Tarsometatarsal (Lisfranc) Joint Dislocation
Lawrence A. DiDomenico
Dawn Y. Stein
Fracture dislocations of the tarsal-metatarsal (Lisfranc injuries) can be subtle and may be missed in both initial and later evaluation of midfoot injuries. Injuries to the Lisfranc complex can be difficult to diagnose and may be overlooked in patients who have multiple injuries (polytrauma, i.e., motor vehicle accident) or in patients who experience a simple injury such as a sprain. These injuries encompass a wide spectrum from simple injuries to grossly unstable dislocations. They can cause severe long-term morbidity if not appropriately treated. Dislocations at the tarsometatarsal joint are an uncommon injury, comprising only 0.2% of all fractures (1,2). However, in more recent literature, it has been reported as common as 7.9% of all fractures (3). It is the author’s experience that the subtle injuries occur more commonly than reported due to the difficulty of making the appropriate diagnosis. It is not uncommon for foot and ankle surgeons to see patients with a Lisfranc injury days or sometimes weeks later following a visit to the emergency room with an unrecognized injury. Although they are not that common in the general population, they are the second most common athletic foot injury, occurring in 4% of football players per year (4). Twenty (5,6) to thirty-five (3) percent of these injuries are unrecognized or misdiagnosed. Therefore, a high index of suspicion is needed when diagnosing this injury (7).
The injury was previously reported to have a high incidence in equestrian riders whose foot would get caught in the stirrup when falling off. The development of narrow-toe boots prevented the foot from being caught in the stirrup (8). Highenergy traumatic injuries, such as in motor vehicle accidents, have been reported to account for the majority of the injuries, resulting in about one-half to two-thirds (9,10 and 11) of them. Myerson reported the injury in several windsurfing athletes and more recently in a high-velocity sledding injury by Benejam and Potaczek (12). Lisfranc injuries may also be a result of lowvelocity trauma such as a stumble or a fall (12,13).
The Lisfranc joint bears its name from Jacques Lisfranc (1790 to 1847), a French surgeon in Napoleon’s army, who performed amputations through the tarsometatarsal joint to treat gangrenous injuries in the foot (14). However, he never described the fracture or dislocation. Lisfranc injury was first described by Quenu and Juss in 1909 who classified the injury based on the deforming force of the foot. Hardcastle et al in 1982 further modified the classification system, followed by Myerson et al in 1986, describing the radiographic injury pattern at the Lisfranc joint.
FUNCTIONAL ANATOMY
The tarsometatarsal joints attach the forefoot to the midfoot and is a weight-bearing structure with numerous ligaments and tendon attachments. Typically, the forefoot is mobile relative to the stable midfoot. The midfoot bones function as a single unit with minimal motion between the individual bones. In nonpathologic feet, these joints are stable and help shape the longitudinal medial arch. The three medial tarsometatarsal joints are very stable. The first tarsometatarsal joint is a deep joint that measures approximately 3 cm in depth. These joints provide varying degrees of dorsal and plantar motion. Based on its shape, size, and strong peripheral ligaments, the first tarsometatarsal joint should provide stability. Additionally, stability is gained through the dynamic tension of its tendon attachments of the peroneal longus and anterior tibial tendon. The second and third tarsometatarsal joints are essentially immobile in normal feet. These joints are stabilized by there osseous configuration and strong plantar intermetatarsal ligaments. The cuboid, which articulates with the fourth and fifth metatarsals, is much more mobile. The fourth and fifth tarsometatarsal joints have immense gliding motion to allow for adjustments to uneven surfaces and align the forefoot with hind foot. Essentially, the fourth and fifth tarsometatarsal joints are mobile adapters (Fig. 106.1).
BONY ANATOMY
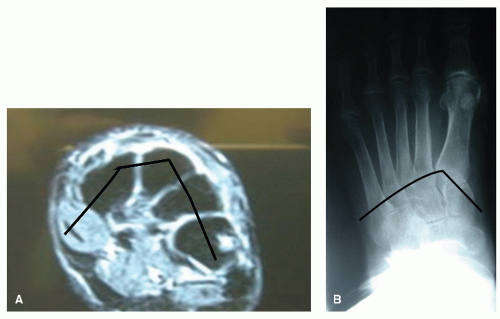
The osseous structures consist of the metatarsals, cuneiforms, and the cuboid bone. Two arches are formed on the frontal and transverse planes. The metatarsal and cuneiforms are asymmetric in size and shape. The second and third cuneiforms are situated more dorsally than plantarly; they are wedge shaped, with the base of the wedges situated dorsally and the apex plantarly, which accounts for the naturally occurring intrinsic support (Fig. 106.2A). The second metatarsal is recessed between the adjacent metatarsal-cuneiform joints, contributing to a keystone effect (Fig. 106.2B). The intercuneiform joints are perpendicular to the transverse arch, which accounts for most of the intrinsic support of the arch (8).
LIGAMENTOUS ANATOMY
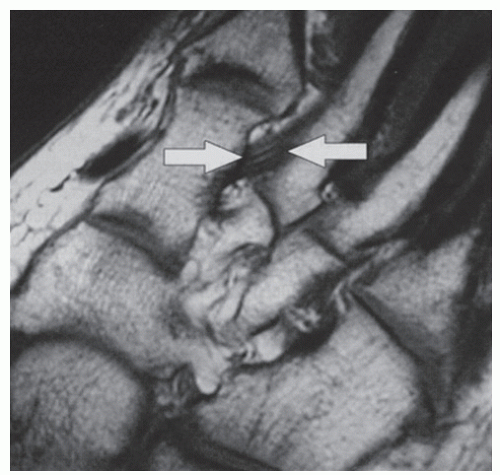
Each metatarsal base is connected by a strong transverse, oblique, and interosseous ligament, except at the base of the first and second metatarsal where none exists. Instead, an extremely strong, thick ligament extends from the medial base of the second metatarsal obliquely into the medial cuneiform, which has been previously noted as the Lisfranc ligament (15,16) (Fig. 106.3). The Lisfranc ligament is roughly 1.5 cm × 0.5 cm thick, consisting of a longitudinal and oblique portion in 22% of cases (17). The ligaments are stronger plantarly than dorsally (7). The plantar fascia, tendons, and muscles also support the joints on the plantar aspect.
DIAGNOSIS
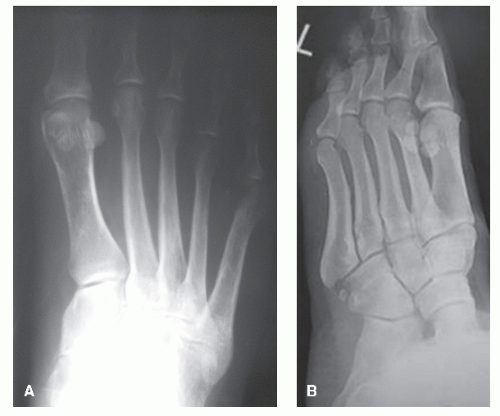
Many injuries go unrecognized as many appear to reduce spontaneously, although on closer examination they remain displaced. As a result, many patients are misdiagnosed with a foot sprain. Initially, plain radiographs are taken (Fig. 106.4A and B). Significant fracture, subluxation, and/or dislocation at the tarsometatarsal joints can be seen on plain radiographs. In cases with distinct injury, it is important to review the surrounding anatomy to evaluate for further injury (Fig. 106.4C). Although many injuries go undiagnosed or overlooked, a high index of suspicion is necessary to properly diagnose a patient with a Lisfranc injury. An individual may present with swelling and tenderness along the tarsometatarsal joints with additional instability. Weight-bearing radiographs can be difficult to obtain as most of these injuries will prevent patients from full weight-bearing. A stress test may be performed by grasping both the first and second metatarsals and performing both dorsiflexion and
plantarflexion motions. Also, performing simultaneous pronation and abduction of the midfoot and forefoot can reproduce symptoms. A positive test result is one that elicits pain with minimal stress (18). Harwood and Raikin (19) suggest maintaining the hindfoot in a position of inversion when performing the stress test to eliminate subtalar motion (Fig. 106.4D and E)
plantarflexion motions. Also, performing simultaneous pronation and abduction of the midfoot and forefoot can reproduce symptoms. A positive test result is one that elicits pain with minimal stress (18). Harwood and Raikin (19) suggest maintaining the hindfoot in a position of inversion when performing the stress test to eliminate subtalar motion (Fig. 106.4D and E)
DIAGNOSTIC STUDIES
Diagnostic tools are very helpful in the diagnosis of a Lisfranc injury. A study by Foster and Foster (20) in 1976 reviewed 200 normal radiographs and compared the findings with those diagnosed with a Lisfranc injury. Normal radiographic findings are alignment of the medial aspect of the base of the second metatarsal with the medial border of the intermediate cuneiform on the anterior-posterior view and, on the oblique view, medial border of the base of the fourth metatarsal aligned with the medial aspect of the cuboid (see Fig. 106.1). In addition, a space between the base of the first and second metatarsal bases may be normal; however, if there is a “step-off” at the base of the second metatarsal and intermediate cuneiform, there may be evidence of an injury. A distance between the first and second metatarsals greater than 2 mm is suggestive of injury (21). Myerson identified a “fleck sign” that can be seen at the medial
base of the second metatarsal or lateral base of the first metatarsal as an avulsion fracture (Fig. 106.5A), as seen in 90% of the 72-patient Lisfranc injury study (22). Other authors, such as Faciszewski, suggested that a diastasis of 2 to 5 mm between the bases of the first and second metatarsals, as seen on the AP radiographs, is consistent with injury. Also noted in subtle injuries of the Lisfranc joint was a flattening of the longitudinal arch, which could be identified on a lateral radiograph by observing the medial cuneiform at a more plantar attitude to the fifth metatarsal (23) (Fig. 106.5B). Lu suggests that a 1-mm diastasis between the first metatarsal and second metatarsal on CT image as well as an increase of more than 15 degrees in the tarsometatarsal angle results in a chronic Lisfranc joint failure (24).
base of the second metatarsal or lateral base of the first metatarsal as an avulsion fracture (Fig. 106.5A), as seen in 90% of the 72-patient Lisfranc injury study (22). Other authors, such as Faciszewski, suggested that a diastasis of 2 to 5 mm between the bases of the first and second metatarsals, as seen on the AP radiographs, is consistent with injury. Also noted in subtle injuries of the Lisfranc joint was a flattening of the longitudinal arch, which could be identified on a lateral radiograph by observing the medial cuneiform at a more plantar attitude to the fifth metatarsal (23) (Fig. 106.5B). Lu suggests that a 1-mm diastasis between the first metatarsal and second metatarsal on CT image as well as an increase of more than 15 degrees in the tarsometatarsal angle results in a chronic Lisfranc joint failure (24).
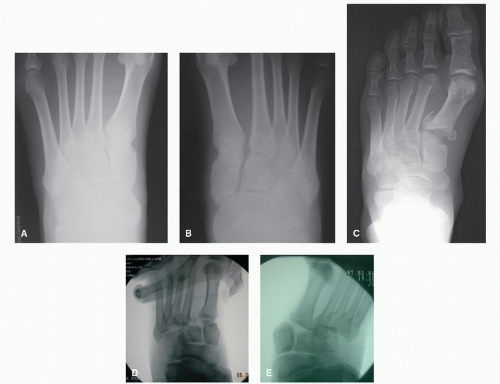 Figure 106.4 A,B: Bilateral weight-bearing radiographs demonstrating a small “fleck sign” on the right with a gapping noted at the intercuneiform and Lisfranc joint. C: AP radiograph demonstrating trauma to Lisfranc joint as well as the second and third metatarsal heads. D,E: Abduction stress radiographs demonstrating Lisfranc instability.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|