuncture is effective for initial pain management and as a precursor to rehabilitation.
The lack of consensus regarding the management of this condition presents scope for further investigation into symptomatic relief and functional improvement.
Acupuncture is recognized in the Western world as a useful complementary medicine procedure (NIHCC 1998). Clinically, its uses have been recognized in the relief of acute pain following surgery (Suzuki et al 2002; Taguchi 2008), as well as for long-term relief from chronic pain following carpal tunnel syndrome (Napadow et al 2007), knee osteoarthritis (Selfe & Taylor 2008), shoulder pain (Filshie 2005), and chronic low back pain (Haake et al 2007). Research has indicated that acupuncture intervention for the relief of pain (Chilton 1997; Tsui & Leung 2002) and management of dysfunction (Fink et al 2002a) may be beneficial in the treatment of LE, provided that attention to the predominant pain presentation and tissue-healing time scales are taken into consideration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree