Advances in medical and surgical care over the past 20 years have resulted in children who formerly would have died at birth or infancy now surviving well into adulthood, many with permanent physical disabilities, including those caused by cerebral palsy. Inadequate medical and surgical diagnoses and intervention are prevalent in the adult cerebral palsy population. Decreased physical activity and participation in physical therapy and fitness programs, along with loss of strength, contractures, and pain are common factors in the loss of functional weight bearing, self-care, and daily performance over time. Increased awareness of these problems is needed by adult health care providers who provide care to these individuals and also by pediatric providers who may be able to intervene and prevent some of the long-term problems. Early identification and intervention in the child and younger adult remain the ideal in the pursuit of optimal musculoskeletal function and lifestyle throughout the adult years.
Advances in medical and surgical care over the past 20 years have resulted in children who formerly would have died at birth or infancy now surviving well into adulthood, many with permanent physical disabilities, including those caused by cerebral palsy (CP). Increased awareness of these problems is needed by adult health care providers of these individuals and also by pediatric providers who may be able to intervene and prevent some of the long-term problems. Orthopedic issues prevalent in the child with CP have long-term lifetime sequela being further defined at this time. Before any specific musculoskeletal intervention, the primary, secondary, and associated conditions of CP need to be considered in addition to comorbidities. The primary condition of CP, by definition, is nonprogressive over time in the neurologic sense. Secondary conditions are those that develop as a result of the primary conditions and include causes such as soft tissue contractures, degenerative arthritis, hip dysplasia, and equinovalgus foot deformities. These conditions can often be prevented with early diagnosis and appropriate intervention before problematic sequelae develop. Associated conditions are those that occur with increased prevalence in individuals with CP, such as visual or auditory impairment, seizure disorder, learning disability, and gastroesophageal reflux. These conditions are not necessarily preventable, but their impact may be lessened by early diagnosis and intervention during the developmental years. Comorbidities are those conditions unrelated to the primary disability and appearing with similar frequency whether one has CP or not (eg, diabetes, appendicitis, hypertension). In the author’s experience medical care providers often blame the primary condition for just about all the symptoms and problems that can develop in the adult with CP. Symptoms such as leg pain, discomfort in the neck or lower back, and headaches are too often misattributed to the underlying condition of CP, giving no further pursuit to more specific and definitive diagnosis. For example, a person with CP presenting with a headache may be erroneously told that all people with CP develop headaches eventually, with no additional diagnostics being pursued. Strauss and colleagues reviewed the public health record for the state of California and reported up to 9 times higher risk of brain cancer in people with CP, both young and old. As with any evaluation of an individual presenting with medical or surgical symptoms, the main initial goal should be to establish a correct diagnosis. This goal is less frequently achieved if medical symptoms and loss of function in individuals with CP are attributed to the primary condition.
Adults with CP are living longer, with an estimated population in the United States of between 400,000 and 500,000, depending on the defined age of an adult. In addition to a possible higher risk of brain cancer in people with CP, Strauss and colleagues also reported a 3 times higher risk of breast cancer and up to 4 times increased risk of cardiovascular death. A busy clinician might easily blame persistent back pain in an adult with CP on the primary condition without detecting breast cancer and a spinal metastasis in this higher-risk population. Most of the higher risk is believed to be secondary to inadequate medical screening in the adult with CP. Inadequate screening in part relates to a lack of education of the medical provider, undersized and inaccessible medical examination rooms and equipment, and not enough time being allotted to the provider for adequate history taking and physical evaluation. This is especially so for those of increased physical involvement and with more challenging communication needs. Communication barriers are especially significant for those adults who are nonverbal, require augmentative communication devices, or have expressions of pain that are not recognized by the busy clinician. Adults with CP surviving well past 60 years of age and maintaining a functional lifestyle with or without caregiver assistance are not uncommon. Higher survival rates have been found in those adults with increased functional levels, both ambulatory and mat mobility, and in individuals with gastrostomy tube feedings. Rimmer was one of the first investigators to report that regular exercise improves functional status, decreases the level of required assistance, and reduces the incidence of secondary conditions in people with disability. Obesity is a secondary condition of concern in the adult with decreased metabolic rate and lack of exercise. Heller and colleagues subsequently reported that participation in and frequency of exercise depend mostly on the care provider’s attitude; if the care provider believed that exercise was important to the individual with physical disability, then exercise occurred.
A major functional premise in the care for the adult with CP is that functional deterioration is almost always secondary to something other than the primary condition. Multiple diagnoses always need to be considered. Adults with CP, not uncommonly, develop multiple sclerosis, Alzheimer disease, Parkinson disease, depression, cerebral vascular accident, and other associated or comorbid conditions.
The natural history of CP and musculoskeletal function is of utmost importance and needs further definition and lifetime perspective. Primitive reflexes, as well as a gradual trend toward more dystonia, may be more noticeable with aging in this population. About 50% to 80% of individuals with cerebral palsy are able to walk in some manner during their lifetime. The gross motor functional measure (GMFM) may be the most reliable method for predicting ultimate walking ability and gross motor function classification system (GMFCS) level. The GMFM and GMFCS levels have been discussed previously in this text and therefore not repeated here for the sake of brevity. The loss of ambulatory skills in the adult with CP seems to occur at 2 peaks of age. The first peak is around the age of 20 to 25 years, commonly associated with progressive crouch gait and inability of the young adult to keep up with peers efficiently in the community, workplace, and academic settings. The second peak is around the age of 40 to 45 years, with progressive fatigue, pain, and possibly accelerated joint degeneration, making further functional ambulation not possible. To date there are no studies of accelerated arthritis or joint degeneration in adults with CP, although anecdotal evidence is supportive. Individuals with minimal to no ambulatory limitations (GMFCS level I) or those requiring just an ankle-foot orthosis (AFO) or simple gait aid for longer distances (GMFCS level II) are at less risk for gait deterioration and not uncommonly are ambulatory in the seventh decade of life. Individuals who require more extensive gait aids for exercise or in-home walking and those just able to stand or take a few steps with transfers (GMFCS levels III and IV, respectively) are at greatest risk for loss of ambulatory function or weight-bearing skills over the lifetime.
Too often, specialists who deal with children having CP focus inordinately on ambulatory function at the neglect of other more lifetime functional skills. Such skills include those dealing with social engagement, academics, and home and workplace participation. More emphasis should be placed on the concept of functional weight bearing over the lifetime, of which functional ambulation is just one component. In this manner, functional weight bearing becomes particularly more concerning for adults with CP having more physical involvement (GMFCS levels III and IV), whereby a loss of weight-bearing posture in any form can take away functional in-home or community participation. These individuals often crawl throughout their home or alternative living environment. Not uncommonly they ambulate 3 or 4 steps at a time into and out of a bathroom or pull to stand from a wheelchair allowing overhead reach into cupboards or preparation of meals on countertops. Taking a step or two often eliminates the need for a Hoyer lift, ceiling track, or similar hydraulic device while also sparing the care provider’s spinal column from chronic stress, strain, and debility. These are all vital functions, not to exclude others, precluded without effective weight-bearing postures of the extremities. Any intervention by the treating orthopedist to preserve functional weight bearing over the lifetime is precious in keeping the adult as independent as possible in the community, home, and other chosen environments. Functional extension through the hips and knees and positioning of the feet are important for functional weight bearing over the lifetime and, when threatened, should be addressed aggressively at any age. The natural history of ambulation in CP (untreated outcomes) over the lifetime seems to be on a downward spiral, beginning around the time of early adolescence. It is therefore important for parents, therapists, surgeons, and young adults with CP to realize that ambulation may already be on a slow downward trajectory when multilevel surgery (hips, knees, and ankles) is being considered. Surgical intervention to maintain gait at the present level of function might well be an improvement over the natural history. In this regard, further improvements in gait parameters compared with presurgical baseline could represent an even greater gain of function. Comprehensive computerized functional gait laboratory assessment is still the best way to define, measure, and record gait function over time, pre- and postsurgically, and is the norm for all functional gait surgery in both young and older people with CP. With this in mind, a brief discussion regarding spasticity management along with specific review of certain conditions identified as more common in the adult with CP is in order.
Spasticity
Botulinum toxin A (BTX-A) continues to have a positive role in adults for relaxing hypertonic muscles for functional gain in the absence of fixed contractures. The toxin can be particularly helpful for individuals with dystonia in relieving painful spasms, improving vertical posture, and controlling unwanted upper extremity motions or tremors that interfere with functional tasks. BTX-A inhibits the release of acetylcholine from the nerve terminal, causing partial paralysis of the muscle lasting up to 3 to 4 months at a time. Repeat BTX-A injections may not be needed every 3 months if appropriate stretching and splinting with home exercise is in place after the procedure. In individuals with dystonia, the botulinum toxin injections often need to be repeated every 3 months for inhibition of the recurrent movement patterns.
Adults may benefit from intrathecal baclofen, more commonly but not exclusively, those of nonambulatory status. It is not uncommon to see catheter tip placements as high as the midcervical spine in individuals with more dystonia or upper extremity involvement. Baclofen acts at the level of the spinal cord; it binds to GABA B receptor sites, agonizes the site, and suppresses the release of excitatory neurotransmitters. Augmenting GABA B activity reduces spasticity. Medical management can include levodopa and/or trihexyphenidyl (a centrally acting anticholinergic) in those individuals with dystonia. Diazepam, oral baclofen, and α 2 -adrenergic agonists such as tizanidine or clonidine can be helpful at the brain and spinal level (clonidine is often used in those with spinal cord injury). Dantrolene sodium works at the level of the muscle, inhibiting the release of calcium ions from the sarcoplasmic reticulum. It acts on nonspastic muscles as well and may cause some unwanted weakness in the ambulatory patient. The medication carries a “black box” warning for hepatotoxicity, which is seen in about 1.8% of patients treated. Monitoring the levels of liver enzymes is recommended (as for tizanidine) at least every 6 months, and the medication is weaned if drug-related abnormalities are identified. Phenol (a 5% or 7% solution) injected into motor nerves can still be helpful, particularly around the hip, to decrease unwanted adduction posture in the absence of contracture. With good positioning and exercise postprocedure, the partial phenol obturator neurectomy should not result in unwanted abduction and external rotation hip contracture. Phenol can also be useful at the level of the shoulder. Injections into the pectoralis major, latissimus dorsi, and biceps (musculocutaneous neurectomy) can improve upper extremity function and overhead reach, facilitating upper torso dressing and outer garment donning and doffing.
Spine
Scoliosis can be present in up to 60% of adults with CP and is particularly likely in those with nonambulatory status having spastic quadriparesis. Progression with aging can occur to approximately 1° per year and should be monitored carefully over time. Decompensation can be accompanied by loss of function, improved somewhat with custom molded seating or postural thoracolumbar orthosis, depending on the individual. Pain, when it occurs, is often associated with thoracolumbar soft tissue strain on the convex side and degenerative changes in the facet joints on the concave side. Scoliotic pain can be a new experience for the adult, as scoliosis in children is generally pain free. Episodic bolus physical therapy and nonsteroidal antiinflammatory drugs can be helpful. Despite conservative care, decompensating curvatures beyond 50° often require posterior fusion to prevent future compromise to the cardiopulmonary and gastrointestinal systems.
Spondylolysis has a prevalence of approximately 4.4% at 6 years of age, increasing to 6% in able-bodied adults. Reports in the literature have identified spondylolysis in weight-bearing adults with CP, having an estimated prevalence of between 21% and 30%, with or without dystonia. The prevalence may be higher in individuals who had a selective posterior rhizotomy and associated increased anterior pelvic tilt. In a series of 143 patients who had never walked, in whom the condition of CP was predominant, no case of spondylolysis or spondylolisthesis was detected radiographically. Dystonic movements in the lumbosacral spine, particularly into extension and axial rotation, seem to be contributing to the higher incidence of spondylolysis in patients with CP. It is not uncommon to see adults with CP having chronic back pain, followed by their primary care providers for years. The back pain has usually been attributed to their primary condition of CP; it is believed to be expected and usual and elicits no further diagnostic evaluation. Simple radiographs of the lumbar spine, including an oblique view, often reveal spondylolysis with low-grade spondylolisthesis, commonly improving with basic conservative care. Efforts to minimize significant anterior pelvic tilt in weight-bearing children may be helpful in preventing these potential stress fractures later in life. These efforts would seem particularly important in those undergoing selective posterior rhizotomy or aggressive hamstring lengthening, especially in the presence of tight hip flexors. Surgical options including segmental fusion in the presence of failed conservative intervention and any neurologic compromise should be used when necessary. Toe walking should be minimized with the use of appropriate orthosis when indicated. Medical history should also include a review of any falls or injuries to the lumbar and pelvic region because more distant traumatic causes may not be considered relevant by the individual at the time of medical evaluation.
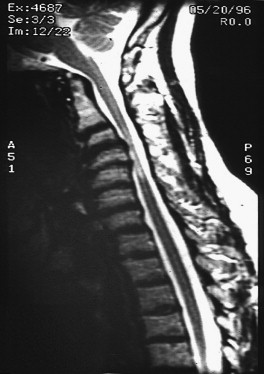
Cervical stenosis has been found to occur with a higher incidence in adults with CP and dystonia than in normal controls. In a study of 180 patients with CP and dystonia compared with 417 control subjects, Harada and colleagues found an 8-fold increase of the frequency of cervical disk degeneration and a 6- to 8-times increased frequency of listhetic instability in the midcervical spine in the CP group. The combination of disk degeneration and listhetic instability with a narrowed spinal canal was believed to be predisposing individuals to rapid progressive loss of function and devastating neurologic deficit. In approximately 35% of adults with CP, Ando and Ueda identified functional deterioration with higher frequency in those having involuntary movements of the head and neck. Symptoms often occur over a 6- to 18-month period and include neck pain, loss of ambulation, and progressive hypertonicity, as well as loss of bladder control and upper extremity function. Additional studies focused on adults with CP have associated the higher incidence of cervical spondylosis and myelopathy with dystonic neck and head postures. Fig. 1 is a magnetic resonance imaging (MRI) scan of a 38-year-old man with CP, spastic quadriparesis, and cervical dystonia. Encroachment of the spinal canal can be noted particularly at the C4-C5 level. This individual was independent with his self-care, toileting, and mobility including limited community ambulatory ability with a gait aid (GMFCS level III), 1 year before the discovery of his cervical stenosis. Over a 6- to 12-month period, he gradually lost his ambulatory skills, displayed increased hypertonicity in the trunk and lower extremities, and progressed toward inability to assist with his dressing and upper extremity hygienes. Bladder control was lost with spontaneous incontinence about 10 months after onset of symptoms. Anterior surgical decompression with posterior fusion was provided, and the patient regained his former ability to walk and participate in self-care activities within 8 months. Thirteen years after surgery, he continues to maintain independent living skills and ambulation at GMFCS level III and requires just minimal supervision within his community group home residence.
In individuals with higher risk beginning in young adulthood, serial MRI scans every 2 years may facilitate early identification of cervical spondylosis and stenosis, allowing for more proactive intervention and prevention of sequelae. Botulinum toxin injections can be helpful in minimizing cervical dystonia, particularly excessive movements into extension and axial rotation. Medications for control of dystonia, including intrathecal baclofen therapy, should be considered in carefully selected individuals. Calmer environments, use of sensory biofeedback techniques, and stress-reduction strategies can be helpful in reducing some regional dystonia. The author recalls a patient who, when flying alone in her glider plane, was completely relieved of all her dystonic movements until touchdown, when the ground support staff would come to her assistance. Cervical discomfort of any sort should be taken seriously in this population, as it may be the only prodrome recognizable before more devastating neurologic compromise. Serial neurologic examinations adapted for individuals with CP are encouraged. Reproducible voluntary motor functions measured over time along with a clinically reproducible spasticity measure are suggested. Close monitoring of bowel and bladder functions is not to be neglected. If conservative care fails, surgical decompression of the stenotic cervical canal may be required. A trend toward more anterior approach with interbody fusion and posterior wiring has been noted in the literature. Regional dystonia postoperatively in the surgical zone, with potential for aspiration and bleeding, is a higher risk of such surgical procedures. Cervical immobilization devices are of limited use in this population. Cervical stenosis with major functional loss over time seems to be rapidly progressive in this population of patients with dystonic CP. For this reason, surgical intervention, despite the higher risk, seems warranted when conservative care has failed to maintain function and comfort.
Spine
Scoliosis can be present in up to 60% of adults with CP and is particularly likely in those with nonambulatory status having spastic quadriparesis. Progression with aging can occur to approximately 1° per year and should be monitored carefully over time. Decompensation can be accompanied by loss of function, improved somewhat with custom molded seating or postural thoracolumbar orthosis, depending on the individual. Pain, when it occurs, is often associated with thoracolumbar soft tissue strain on the convex side and degenerative changes in the facet joints on the concave side. Scoliotic pain can be a new experience for the adult, as scoliosis in children is generally pain free. Episodic bolus physical therapy and nonsteroidal antiinflammatory drugs can be helpful. Despite conservative care, decompensating curvatures beyond 50° often require posterior fusion to prevent future compromise to the cardiopulmonary and gastrointestinal systems.
Spondylolysis has a prevalence of approximately 4.4% at 6 years of age, increasing to 6% in able-bodied adults. Reports in the literature have identified spondylolysis in weight-bearing adults with CP, having an estimated prevalence of between 21% and 30%, with or without dystonia. The prevalence may be higher in individuals who had a selective posterior rhizotomy and associated increased anterior pelvic tilt. In a series of 143 patients who had never walked, in whom the condition of CP was predominant, no case of spondylolysis or spondylolisthesis was detected radiographically. Dystonic movements in the lumbosacral spine, particularly into extension and axial rotation, seem to be contributing to the higher incidence of spondylolysis in patients with CP. It is not uncommon to see adults with CP having chronic back pain, followed by their primary care providers for years. The back pain has usually been attributed to their primary condition of CP; it is believed to be expected and usual and elicits no further diagnostic evaluation. Simple radiographs of the lumbar spine, including an oblique view, often reveal spondylolysis with low-grade spondylolisthesis, commonly improving with basic conservative care. Efforts to minimize significant anterior pelvic tilt in weight-bearing children may be helpful in preventing these potential stress fractures later in life. These efforts would seem particularly important in those undergoing selective posterior rhizotomy or aggressive hamstring lengthening, especially in the presence of tight hip flexors. Surgical options including segmental fusion in the presence of failed conservative intervention and any neurologic compromise should be used when necessary. Toe walking should be minimized with the use of appropriate orthosis when indicated. Medical history should also include a review of any falls or injuries to the lumbar and pelvic region because more distant traumatic causes may not be considered relevant by the individual at the time of medical evaluation.
Cervical stenosis has been found to occur with a higher incidence in adults with CP and dystonia than in normal controls. In a study of 180 patients with CP and dystonia compared with 417 control subjects, Harada and colleagues found an 8-fold increase of the frequency of cervical disk degeneration and a 6- to 8-times increased frequency of listhetic instability in the midcervical spine in the CP group. The combination of disk degeneration and listhetic instability with a narrowed spinal canal was believed to be predisposing individuals to rapid progressive loss of function and devastating neurologic deficit. In approximately 35% of adults with CP, Ando and Ueda identified functional deterioration with higher frequency in those having involuntary movements of the head and neck. Symptoms often occur over a 6- to 18-month period and include neck pain, loss of ambulation, and progressive hypertonicity, as well as loss of bladder control and upper extremity function. Additional studies focused on adults with CP have associated the higher incidence of cervical spondylosis and myelopathy with dystonic neck and head postures. Fig. 1 is a magnetic resonance imaging (MRI) scan of a 38-year-old man with CP, spastic quadriparesis, and cervical dystonia. Encroachment of the spinal canal can be noted particularly at the C4-C5 level. This individual was independent with his self-care, toileting, and mobility including limited community ambulatory ability with a gait aid (GMFCS level III), 1 year before the discovery of his cervical stenosis. Over a 6- to 12-month period, he gradually lost his ambulatory skills, displayed increased hypertonicity in the trunk and lower extremities, and progressed toward inability to assist with his dressing and upper extremity hygienes. Bladder control was lost with spontaneous incontinence about 10 months after onset of symptoms. Anterior surgical decompression with posterior fusion was provided, and the patient regained his former ability to walk and participate in self-care activities within 8 months. Thirteen years after surgery, he continues to maintain independent living skills and ambulation at GMFCS level III and requires just minimal supervision within his community group home residence.
In individuals with higher risk beginning in young adulthood, serial MRI scans every 2 years may facilitate early identification of cervical spondylosis and stenosis, allowing for more proactive intervention and prevention of sequelae. Botulinum toxin injections can be helpful in minimizing cervical dystonia, particularly excessive movements into extension and axial rotation. Medications for control of dystonia, including intrathecal baclofen therapy, should be considered in carefully selected individuals. Calmer environments, use of sensory biofeedback techniques, and stress-reduction strategies can be helpful in reducing some regional dystonia. The author recalls a patient who, when flying alone in her glider plane, was completely relieved of all her dystonic movements until touchdown, when the ground support staff would come to her assistance. Cervical discomfort of any sort should be taken seriously in this population, as it may be the only prodrome recognizable before more devastating neurologic compromise. Serial neurologic examinations adapted for individuals with CP are encouraged. Reproducible voluntary motor functions measured over time along with a clinically reproducible spasticity measure are suggested. Close monitoring of bowel and bladder functions is not to be neglected. If conservative care fails, surgical decompression of the stenotic cervical canal may be required. A trend toward more anterior approach with interbody fusion and posterior wiring has been noted in the literature. Regional dystonia postoperatively in the surgical zone, with potential for aspiration and bleeding, is a higher risk of such surgical procedures. Cervical immobilization devices are of limited use in this population. Cervical stenosis with major functional loss over time seems to be rapidly progressive in this population of patients with dystonic CP. For this reason, surgical intervention, despite the higher risk, seems warranted when conservative care has failed to maintain function and comfort.
Surgical procedures and indications
Hip
Hip displacement occurs in approximately 1% of patients with spastic hemiplegia, up to 15% of those with diplegia, and more than 50% of those with quadriplegia. It has been shown that children who function at GMFCS level I have almost no chance of hip subluxation and those who function at GMFCS levels IV and V have up to a 70% to 90% chance of hip dysplasia. As the GMFCS level increases, the degree of hip abnormality increases and the ability to walk decreases. Pain with degenerative arthritis and joint space incongruity can occur in at least 50% of individuals with CP who have dislocated hips or pseudoacetabulum formation over time. This problem is of particular concern in individuals having functional weight bearing in the lower extremities. Weight bearing can be limited but is important in standing pivot transfers, standing table usage, household or community ambulation, or crawling. Mild hip displacement, which is asymptomatic in the teenager, may develop into painful premature degenerative arthritis, leading to a loss of functional weight bearing and the need for additional reconstructive surgery later in life. Early identification of hip dysplasia and appropriate intervention in the younger child should hopefully prevent most of this hip abnormality in subsequent years. Intra-articular injections with long-acting steroid and anesthetic can provide relief in the dysplastic, dislocated, or osteoarthritic hip for up to 6 months or longer in certain individuals. These injections combined with periarticular BTX-A injections and phenol obturator neurectomies in individuals having more dynamic adduction preference can alter joint articulating surfaces, reduce spasms, and provide further relief. Intrathecal baclofen, oral medications to reduce tone, and therapy interventions including seating adjustments are still valuable and always need to be considered in the adult with a painful hip.
Total hip arthroplasties have been reported as safe and effective in selected individuals with CP having severe degenerative arthritis and pseudoacetabular formation. Long-term follow-up studies have shown more than 90% pain relief and improved function with time, even when operated on at a young age of 30 years. Wear and tear to the arthroplastic joint seems to be minimal, which may relate to fewer steps per day and over time in the adult with CP. Fig. 2 shows severe degenerative arthritis with pseudoacetabular formation in a 42-year-old man with spastic diplegia. Ambulatory function had markedly decreased 5 years before surgery, from more than a mile (GMFCS level II) to less than 10 steps (GMFCS level IV). Severe loss of hip motion was present, which limited hip abduction to less than 15° with near arthrodesis bilateral. Fig. 3 shows the same individual 1 year after bilateral total hip arthroplasties.











