Tendon Transfer for Foot Drop
Mark E. Easley
Aaron T. Scott
DEFINITION
Pathology leading to a spectrum of motor function loss that includes loss of ankle dorsiflexion
Common peroneal nerve palsy, L5 radiculopathy, cerebrovascular accident
Loss of ankle dorsiflexion and hindfoot eversion
Retained posterior tibial tendon (PTT) function
Hereditary sensory motor neuropathy
A constellation of motor function deficits and associated deformity
Includes loss of dorsiflexion and hindfoot eversion
Retained PTT function
Flaccid paralysis
Global loss of motor function to the ankle and foot
ANATOMY
Posterior tibialis
Muscle originates on the posterior tibia, interosseous membrane (IOM), and fibula.
Muscle and then tendon course in the deep posterior compartment.
Tendon travels directly posterior to the medial malleolus.
Tendon has numerous insertions on bones of plantar midfoot, spring ligament, and medial aspect of navicular.
IOM and distal tibia-fibula syndesmosis
Thick fibrous bands between tibia and fibula
Distal tibia-fibula syndesmosis is narrow, with little space for tendon transfer even when a generous window is created in the distal IOM.
Inferior extensor retinaculum
On the dorsum of the foot to prevent bowstringing of the extensor tendons as they transition across the anterior ankle to the dorsal foot
Sciatic nerve
Comprises tibial and common peroneal nerves that separate immediately proximal to the popliteal fossa
Common peroneal nerve often affected in these neuropathies
Superficial peroneal nerve
Motor function to anterior and lateral compartment muscles
Dorsiflexion and eversion, respectively
Sensory distribution to dorsum of the foot
Deep peroneal nerve
Courses between tibialis anterior and extensor hallucis longus tendons proximal to the ankle
Located directly on the dorsum of midfoot
Immediately deep to extensor hallucis brevis muscle belly
Motor function to intrinsic muscles of foot
Sensory distribution to first web space
Tibial nerve function typically spared
Tibial nerve must be intact to create a dynamic tendon transfer.
If tibial nerve is not intact, then transfer can only be a tenodesis.
Anterior ankle and dorsal midfoot neurovascular structures at risk
Superficial peroneal nerve (may be insensate as part of the neuropathy)
Deep neurovascular bundle
Anterior tibial artery
Deep peroneal nerve (may also be insensate as part of the neuropathy)
Peroneal artery branch
Situated directly on anterior distal IOM
PATHOGENESIS
Loss of common peroneal nerve function
Loss of ankle dorsiflexion and hindfoot eversion
Loss of major antagonists
Eventual equinus contracture
Imbalance of hindfoot inverter (PTT) and everters (peroneus brevis and usually, but not always, peroneus longus)
Eventual hindfoot varus deformity
Imbalance of hindfoot inverters (PTT) and everter (peroneus longus)
Flaccid paralysis
Tibial and common peroneal nerve palsies
No motor function distal to knee
Because both sets of major antagonists lost, typically no contractures
NATURAL HISTORY
Foot drop may eventually recover.
Tendon transfers should not be considered until a chance for recovery has been ruled out.
Common peroneal nerve palsy may lead to progressively worsening equinocavovarus foot deformity due to overpull of plantarflexors and inverters powered by intact tibial nerve and loss of dorsiflexors and everters powered by compromised common peroneal nerve.
Flaccid paralysis remains relatively stable because both sets of antagonists are compromised.
PATIENT HISTORY AND PHYSICAL FINDINGS
Gait abnormality
“Slap foot gait”
Inability to dorsiflex ankle and control tibialis anterior from heel strike to stance phase
Exaggerated hip and knee flexion
Inability to dorsiflex ankle or great toe from push-off through swing phase
Compensation to allow toes to clear during swing phase
Hindfoot inversion
Patient walks on lateral border of foot.
Inability to dorsiflex ankle
May check by asking patient to walk on heels
Manual muscle testing with patient seated on examining table with knee flexed
Lack of eversion
Varus hindfoot
Over time, may become a fixed inversion contracture
In some disease processes (eg, Charcot-Marie-Tooth disease), toe dorsiflexion is spared, creating claw toe deformities.
Patient attempts to compensate for lack of ankle dorsiflexion with toe extensors, worsening claw toe deformities.
Even when toe extensors are involved in the palsy, flexor tendons may become contracted.
Passive dorsiflexion of the ankle will reveal this.
With equinocavovarus foot contracture, calluses may form under metatarsal heads, particularly the fifth.
Sensation may be diminished on the dorsal and lateral aspects of the foot.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Imaging is typically unnecessary for patients with foot drop except in the following situations:
Consideration should be given to MRI:
If there is concern for mass effect creating a compressive neuropathy: lumbar spine, common peroneal nerve at fibular head
To rule out tibialis anterior tendon rupture (should be evident on clinical examination alone)
Consideration should be given to radiographs of foot or ankle:
To rule out stress fracture
To better define bony deformity (fixed deformity, associated ankle or foot arthritis; important because arthrodesis may need to be considered in lieu of or in combination with tendon transfer)
Electrodiagnostic studies
Absence of recovery at 1 year and particularly at 18 months is highly suggestive that recovery of nerve function will not occur.
Nerve conduction studies and electromyography
Baseline and follow-up studies to determine if any recovery is evident
Important to determine if tendon transfer is warranted
Tendon transfer should not be performed if nerve function may recover
Absence of recovery at 1 year and particularly at 18 months is highly suggestive of no recovery.
We recommend consultation with a neurologist to confirm interpretation of electrodiagnostic studies.
Studies may also define function of PTT.
Important when considering dynamic PTT transfer versus PTT tenodesis
A tendon transfer of a healthy tendon immediately reduces its strength on manual muscle testing from 5/5 to 4/5, so if it is already compromised, then the tendon transfer will do little more than create a tenodesis.
Useful in determining if a more proximal compressive neuropathy exists
DIFFERENTIAL DIAGNOSIS
Tibialis anterior tendon rupture
Cerebrovascular accident
Lumbar spine radiculopathy
Hereditary sensorimotor neuropathy
Leprosy
Poliomyelitis
Cerebral palsy (spastic)
NONOPERATIVE MANAGEMENT
Bracing with an ankle-foot orthosis (AFO)
Requires a fixed AFO in flaccid paralysis
May be a flexible AFO with common peroneal palsy
Requires plantarflexion stop
Equinus contracture may need to be corrected to facilitate brace wear.
Achilles stretching
Botulinum toxin injection
Tendo Achilles lengthening (TAL)
Varus deformity
If flexible may be corrected with bracing
If fixed, bracing is difficult.
SURGICAL MANAGEMENT
Preoperative Planning
The surgeon must confirm that motor function will not recover before proceeding with tendon transfer.
Serial clinical examination
Serial electrodiagnostic studies (at least one compared to baseline)
The surgeon must determine what motor function persists:
Tibial nerve
PTT (inversion)
Gastrocnemius-soleus (plantarflexion)
None (flaccid paralysis)
The surgeon must evaluate for equinus contracture.
The surgeon should be prepared to perform TAL if necessary (see TECH FIG 1A-D).
Flexible versus fixed deformities
Flexible deformity typically corrects with tendon transfer alone.
Fixed deformity
May require capsular release or even arthrodesis
Toe contractures
Although claw toe deformity may not be evident with the ankle plantarflexed, once the deformity is corrected, toe contractures may become obvious.
Dorsiflexing the ankle will put the contracted flexor hallucis and digitorum on stretch, thereby revealing the toe contractures.
The surgeon should be prepared to address toe contractures as part of the procedure.
Tendon transfer anchoring
We routinely use interference screws to anchor tendon transfers to bone.
Need to have an anchoring system available
Alternatively, anchoring to existing distal tendon or existing soft tissues in the foot may be possible.
In our experience, anesthesia should maintain complete muscle relaxation and paralysis during the procedure; otherwise, the success of the tendon transfer may be compromised.
At the conclusion of the procedure, we often perform botulinum toxin injections into the gastrocnemius-soleus complex to further protect the tendon transfer postoperatively.
Positioning
Supine
If the PTT will be transferred through the IOM or if a peroneal tendon will be used for correction of flaccid paralysis, we routinely place a bolster under the ipsilateral hip to afford optimal lateral exposure. Once the lateral tendon is harvested or the PTT transferred through the IOM, the bolster may be removed.
We routinely use a thigh tourniquet.
Approach
Multiple relatively small incisions are needed; extensile exposures are unnecessary.
PTT harvest
Medial harvest over navicular
Posteromedial tibia at musculotendinous junction of PTT
PTT transfer through the IOM
Incision over distal IOM
Incision over dorsolateral foot
PTT transfer anterior to tibia
Incision over central midfoot
Bridle procedure
Same PTT harvest
PTT transfer through IOM with incision directly anterior over distal tibia; may be extended to dorsal foot. Alternatively, separate small incision over centrodorsal midfoot.
Lateral incisions: incision over musculotendinous junction of peroneus longus and another incision over lateral cuboid where peroneus longus courses around cuboid
TECHNIQUES
▪ Achilles Lengthening
Indications
Not always necessary but typically required when foot drop occurs
Without active dorsiflexion, the gastrocnemius-soleus’ antagonist is lost, often leading to an Achilles contracture.
Occasionally, patients maintain an active stretching program, thereby avoiding an Achilles contracture.
Weakening of the gastrocnemius-soleus complex may be beneficial because a transfer of a healthy muscle-tendon unit is subject to an automatic one-grade loss of power (5/5 manual muscle testing drops to 4/5 with transfer).
Occasionally, we use botulinum toxin in the gastrocnemius-soleus complex when performing a PTT transfer for foot drop.

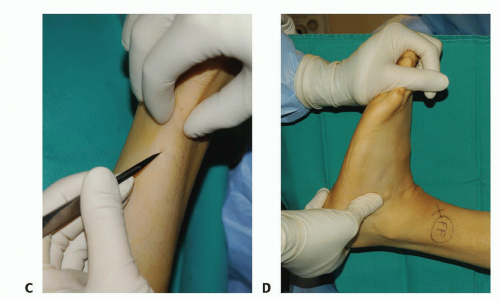
TECH FIG 1 • TAL. A. Equinus with knee in flexion and extension suggests tight gastrocnemius and soleus. B. Initial Achilles hemisection. (continued)
Technique
Determined by the Silfverskiöld test
Equinus contracture with the knee in extension and flexion (TECH FIG 1A)
Triple hemisection (Hoke procedure) because both the gastrocnemius and soleus are contracted (TECH FIG 1B-D)
Equinus contracture only with the knee in extension: gastrocnemius-soleus recession (Strayer procedure) because only the gastrocnemius is contracted
Posterior Tibial Tendon Transfer through the Interosseous Membrane
Advantages
PTT in direct line from its muscle through the IOM to the lateral cuneiform (our preferred site for tendon anchoring)
Anchor point slightly lateral of midline to promote dorsiflexion and eversion
Disadvantage
PTT may be constricted and stenosed within narrow window created in distal IOM.
Posterior Tibial Tendon Harvest
Make a 4-cm longitudinal incision over the medial navicular and PTT on the medial foot.
Open the PTT sheath to expose the tendon.
Release the PTT insertion on the medial navicular.
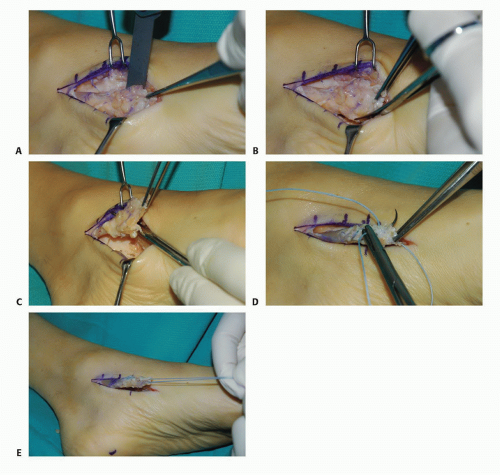
Alternatively, use a chisel to elevate some medial navicular bone with the PTT release from the medial navicular (may allow for another centimeter of tendon for transfer) (TECH FIG 2A).
Isolate the PTT attachment on the medial navicular and the tendon fibers that begin to course to the plantar midfoot (TECH FIG 2B).
With the PTT fibers isolated, transect them to release the PTT distally.
Be sure to fully isolate the PTT fibers; the medial plantar nerve and the plantar medial complex of veins is in close proximity.
Accidentally transecting the nerve leads to loss of sensation in the plantar medial forefoot.
Violating the veins may make it difficult to achieve satisfactory hemostasis, as these veins may then retract under the foot.
Thin the distal stump of the PTT to be transferred to facilitate its transfer into an osseous tunnel that will be created in the foot (TECH FIG 2C).
Place tag sutures in the distal PTT (TECH FIG 2D,E).
Make a more proximal medial incision at the PTT musculotendinous junction on the posterior tibia.
A 3-cm incision (TECH FIG 2F)
Flexor digitorum tendon is usually encountered first.
Deep to the flexor digitorum longus, directly on the posteromedial tibia, the PTT is identified.
Place a blunt retractor around the PTT through this more proximal wound to isolate it.
Mobilize the distal PTT.
Alternate tension on the proximal tendon through the proximal wound and the distal tag sutures (TECH FIG 2G), then apply tension proximally only.
This may not work.
The medial incision may need to be extended proximally to allow access to the posterior medial malleolus, a common location where the tendon may bind.
Once mobilized, the distal aspect of the PTT may be transferred to the proximal wound (TECH FIG 2H).
Tendon will desiccate rapidly, so we keep it tucked in the proximal medial wound.
Posterior Tibial Tendon Transfer through the Interosseous Membrane
Lateral incision on anterior aspect of distal fibula, at distal tibiofibular syndesmosis
Careful exposure of anterior IOM
Elevate the anterior compartment soft tissues.
A branch of the peroneal artery courses on the anterior IOM and is at risk.
Create a generous window in the distal IOM (TECH FIG 3A).
From tibia to fibula
About 3 to 4 cm long
Pass a tonsil clamp through the IOM directly on the posterior aspect of the tibia to exit in the proximal medial wound (TECH FIG 3B).
The posterior neurovascular structures (tibial nerve and posterior tibial artery) are at risk, so be sure the clamp is directly on the posterior tibia.
Use the tonsil clamp to grasp the tag sutures of the PTT (TECH FIG 3C).
Pull the tag sutures and PTT from the medial wound to the lateral wound, keeping the tendon directly on the posterior aspect of the tibia (TECH FIG 3D,E).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree