Meniscoplasty for Discoid Lateral Meniscus
Jay C. Albright
DEFINITION
A discoid meniscus is abnormal in both thickness and amount of covering or interposition of the compartment or plateau.
Over 99% of cases occur on the lateral side of the knee, with an overall incidence of 1% to 15% of the general population.
Ten percent of children found to have a discoid meniscus will have it bilaterally.
ANATOMY
Three types of discoid meniscus are described: complete (covering entire compartment), incomplete (on partial compartment covering), and Wrisberg (complete or incomplete compartment covering with no peripheral attachments).5
Wrisberg type is by definition unstable, allowing displacement, popping, and locking as well.
PATHOGENESIS
It arises either congenitally or through abnormal development. No cases have been found in autopsies of fetal deaths or stillborns.
NATURAL HISTORY
Discoid menisci have frequently been found at autopsy in elderly, reportedly asymptomatic people.
Frequently, it is an incidental finding.
Symptoms typically present in the late first or early second decade of life but may occur at any age.6
Symptoms are pain with or without loss of motion.
PATIENT HISTORY AND PHYSICAL FINDINGS
The common presentation is a young child (younger than 10 years) with a catch or popping of the lateral side of the knee with motion, with or without pain.
Some patients describe true mechanical locking symptoms.
The patient may present with painful or painless loss of motion.
The clinical examination may show a hypermobile lateral meniscus with palpable, audible, and frequently visual meniscal instability.
Effusion is a common finding. Objective signs of swelling with or without activity indicate irritation of the joint and possible tearing.
Loss of extension and joint line tenderness are also common.4
A discoid meniscus with a tear or instability will click or pop and may be uncomfortable. The results of the McMurray test will help with diagnosis.
Positive: pain and a pop or click
Negative: no pain and no pop or click
Equivocal: pop or click or pain without the other
Significant mobility of the lateral meniscus, although not uncommon, normally may indicate a discoid meniscus.
In children, varus instability may be due to accommodation of the large discoid lateral meniscus. Collateral ligament test results are important.
Normal: symmetric to the opposite side
Mild: 1 to 3 mm of increased laxity from the opposite side
IMAGING AND OTHER DIAGNOSTIC STUDIES
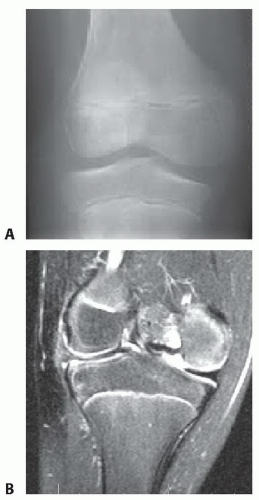
Radiographs may show flattening or sloping of the lateral femoral condyle, with widening of the lateral compartment compared to the medial compartment (FIG 1A).
Magnetic resonance imaging (MRI) will show the discoid meniscus the best (FIG 1B).
A discoid meniscus will be thicker and wider than a normal meniscus.
Frequently, signal change is present in the center of the discoid meniscus; this could represent a tear or degenerative tissue.1
There should be no more than three consecutive 3-mm cuts of the body of a meniscus on the sagittal view before
it is separated into an anterior and posterior horn. Coronal cuts may also show a wide, thickened meniscus (more than 12 to 15 mm).
DIFFERENTIAL DIAGNOSIS
Meniscal cyst
Tear in a normal meniscus
Anterior cruciate ligament tear
Hypermobile lateral meniscus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree