The Elbow 
The elbow is a highly congruent hinge joint that is stabilized by its bony configuration, as well as ligamentous and capsular structures. It is composed of three distinct articulations, which are enveloped by a common synovial-lined capsule. These include the following:
 The ulnohumeral joint, a near-uniaxial hinge articulation, which is constituted by the trochlea of the humerus and the trochlear notch of the ulna, and bears ~40% of the forces.
The ulnohumeral joint, a near-uniaxial hinge articulation, which is constituted by the trochlea of the humerus and the trochlear notch of the ulna, and bears ~40% of the forces.
 The radiohumeral joint, which is formed by the radial head and the capitellum of the humerus, and bears ~60% of the forces.
The radiohumeral joint, which is formed by the radial head and the capitellum of the humerus, and bears ~60% of the forces.
 The proximal radioulnar joint, a pivot-type articulation, which is composed of the radial head the radial notch of the ulna.
The proximal radioulnar joint, a pivot-type articulation, which is composed of the radial head the radial notch of the ulna.
Supplemented by a limited number of strong ligaments, the above anatomy provides excellent static stabilization, whereas more than 20 associated muscles provide dynamic stabilization. The above complex configuration allows forearm flexion and extension, as well as pronation and supination, thereby enabling the hand to perform various skilled and precise motions.
The hyaline cartilage covers (1) the circumference of the radial head, being relatively thin at its anterolateral aspect (which is thought to predispose to radial fractures in this location in elbow subluxations/dislocations); (2) the trochlea over an arc of approximately 330 degrees, except at the longitudinally coursing anteriorly located trochlear ridge and sulcus; and (3) the capitellum, except at its posterior aspect, referred to as the bare area or pseudodefect. The fibrous capsule ensheaths the articulating surfaces of the elbow and creates (1) an anterior recess, which extends from the anterior surface of the trochlea and capitellum to the radial and coronoid fossae; (2) a posterior (olecranon) recess, which is more capacious, and extends from the distal humerus to the radius and ulna around the olecranon process; and (3) an annular recess, which surrounds the radial neck, and represents the most distal extension of the synovial cavity.
The elbow is susceptible to a variety of injuries because of the excessive forces that are generated and transferred to this joint during heavy (particularly arm weight-bearing) activities, especially in athletes involved in overhead throwing (particularly in racket sports). Compared to other joints, elbow is the second most frequently affected joint by overuse injuries. A systematic image analysis and structured reporting is essential for optimal diagnostic assessment of the elbow structures. This chapter discusses the imaging evaluation approach and describes how to fill in the structured checklist (Box 1). Conceptual details of related MR physics and imaging protocol are discussed in the chapter on MR protocol optimization.
 IMAGE EVALUATION
IMAGE EVALUATION
The below-outlined stepwise interpretation approach is only a practical guide, and all structures of the elbow should be evaluated in multiple planes for optimal assessment. This will also help readers perceive which structures are best depicted/evaluated on which particular plane.
1. Line up the similar-plane fat-saturated (fs) and non-fs images and synchronize them for tandem evaluation.
2. Start with the sagittal images to look for possible effusion in the elbow joint by interrogating the recesses described above. Subsequently, check for cartilaginous or osteochondral bodies and assess the bony alignment. Then, evaluate the triceps and biceps tendons for continuity, pathology, or abnormality of their attachment sites (e.g., olecranon bursitis, enthesopathy, avulsive cystic changes). Finally, check the cartilage and bone marrow for osteochondral lesions (OCLs) or ulnohumeral osteoarthritis. Far-lateral images are particularly suitable for assessing the lateral ulnar collateral ligament (LUCL).
3. In the coronal plane, check for asymmetric widening of posterolateral joint space, which may indicate underlying posterolateral instability. Moving from anterior to posterior images, interrogate the radial collateral ligament (RCL), the three bundles of the ulnar collateral ligament (UCL), and then evaluate the medial epicondyle, the overlying common flexor tendon (CFT) and the adjacent muscles. Moving to the lateral side, check for OCLs of the capitellum and trochlea, and then interrogate the lateral ligamentous and musculotendinous structures.
4. The axial plane is best for evaluating the peripheral nerves and assessing lesions of the biceps, brachialis, and triceps tendons. Axial images are also useful for evaluating the annular ligament, the posterior bundle of the UCL, the biceps tuberosity, and the bicipital radial bursa. The cubital tunnel, elbow vessels, and masses are also optimally evaluated in the axial plane.
 BOX 1: The Structured Report: Elbow
BOX 1: The Structured Report: Elbow
The checklist for structured reporting of MR imaging of the elbow. For each field, Normal, None, or Intact is considered default in the dictation, whereas the rest of the elements describe various pathologies that could be encountered during imaging evaluation. See Appendices 1 and 2 at the end of the chapter for a sample completed reports for normal and abnormal (positive) examination results.
MRI of Elbow
FINDINGS:
Alignment: [<Normal> / <Posterior subluxation> / <Dislocation>]
Joint fluid: [<None> <Small effusion> <Moderate effusion> <Large effusion>]
Intra-articular bodies: [<None> <Cartilaginous or Osteochondral bodies>]
Medial structures:
Ulnar collateral ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Common flexor tendon: [<Normal> <Tendinosis> <Partial tear (low/high grade)> <Complete tear>]
Medial epicondyle: [<Normal> <Enthesopathy> <Bone marrow edema>]
Lateral structures:
Radial collateral ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Lateral ulnar collateral ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Annular ligament: [<Intact> <Thickened> <Acute Sprain>]
Common extensor tendon: [<Normal> <Tendinosis> <Partial tear (low/high grade)><Complete tear>]
Lateral epicondyle: [<Normal> <Enthesopathy> <Bone marrow edema>]
Posterior structures:
Triceps: [<Normal> <Tendinosis> <Enthesopathy> <Partial tear> <Complete tear>]
Olecranon bursa: [<Normal> <Distended>]
Olecranon: [<Normal> <Enthesopathy> <Bone marrow edema>]
Anterior structures:
Biceps: [<Normal> <Tendinosis> <Tenosynovitis> <Partial tear> <Complete tear>]
Brachialis: [<Normal> <Tendinosis> <Tenosynovitis> <Partial tear> <Complete tear>]
Bicipitoradial bursa: [<Normal> <Distended>]
Articular:
Radiocapitellar joint: [<Normal> <Osteochondral lesion> <Osteoarthritis>]
Ulnohumeral joint: [<Normal> <Osteoarthritis>]
Proximal radioulnar joint: [<Normal> <Osteoarthritis>]
Bones: [<Normal>]
Muscles: [<Normal>]
Vessels: [<Normal>]
Nerves: [<Cubital tunnel normal> <Retinaculum deficient> <Hyperintense ulnar nerve>]
Other: [<None>]
Impression:
[<In the order of importance with acute findings first>]
 HOW TO FILL THE STRUCTURED REPORT
HOW TO FILL THE STRUCTURED REPORT
Alignment: [<Normal> <Posterior subluxation> <Dislocation>]
The evaluation of bony structures and bone alignment is best performed on non-fs images, since the latter provide clear depiction of the fatty marrow, bone cortex, and osteophytes. Normal alignment means bony articulation congruency at the ulnohumeral and proximal radioulnar joints. Generally, the central axis of the capitellum should continue distally as the axis of radial head and shaft in all positions and planes (radiocapitellar line), whereas the anterior humeral cortical line should cross the capitellum at the intersection of its anterior and middle thirds (anterior humeral line). Sagittal images are best for detecting subluxation or dislocation of the radiocapitellar joint and/or the ulnohumeral joint (perched trochlea) since in most cases the elbow misaligns posteriorly or posterolaterally (posterolateral rotary instability). The other malalignments may be related to anterior subluxation (rare and is usually associated with olecranon fracture), valgus instability (acute with UCL rupture with or without radial head fracture) or chronic overload (valgus extension overload syndrome due to attenuated anterior bundle of UCL, especially in throwing athletes), and varus instability (associated with rupture of RCL). Sagittal images are also suitable for evaluating associated entrapped osteochondral fracture fragments and assessing respective donor sites (medial epicondyle, radial head, coronoid process, and posterior capitellum). Anterior or medial elbow subluxation or dislocation is uncommon, seen in less than 10% cases.
Proximal radioulnar subluxation (or dislocation) is a relatively common injury in children and is caused a sudden pull on the extended pronated arm (nursemaid’s elbow). Imaging shows increased radiocapitellar distance with anterior displacement (subluxation) of the radial head out of the sigmoid notch of the ulna, along with tear and interposition of the annular ligament in the radiocapitellar space. In adults, the injury is additionally associated with complex lateral ligamentous injury and/or fracture.
Other useful anatomic relationships to evaluate clinically or on imaging include the carrying angle (normal range: 154–178 degrees in men, 158–178 degrees in women), which is formed by the axes of the arm and the forearm with the elbow in full extension, and the humeral angle (normal range: 77–95 degrees in men, 72–91 degrees in women), which is formed by the intersection of the long axis of the humerus and the transverse line drawn tangentially across the most distal points of the articular surfaces of the trochlea and capitellum.
JOINT FLUID:
Effusion: [<None> <Small effusion> <Moderate effusion> <Large effusion>]
Intra-articular body: [<None><Cartilaginous> <Osteochondral body>]
The elbow and proximal radioulnar joints have thin synovial lining and small amount of fluid for nutrition and lubrication, which does not normally distend (produce convex margins) the capsule. Joint effusion is established when there is capsular distention, a finding, which is usually more prominent at the anterior (non-dependent) portion of the capsule if imaging is performed in the “superman” position. When present, the joint effusion should be graded as small, moderate, or large (Fig. 1). Irregularity, attenuation, and/or thickening of the joint capsule are usually indicative of recent or remote injury. Associated findings that may indicate underlying internal derangement(s) include synovial thickening, debris, intra-articular cartilaginous (intermediate signal) or osteochondral bodies (dark ring with/without internal fatty marrow signal), synovial diverticula(e), and ganglion cysts (Fig. 2).
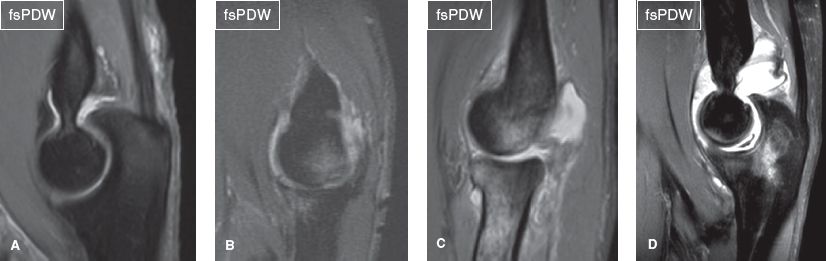
Fig. 1: Normal and abnormal amount of joint fluid. Sagittal images demonstrate normal amount of joint fluid (A), as well as mild (B), moderate (C), and large joint effusion (D) in the elbow.
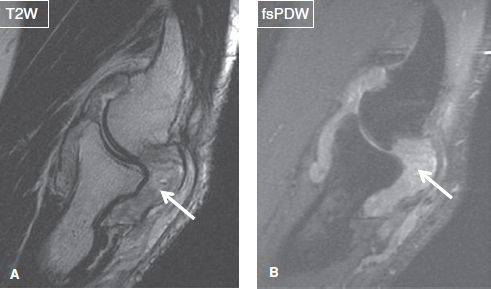
Fig. 2: Rheumatoid arthritis involving the elbow. Sagittal images (A, B) demonstrate large joint effusion with diffuse synovial thickening (arrows).
Loose bodies typically lodge in the olecranon or the coronoid recesses. Potential diagnostic pitfalls include (1) a synovial fringe (meniscus), which is commonly present in the radiocapitellar joint space (Fig. 3); (2) an os supratrochlear dorsale, which is an accessory ossicle adjacent to the olecranon, representing an unfused secondary ossification center; and (3) detached enthesophytes adjacent to the epicondyles, resulting from chronic epicondylitis. Synovial osteochondromatosis is a benign metaplastic proliferative disorder of the synovium, which manifests as numerous osteochondral loose bodies of similar size (primary form) or less number of bodies of variable (secondary form) size. The secondary form is typically seen in older individuals and is associated with prior trauma or arthritis (Fig. 4).
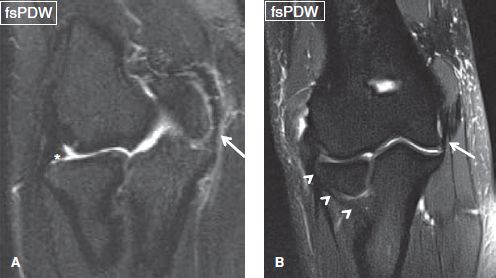
Fig. 3: Normal MR anatomy of the elbow. Coronal images show the posterior band of the ulnar collateral ligament (arrows), the lateral ulnar collateral ligament (arrowheads in B), and a normal synovial fringe (asterisk in A).
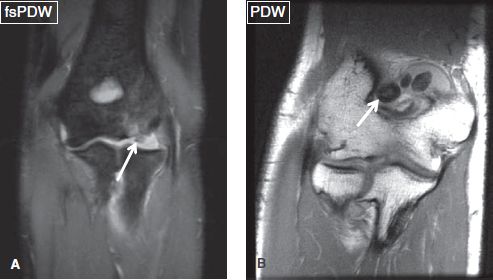
Fig. 4: Loose intra-articular bodies. Coronal images in two different subjects display a loose cartilage body (arrow in A) adjacent to the capitellum with posttraumatic marrow. Notice in a different patient, olecranon recess distended with multiple loose osteochondral bodies of variable size (arrow in B), in this case of secondary osteochondromatosis.
Fatty synovial fronds may be seen with synovial hypertrophy, an entity that is referred to as lipoma arborescens and is defined as partial or complete, depending upon the degree of joint involvement. In most cases, it a response to chronic internal joint derangement, and less commonly a primary process (usually in children), which may require arthroscopic resection.
MEDIAL STRUCTURES:
Ulnar collateral ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Common flexor tendon: [<Normal> <Tendinosis> <Partial tear (low/high grade)> <Complete tear>]
Epicondyle: [<Normal> <Enthesopathy> <Bone marrow edema>]
The UCL is a thickening of the medial capsule, which provides the primary static restraint to valgus stress. It extends from the medial epicondyle to the medial coronoid process, lies immediately under the common flexor tendons and consists of three bundles. The anterior bundle, which is the strongest and most important restraint against valgus instability extends from the inferior aspect of the medial epicondyle to the sublime tubercle of the ulna, and less commonly, up to 3 mm distal to ulnar articular surface. The transverse bundle (Cooper ligament) extends from the medial olecranon to the inferomedial coronoid process and partly forms the floor of the cubital tunnel. The fan-shaped posterior bundle originates from the medial epicondyle, slightly posterior to its most inferior portion and inserts broadly onto the olecranon. It forms the majority of the floor of the cubital tunnel and provides secondary stability when the elbow is flexed beyond 90 degrees. Structurally, the anterior bundle of the UCL is composed of two separate bands, anterior and posterior.
The UCL is primary evaluated in the coronal plane (where it is usually visible on two or three consecutive slices) and secondarily in the axial plane. It appears as a thin band, which extends along the medial surface of the joint, and features homogeneous low signal on all pulse sequences. Small amounts of interspersed hyperintense fat or invaginated synovium may normally exist near the humeral attachment of the anterior bundle, which should not be mistaken for partial tear (Figs. 5, 6). Chronic UCL degeneration appears as ligamentous thickening or attenuation, with or without intrinsic abnormal signal, and is often accompanied by foci of calcification or ossification and enthesopathy. Partial tears (grade I/II sprains) of the UCL can involve the humeral or the ulnar attachment (sublime tubercle). Proximal tears typically involve the deep layer of the humeral attachment (with preservation of the overlying superficial layer) and may be difficult to detect unless joint effusion is present (Figs. 7, 8). Distal tears may be associated with bony fleck avulsion or may feature a T-sign configuration, in which joint fluid extends in a linear fashion along the medial margin of the coronoid process, through the disrupted deep UCL fibers (Fig. 9). MR arthrography is recommended in uncertain cases when conventional images are unrevealing due to scarring. It should be noted that the T-sign can be a normal finding in children, and in some adults. Presence of adjacent fascial edema is a confirmatory finding of partial tear. Complete tears (grade III sprains) of the UCL can involve the midsubstance of the ligament, in which case there is full-thickness ligament discontinuity and irregularity with laxity of torn fragments, or these lesions might be observed as full-thickness avulsion of the ulnar or humeral attachments (Figs. 10–12). The adjacent soft tissues are usually T2 hyperintense, reflecting hemorrhage and edema. Associated injuries include CFT tear, elbow subluxation or dislocation, osteochondral injury, medial epicondyle avulsion, and ulnar nerve (UN) injury.
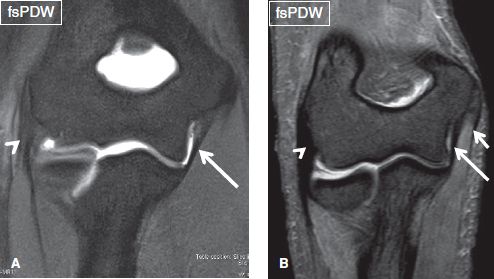
Fig. 5: Normal MR anatomy of the elbow. Consecutive coronal images demonstrate the anterior (arrow in A) and the transverse (long arrow in B) bands of the ulnar collateral ligament, the common extensor tendon (arrowhead in A, B), and the common flexor tendon (short arrow in B).
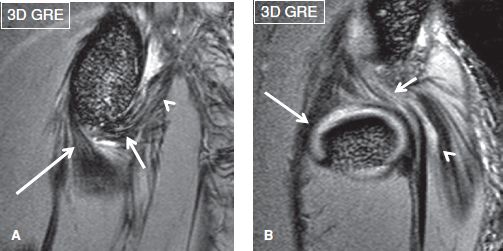
Fig. 6: Normal ulnar collateral ligament. A: Far medial image demonstrates the anterior (long arrow), transverse (short arrow), and posterior (arrowhead) bundles of the ulnar collateral ligament. B: Far lateral image shows the radial collateral ligament (long arrow), the lateral ulnar collateral ligament (short arrow), and the common extensor tendon (arrowhead).
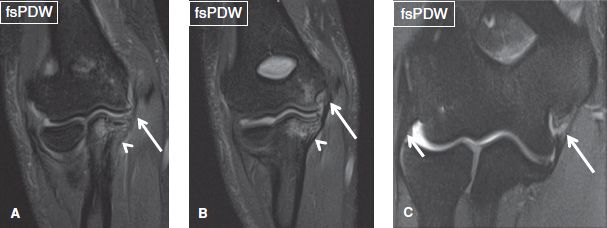
Fig. 7: Sprains of the ulnar collateral ligament. Coronal images. A, B: Sequential images demonstrate mild hyperintensity and thickening of the ulnar collateral ligament (arrows), corresponding to grade I/II sprain. Note the associated marrow edema (arrowheads) of the proximal ulna and distal humerus. C: A partial tear is evident at the posterior band of the ulnar collateral ligament (long arrow), corresponding to grade II sprain. Note the normal RCL (short arrow).
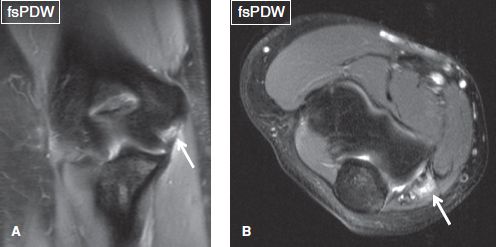
Fig. 8: Grade II sprain of the ulnar collateral ligament. A: Coronal image shows partial discontinuity of the ulnar collateral ligament (arrow), corresponding to grade II sprain. B: In the respective axial image, the lesion involves all the three bundles of ligament (arrow).
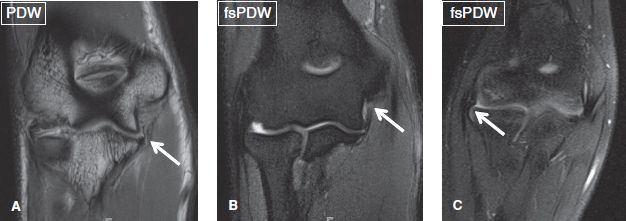
Fig. 9: Partial tear (grade II sprain) of the ulnar collateral ligament. Coronal images. A: Image shows stripping of the distal attachment of the ulnar collateral ligament from the sublime tubercle, creating a “T-sign” (arrow). B: Image demonstrates hyperintensity of the proximal portion of the ulnar collateral ligament (arrow), indicating a partial tear. C: Images exhibit a normal synovial recess, which exists on the lateral aspect of the joint (arrow), and should not be perceived for lateral collateral ligament tear.
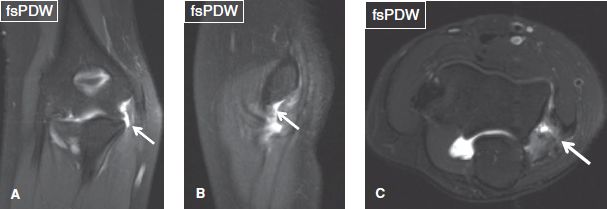
Fig. 10: Grade III sprain of the ulnar collateral ligament. Coronal (A), sagittal (B), and axial (C) images exhibit complete deficiency of all three bundles of the ulnar collateral ligament (arrows).
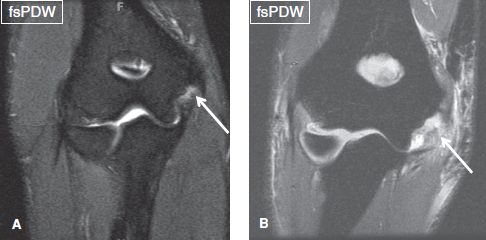
Fig. 11: Grade III sprain of the ulnar collateral ligament. Coronal images. A: Complete discontinuity of the posterior bundle of the ulnar collateral ligament (arrow) is evident at its proximal attachment. B: Complete tear and proximal retraction of all of the three bundles of the ulnar collateral ligament (arrow) at its humeral attachment.
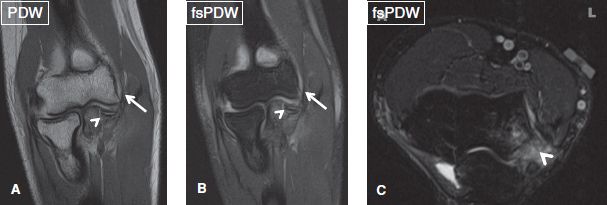
Fig. 12: Grade III sprain of the ulnar collateral ligament. Coronal (A, B) and axial (C) images demonstrate avulsion of the humeral attachment of ulnar collateral ligament (arrows), along with an associated fracture of the coronoid process (arrowheads).
The CFT origin includes the tendons of pronator teres, flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis muscles. The CFT arises from the medial epicondyle and overlies the UCL, providing dynamic support to the latter in resisting valgus stress. The CFT is best evaluated on coronal and axial images and normally demonstrates homogeneous low signal on all sequences (Fig. 5). Repetitive stress or overuse of the flexor and pronator musculature may result in common flexor tendinosis and/or partial tear, which may finally progress to complete tear. The condition is known as medial epicondylitis (golfer’s or pitcher’s elbow). Tendinosis is graded similar to the rotator cuff, as mild (intermediate intrasubstance signal), moderate (thickening and diffuse intermediate increased signal), and severe (diffusely near-fluid-bright intrasubstance signal, difficult to differentiate from tears). The subjacent epicondyle may show bone marrow edema (avulsive), enthesopathy, and/or subcortical avulsive cystic changes, reflecting chronic stress changes. Partial CFT tears manifest as focal increased fluid-like signal or fiber discontinuity on fs proton density–weighted (PDW) or fs T2–weighted (T2W) images, often with underlying tendinosis (Figs. 13, 14). The tears should be graded as low-grade (involving less than 50% of tendon thickness), high-grade (involving 50% to 99% of tendon thickness), or full-thickness (tendon discontinuity and avulsion). In both partial and full-thickness tears, the adjacent soft tissues may be edematous in acute/subacute cases.
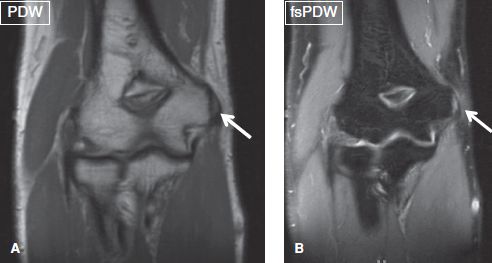
Fig. 13: Grade II sprain of the common flexor tendon. Coronal images show a partial, low-grade tear of the common flexor tendon (arrows).
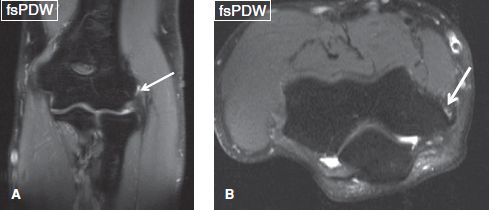
Fig. 14: Grade II sprain of the common flexor tendon. Coronal (A) and axial (B) images show a partial, low-grade tear of the common flexor tendon (arrows).
In adolescents involved in sports with throwing activities, repetitive valgus overload upon the elbow may cause injury to the immature medial epicondyle apophysis. The entity is known as “little leaguer’s elbow,” and it manifests as marrow edema of the apophysis (reflecting stress reaction) in mild cases, frank separation of the apophysis (Salter I injury) in moderate cases, or fragmentation of the apophysis (fracture) in severe cases, in which the degree of displacement is important to report, as apophyseal avulsions larger than 3 or 4 mm necessitate surgical intervention (Figs. 15, 16). Associated findings may include complete tears or avulsions of the UCL, flexor and/or pronator muscle strains, and proximal ulna stress fractures, whereas some cases may be associated with osteochondritis dissecans (OCD) of the capitellum.
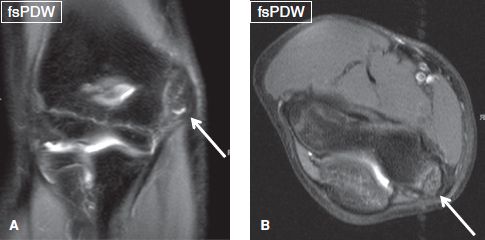
Fig. 15: Little leaguer’s elbow. Coronal (A) and axial (B) images demonstrate osseous fragmentation of the medial epicondyle (arrows) in the case of a 12-year-old baseball player.
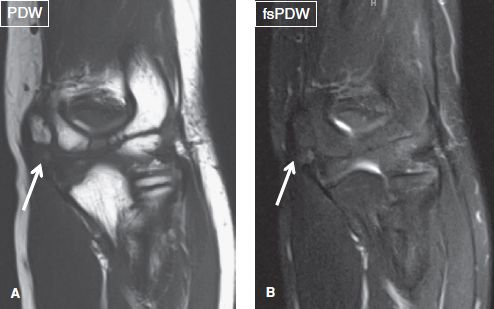
Fig. 16: Chronic avulsion of the medial epicondyle. Coronal images (A, B) exhibit partially united mildly edematous avulsed fragment of the medial epicondyle (arrows).
LATERAL STRUCTURES:
Radial collateral ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Lateral ulnar collateral ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Annular ligament: [<Intact> < Thickened> <Acute sprain>]
Common extensor tendon: [<Normal> <Tendinosis> <Partial tear (low/high grade)> <Complete tear>]
Lateral epicondyle: [<Normal> <Enthesopathy> <Bone marrow edema>]
The lateral collateral ligamentous structures include the RCL, which is the main restraint to varus stress, and the LUCL that provides posterolateral static stability. The RCL extends from the anterior aspect of the lateral epicondyle to the annular ligament and fascia of the supinator muscle. The LUCL originates from the lateral epicondyle, blends with RCL fibers at its origin, courses posterior to the radius, and inserts on the supinator crest of the ulna. It is absent in up to 10% of anatomic specimens. The RCL is relatively straight and lies anterior to the LUCL, which is obliquely oriented. The RCL and LUCL are best visualized on sequential coronal images from anterior to posterior, respectively. The annular ligament attaches to the anterior and posterior margins of the ulnar sigmoid notch, encircling the radial head like a sling. It serves as the primary stabilizer of the proximal radioulnar joint and is optimally visualized on axial images (Figs. 17, 18). The inconstantly present accessory annular ligament extends from the annular ligament to the supinator crest of the ulna.
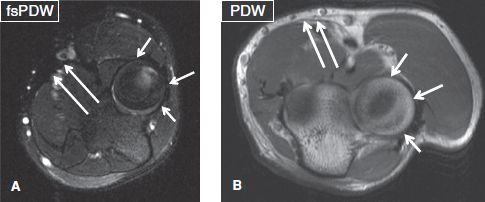
Fig. 17: Normal annular ligament and bicipital aponeurosis (lacertus fibrosus). Axial images (A, B) show the annular ligament (short arrows) and the bicipital aponeurosis (long arrows).
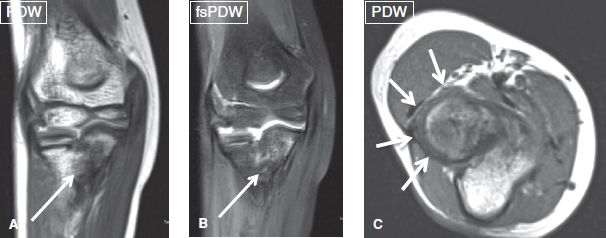
Fig. 18: Thick annular ligament in the setting of congenital proximal radioulnar synostosis. Coronal (A, B) images demonstrate proximal radioulnar synostosis (arrows) in this young individual (note the unfused epiphyses). C: The corresponding axial image shows diffuse thickening of the annular ligament (arrows), as a result of the developmental and remodeling abnormality.
The lateral collateral ligaments normally exhibit uniform thickness and homogeneous low-signal intensity on all sequences (Figs. 7, 19). They can be injured by acute varus stress injury or elbow dislocation, which may result in posterolateral rotary instability, especially with injury to the LUCL. Posterolateral instability is tested by pivot-shift test clinically using axial and valgus load in supination position. Ligament sprains are graded similar to other ligaments of the body, with grade III sprains indicating complete disruption, which most often involve the humeral attachments (Figs. 20–23). Avulsions from bony attachments may be associated with marrow edema and/or underlying enthesopathy. RCL injury is commonly associated with common extensor tendon (CET) tear in lateral epicondylitis (described in the next paragraph). Disruption of the LUCL results in pivot-shift phenomenon and posterolateral rotary instability of the joint, which is best seen on coronal images as asymmetric posterolateral joint space widening. Disruption of the annular ligament results in subluxation of the radial head, which is best depicted on sagittal images with a secondary sign of radiocapitellar line disruption. Table 1 presents the classification system for staging elbow instability.

Fig. 19: Normal MR anatomy of the elbow. Sagittal images exhibit the lateral ulnar collateral ligament (arrow in A), the biceps tendon (long arrow in B), a redundant triceps tendon (short arrows in B, C), and the bare area of the trochlear notch (arrowhead in B).
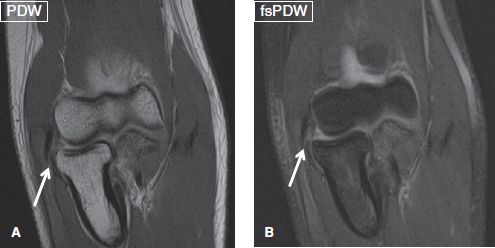
Fig. 20: Grade III sprain of the radial collateral ligament. Coronal images (A, B) show complete discontinuity of the radial collateral ligament (arrows).

Fig. 21: Grade III sprain of the radial collateral ligament. Coronal image displays complete discontinuity of the radial collateral ligament (arrow).
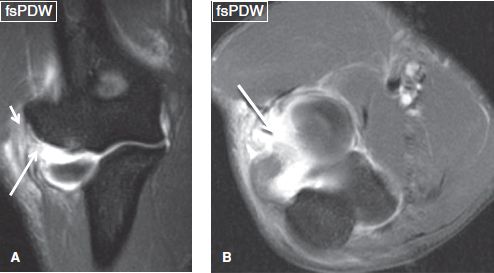
Fig. 22: Grade III sprain of the lateral ulnar collateral ligament. Coronal (A) and axial (B) images demonstrate complete discontinuity of the lateral ulnar collateral ligament (arrows). Also note the high-grade partial tear of the common extensor tendon origin (short arrow), fascial edema, and posterolateral joint space widening that would be seen in the setting of posterolateral instability.

Fig. 23: Sprains of the collateral ligaments in the setting of elbow fracture-dislocation. Coronal (A–C) and sagittal (D–F) images show tears of the RCL (arrow in B), UCL (long arrow in C) and LUCL (short arrows in C, D), fracture of the radial head (long arrow in D), and large joint effusion (arrow in E) with a loose body (arrow in F).
The CET origin includes the extensor carpi radialis brevis and longus, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris muscles. The CET originates from the anterior aspect of the lateral epicondyle and supracondylar ridge and normally exhibits uniform thickness and homogeneous low signal on all sequences. The tendon may undergo degeneration (tendinosis), or partial or complete tears, particularly in individuals engaged in occupations or sports that involve repetitive varus stress to the lateral aspect of the elbow (Figs. 24–28). The entity is known as lateral epicondylitis or “tennis elbow,” and is much more common compared to its medial counterpart. Tendinosis and tears are graded similar to CFT as described above. Additional findings, which may be present in tennis elbow include marrow edema of the lateral epicondyle, enthesopathy, avulsive cystic changes, and RCL injury.
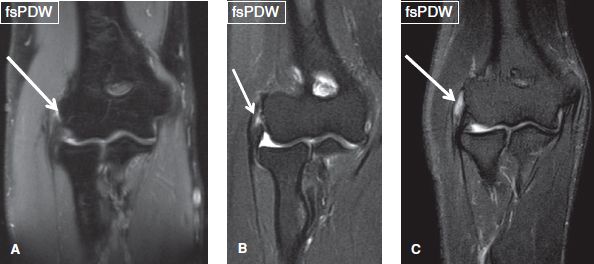
Fig. 24: Grade II sprain of the common extensor tendon. Coronal images (A, B, C) display three different cases of partial tears of the common extensor tendon (arrows), low-, intermediate-, and high-grade tears, respectively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







