Master Techniques in Digital Arthrodesis
Keywords
• Digital arthrodesis • Digital fusion • Interphalangeal joint arthrodesis • Interphalangeal intramedullary implant
Historical background
In 1910, Soule1 first described the intentional arthrodesis of the proximal interphalangeal joint (PIPJ). Further advances have allowed for increased stability of digital arthrodesis procedures. For example, in 1931, Higgs2 advocated fusion using a spike-and-hole method. Young3 developed a similar peg-in-hole configuration, although he remodeled the proximal phalanx into a truncated cone shape. In 1940, Taylor4 was credited with the first use of Kirschner wire (K-wire) intramedullary fixation in hammer toe surgery. To prevent proximal migration of the K-wire, Selig5 further suggested that the hardware be bent at its distal margin, significantly improving the reliability of this form of fixation. More recent innovations include absorbable fixation and intramedullary digital implants.
History and physical examination
Patients complaining of digital deformities may report varying degrees of symptoms. Dorsal pain may be caused by pressure from footwear, which leads to callosities, whereas pain at the distal end of the toe may be secondary to contracture and the resultant shift of pressure from the more plantar padded metatarsal heads to the toe.6 Patients tend to report a history of digital deformity since birth or early childhood. Patients may relate that the extent of deformity has reached an end point or may note continued progression of the deformity. Patients commonly complain of difficulty fitting into shoes because of the severity of digital deformity. Usually the pain is exacerbated by pressure from footwear. Nonunion phalangeal fracture may be a cause of digital deformity, but this is significantly less common than congenital deformities acquired over the years.6
The sensory status of a foot must be evaluated as well. An impaired sensory status can indicate a systemic disease, such as diabetes, peripheral neuropathy, or lumbar disk disease. It is also important to differentiate MPJ pain from an interdigital neuroma of the adjacent intermetatarsal space.7,8 Preoperative documentation of sensation is important because surgical dissection can diminish postoperative sensation.
A thorough biomechanical examination should also be performed. Muscle imbalance between intrinsic and extrinsic muscles of the foot usually involves multiple toes with either rigid or flexible deformities and is often associated with cavus foot with or without contracted Achilles tendon. A painful bursa may develop at the PIPJ as a result of elevated contracture of the toe. When deformity becomes rigid, the plantar fat pad is pulled distally, causing pressure callus formation in the submetatarsal area.9 The plantar aspect of the foot should be examined for development of intractable plantar keratoses that can develop in association with contractures of the lesser toes, the result of a buckling effect of the digits. Calluses can develop pain beneath the tip of the toe or a lesser metatarsal head.10,11 The individual digits should also be examined for callosities on the medial and lateral aspects, as well as over the IPJ and at the tip of the toe. The rigidity of the toe contractures, the position of the metatarsal, and Achilles tendon tightness should all be analyzed. Tightness of the flexor digitorum longus tendon must also be assessed. It is important to evaluate these deformities while the patient is both seated and weight bearing.
Preoperatively, it is also important to determine whether there is sufficient space to accommodate the involved toe after reduction to a normal position. The Kelikian push-up test is important in determining the appropriate procedure. Performance of the push-up test loads the metatarsals plantarly to mimic the weight-bearing position of the patient’s foot. This test should be done preoperatively to determine the extent of contracture in the digit as well as intraoperatively to determine if further release of soft tissue or osteotomy is needed to relieve the contracture.12 If a patient has a concomitant hallux valgus deformity that has diminished the interval between the first and third toes, adequate space must be obtained for the corrected lesser toe, otherwise the deformity can recur.13 A hallux valgus repair may be necessary to obtain sufficient space between the first and third toes to realign the second toe successfully. At times, the adjacent lesser toes can drift into medial or lateral deviation, again diminishing the interval that the corrected toe should occupy. These toes may need to be corrected to afford the corrected hammer toe adequate space.
Etiology/definition
Digital deformities are generally defined based on the level of contracture. Lesser hammer toes present as a deformity primarily in the sagittal plane, with plantar flexion of the PIPJ and dorsiflexion of the MPJ. With such deformity, the middle and distal phalanges become flexed on the proximal phalanx.14 The causes of hammer toe deformity include muscle imbalance, Charcot-Marie-Tooth disease, Friedreich ataxia, cerebral palsy, myelodysplasia, multiple sclerosis, and degenerative disk disease. Such deformities may also be associated with neuropathy secondary to diabetes mellitus and Hansen disease.15 Progressive disease states of rheumatoid, psoriatic, and other inflammatory arthritides can also lead to hammer toe deformity.
Claw toe is a sagittal plane deformity with dorsiflexion of the MPJ and plantar flexion of the distal IPJ and PIPJ.14 The cause of claw toe deformity is similar to that of hammer toe, including neuromuscular disease, arthritis, and metabolic disease.
Mallet toe is a sagittal plane deformity with plantar flexion of the distal IPJ.1 The cause of mallet toe is largely unknown, although deformity has been related to recurrent pressure on the tip of the digit secondary to shoe wear. Such deformity may be associated with trauma or inflammatory arthritis or may present iatrogenically following hammer toe repair. Mallet toe is more common in women (with 84% predominance),16 although equal frequency is observed in the second, third, and fourth toes.10,16–21 In pediatrics, the flexor hallucis longus tendon is sometimes contracted, causing flexion at the distal IPJ. This condition is termed curly toe.22–26
Flexor stabilization is the most common mechanism of deformity. This deformity occurs in a pronated foot type during the late-stance phase of gait. Common causes of flatfoot deformity include forefoot varus, equinus, calcaneal valgus, torsional abnormalities, muscle imbalances, ligament laxity, and neuromuscular disease. Early and long firing of flexor muscles occurs in an attempt to stabilize a pronated mobile forefoot. In turn, increased pull of the long flexor muscles occurs as they gain mechanical advantage over intrinsic muscles such as the interossei.9,12,14,27 Hammer toe deformities develop when intrinsic muscles are not able to counter these deforming forces.
Extensor substitution is a swing phase condition that develops secondary to weak anterior group muscles. During this phase in the gait cycle, anterior group muscles fire to dorsiflex the foot at the ankle. Deformity develops when extensor muscles in the anterior compartment gain a mechanical advantage over intrinsic muscles such as the lumbricals. Extensor substitution can occur secondary to ankle equinus, weak lumbricals, or spasticity of the extensor digitorum longus. On physical examination, marked dorsiflexion of the MPJ is often noted, although this may straighten with weight bearing. The extensor tendons and the metatarsal heads are prominent dorsally and plantarly, respectively.9,12,14,27 Normally the digits dorsiflex approximately 6° at the MPJs, but with extensor substitution there is more dorsiflexion of the proximal phalanges. Although the digits appear rectus on weight bearing, during swing they curl up because of extensor substitution.
Flexor substitution is a stance phase deformity occurring in a supinated foot type (Fig. 1). In this situation, the triceps surae is weak. This deficit may develop secondary to overlengthening of the Achilles tendon or may be congenital. To compensate the posterior deep muscles and the peronei, the physician must attempt to produce heel off in place of the weakened triceps. The flexors in turn gain mechanical advantage over the interossei muscles. On physical examination, a calcaneal gait and supinated high arch foot type are commonly seen with this deformity.12
Radiographic analysis
Radiographic examination is necessary to evaluate the magnitude of digital osseous deformity. During the evaluation of the patient, weight-bearing radiographs are highly recommended. These studies help in determining the extent and location of digital contractures as well as MPJ deformity and subluxation. Associated deformities such as hallux valgus or other contributing pathology such as cavus foot or metatarsus adductus should be evaluated. Radiographic evaluation may also show the presence or absence of arthritic changes, particularly those changes associated with systemic processes such as rheumatoid arthritis and inflammatory diseases. Bone scans, magnetic resonance imaging, or computed tomographic scans are rarely needed in the diagnosis of a lesser digital deformity.6
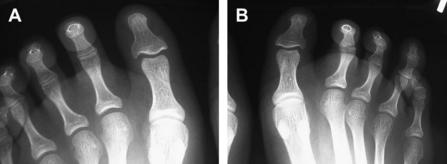
On an anteroposterior view, a severe hammer toe deformity can have the appearance of a gun barrel deformity (Fig. 2) when the proximal phalanx is seen end on. Assessment of the IPJs is difficult on the anteroposterior view. Attenuation of the metatarsophalangeal space can indicate subluxation. Overlap of the base of the proximal phalanx in relation to the metatarsal head indicates dislocation of the MPJ. Subchondral erosion, flattening of the articular surfaces, or Freiberg infraction indicate the need for further radiographic or laboratory evaluation.12
A lateral view may be helpful to assess the magnitude of contracture of the IPJs. Stress radiographs may also be considered to evaluate subluxability of the MPJ.12
Indications for fusion
IPJ fusion should be considered in patients with the following indications:
Fusion may also be considered to address digital deformity in the transverse plane. If the MPJ is subluxated or dislocated, this deformity should be corrected simultaneously with the hammer toe correction.15,28–30 Fusion provides more reliable realignment of multiplane digital deformities.
When inadequate flexion strength at the MPJ is noted, digital arthrodesis should be considered. Digital arthrodesis acts to strengthen the force of the long flexor tendon. This force is then transmitted to the MPJ, resulting in improved plantar flexion of the joint.2 In this case, arthrodesis will likely yield more successful long-term results.
Procedure
Once the cause has been determined, the surgeon determines if surgical correction is appropriate. The steps in the procedure to correct a hammer toe include resection of the head of the proximal phalanx, extensor digitorum brevis tenotomy, extensor digitorum longus lengthening, first MPJ capsulotomy, and PIPJ arthrodesis. It is imperative that the surgeon analyzes the reduction of the deformity after each step in the procedure by performing the Kelikian push-up test in which pressure is applied to the plantar metatarsal area. If the deformity is reduced using this method, the surgeon may opt for closure at this point in the procedure. However, if the deformity is still evident, a digital arthrodesis is then performed.12
General anatomy/joint exposure
Once the patient is under intravenous sedation and local anesthesia has been administered, the surgeon’s attention is directed toward the deformed digit. A #15 blade is used to make a linear longitudinal incision from just proximal to the MPJ to slightly distal to the PIPJ. The incision is made through the epidermal and dermal layer of tissue, above the level of the extensor tendon, taking care not to disrupt the tendon. A lazy “S” incision may be chosen to minimize skin contracture at the incision site. The incision is then deepened through subcutaneous tissue, avoiding any neurovascular structures that may be encountered.12
To allow exposure to the head of the proximal phalanx, the extensor digitorum longus tendon may be retracted, incised transversely, or lengthened via a Z-plasty. Next, the collateral ligaments are excised, and excess soft tissue from the distal phalanx is removed. The head of the proximal phalanx is then resected at an appropriate level using a sagittal saw or bone cutter. The rough bone edges are then smoothed with a rongeur or rasp. The surgeon must perform a Kelikian push-up test at this time to determine if extensor digitorum brevis tenotomy is necessary. The tendon can be identified just proximal to the MPJ, and a small stab incision is made just medial or lateral to the tendon with a #15 blade. The blade is then placed transversely, directly plantar to the extensor tendon. Next, the blade is turned to face dorsally and the digit is plantar flexed, causing the blade to incise the tendon. The Kelikian push-up test is performed at this time to determine if extensor digitorum longus lengthening is necessary. If adequate correction has not been established at this time, the extensor tendon lengthening is performed via a Z-plasty technique. The tendon will be reapproximated after arthrodesis is completed if that step is deemed appropriate.12
If adequate correction has not been achieved following completion of these steps, a PIPJ arthrodesis is performed. If it has not already been done, the extensor digitorum longus is transected transversely or in a “Z” manner, allowing full exposure of the PIPJ. The distal aspect of the proximal phalanx and proximal aspect of the middle phalanx are cleared of any remaining soft tissue attachments. The cartilage of each articular surface is then resected perpendicular to the long axis of each bone to ensure the toe will be in proper alignment once fixated. Appropriate fixation is then done, followed by suturing of the extensor digitorum longus and closure of subcutaneous tissue and, finally, the skin. The toe is then bandaged in the appropriate sterile manner.12
Arthrodesis techniques
The end-to-end arthrodesis procedure, described in detail earlier, is the most commonly performed digital arthrodesis procedure because it results in less digital shortening and is easy to perform.12 However, the procedure does have its drawbacks. For instance, there is more potential for the distal fragment to rotate in the frontal plane, which may lead to the development of delayed union or nonunion.
Another option is the peg-in-hole procedure, which uses the distal cortex and central cancellous bone of the proximal phalanx to form a peg. This peg portion is then inserted into a hole created by drilling into the intermedullary shaft of the proximal aspect of the middle phalanx, thus preventing the possibility of the distal fragment rotating in the frontal plane. This procedure is technically more difficult and time intensive than the end-to-end procedure. It may also result in more digital shortening than other methods of arthrodesis. There is always the potential for the peg portion to fracture, which may lead to delayed union or nonunion. The advantages, however, are that no internal fixation is required and high rates of fusion are obtained.11,31
Digital “V” arthrodesis and box joint arthrodesis are 2 other surgical options in treating flexion deformities of the digits. In the digital “V” arthrodesis, the surgeon makes a “V” cut distally in the articular surfaces of the proximal and distal phalanges.30 The bones can then be fixated with a K-wire. Box joint arthrodesis is performed by resecting the inferior aspect of the head of the proximal phalanx and the superior aspect of the base of the middle phalanx. The bones are then fixated appropriately. These procedures are generally performed based on the comfort level and success rates of the surgeon because the clinical complications are similar.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree