Ankle Arthrodesis
Keywords
• Ankle • Arthrodesis • Fusion • Tibiotalocalcaneal
Ankle arthrodesis was first described by Albert in 1879 as part of a knee and ankle fusion in a child suffering from palsy.1 The early 1900s saw the use of arthrodesis in the ankle and foot for stabilization of paralysis secondary to polio. Then, in the 1950s, Charnely introduced an external fixator device for compression arthrodesis. His method was the first to use surgical hardware to place a compressive force across the arthrodesis site, thereby improving surgical outcomes. However, Charnely used a down to bone transverse incision at the level of the ankle joint, resulting in transection of tendons, nerves, and vascular structures with resulting sequelae.2
Indications
Painful arthrosis of the ankle joint with or without concurrent deformity is the primary indication for arthrodesis.3,4 The typical candidate presents with a history of trauma, often involving articular damage to the ankle joint.5 Specifically crushing injuries, comminuted fractures, and ankle sprains involving condylar cartilage injury are present. Other causes for ankle degeneration indicating arthrodesis may include failed implant, neoplasms, avascular necrosis, infection, Charcot, and congenital deformity.6–9 Systemic arthritides, such as rheumatoid, show high correlations with ankle and subtalar deformities and degeneration. Michelson and colleagues10 showed most rheumatoid patients experienced foot and ankle arthritis, 20% of whom have radiographic changes. Saltzman and colleagues5 found 12% of patients in their study had arthritic ankles secondary to rheumatoid.
Contraindications
When considering ankle arthrodesis, adequate soft tissue quality is of the utmost importance. Comorbidities including peripheral vascular disease, lymphedema, and venous stasis may prevent a patient from tolerating more involved tissue dissection and put the patient as risk for infection and amputation.9,11,12 Smoking tobacco merits consideration because it has been shown to have a negative impact on bone fusion.13 Complex lower extremity deformity with recurrence or progression may result in an unfavorable outcome. Other factors such as the patient’s age, activity, quality of life, and surgical risk versus benefit need to be taken into consideration.
Preoperative assessment
The initial clinical evaluation should determine any previous traumatic events, including sprains or fracture, because these are the most common cause of ankle arthritis.2–4 Additional historical inquiry should screen for systemic illness including obesity, osteoporosis, gout, arthritis, infection, diabetes mellitus, neuropathy, and peripheral vascular disease. The patient’s medications should be carefully reviewed because immunosuppressives are a standard therapy for inflammatory arthritides. Physical examination follows standard neurovascular testing and palpation for tender locations indicating concurrent disease. Biomechanical examination follows standard protocol with walking and static evaluation and special attention paid to the alignment of the rearfoot. This assessment should be a bilateral lower extremity examination, taking into account any existing deformity that may prevent a plantigrade foot. Sometimes the patient has an extremity or postural deformity that, on placing the ankle into normal alignment, inhibits a pain-free functional surgical outcome. The ankle may be put into a more neutral position for a forefoot valgus or greater than 5° valgus to compensate for a forefoot varus.14
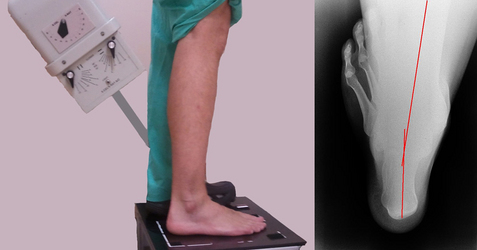
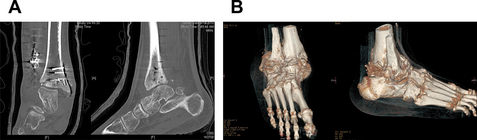
Plain film radiographs may or may not show findings consistent with the clinical pain of which the patient is complaining.15 However, often osteophytic formation, decreased joint space, and asymmetrical joint contour are hallmarks of an arthritic ankle.16 In addition to the standard anterior posterior, mortise, and lateral views, long leg axial calcaneal views allow assessment of the hindfoot deformity (Fig. 1).17 When considering surgical fusion one should seek out adjunctive imaging in the form of magnetic resonance imaging or computed tomography. These modalities allow greater examination of deformity, bone density, congruity, and retained hardware.18 An invaluable addition to the standard computed tomography is volume rendering and shaded surface display three-dimensional reconstructions (Fig. 2). These technologies provide orientation of bone to overlying soft tissue and isolation of individual osseous structures, allowing greater visualization in significant deformities of the ankle joint and hindfoot and aiding in preoperative planning.19,20
Surgical technique
Transfibular Approach Using Tripod Screw Technique
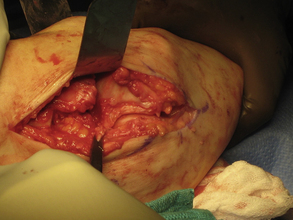
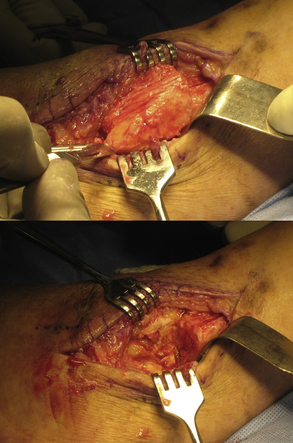
The patient is placed on the operative table in supine position with application of a thigh tourniquet and hip bump to align the knee and lower extremity. The lateral incision is made approximately 7 cm proximal to the ankle joint over the lateral fibula and is carried distally over the fibula, curving gently over the lateral aspect of the talus to a point approximately 1 cm distal to the tip of the fibula (Fig. 3). Dissection is then carried down through subcutaneous tissue to the level of the fibula; care should be taken to avoid the sural nerve and perforating peroneal arteries.21 Deep dissection is made over the anterior ankle joint; the anterior tendon and neurovascular structures should be protected using a malleable retractor (Fig. 4). The surgeon now has the choice of either a transverse or an oblique osteotomy of the fibula. The oblique osteotomy allows repair of the fibula, whereas a transverse osteotomy may be used if a fibular onlay graft is desired.14,22 The fibula is then reflected distally or removed (if removed it is transected longitudinally for use as an onlay graft) (Fig. 5). Depending on the desired positioning and deformity, the joint surfaces may be prepared as is, leaving the existing anatomic relationship, or planed with a saw to achieve the desired positioning. Cartilage is typically removed with a power burr and osteotome down to the level of bleeding, cancellous bone. Care must be taken to curette or osteotome any existing subchondral cystic structures. The medial malleolus cartilage can be removed via a curette through the lateral incision or a medial incision can be performed.21,23–25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree